Office of Research & Development |
 |

VA Research Currents archive
October 15, 2015
Dr. Ronald Przygodzki is VA's director of genomic translation research. His team is looking at how to use data from the Million Veteran Program to advance research and improve Veterans' health care. (Photo by Robert Turtil)
In August, a VA patient in Dallas became the 400,000th enrollee in VA's Million Veteran Program (MVP).
Within the next few years, the program is expected to reach its goal and have DNA and health data from 1 million Veterans. Then what?
How will the Veterans Health Administration (VHA) use the information? How will VHA apply the research based on MVP data? Will this large-scale genomics effort truly change the health care Veterans receive?
Perhaps no one is pondering those questions more deeply than Dr. Ronald Przygodzki.
Przygodzki, a pathologist and genetics expert, has served in leadership positions in VA's Office of Research and Development since 2007. His newest title captures the thrust of his mission nowadays: director of genomic translation research.
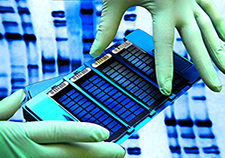
A VA technician handles a tray containing bar-coded DNA from research volunteers, along with more than a million micron-sized beads of lab-supplied DNA, each bead containing a different genetic variant. A special scanner is used to detect matches between the sets of DNA, thus determining which variants a patient or research volunteer has. (Photo by Jeff Bowen)
"We're trying to use genomic research to find new solutions and move those into Veterans' care," says Przygodzki.
Among other applications, he envisions using genomic data to help ward off illness and disability among returning Veterans. Agent Orange, Gulf War Illness, burn pits—past wars led to medical mysteries that have lingered on for years, in some cases decades. Przygodzki says genomics may be one tool for preventing similar scenarios in the future.
"We can use genomics to help find out what is going on with them as various conditions appear. One outcome might be advising the Department of Defense on health issues they might be able to address, to better protect troops and have them return home more intact."
Begun in 2011, MVP has become the largest database of its kind in the nation. The effort is now part of President Obama's Precision Medicine Initiative, announced earlier this year. The idea is to scale up the push nationwide to use patients' genetic information to tailor their medical care.
The approach is already in use in medicine to a certain extent—particularly with cancer. Genetic testing is even considered standard care—and covered by insurance—for a few cancers, such as non-small cell lung cancer, since there are proven therapies that target mutations known to drive those cancers.
The idea now—fueled by MVP and the White House's wider initiative—is to expand the approach across a much wider scope of health problems. One example is depression.
Przygodzki and colleagues are in the early planning stages of a pilot study, based on MVP data, that would look at how genetics can predict response to antidepressants. Genetic variants known generally as "pharma markers" reveal if a person is a slow or fast metabolizer of a drug. Emerging findings are increasingly catching the eye of psychiatrists and others who prescribe the drugs.
"Some people can take a pill once a day and get a dose that's adequate," says Przygodzki. "Others don't metabolize it until the drug starts accumulating in their system. Others, you give the drug, and it just passes through in a few hours—there's no drug left."
What might be the right antidepressant dose for one patient might send another into psychosis, due to an overdose.
Przygodzki says few mental health providers, in or outside VA, are taking advantage of the promise of genomics to boost outcomes for those on depression drugs. Part of the problem is providers' skepticism. They are used to adjusting dosage by trial and error—not by ordering DNA tests for their patients.
"The information is limited but available. But we in VA are not doing this on a large scale, nor is anyone else at this point," says Przygodzki. "They wonder if it's useful."
He describes the pilot he envisions:
"We have these people in MVP. We can find out if they have major depressive disorder, whether they've had any injury through drug, or failure of drug. We can get that data. We can set up a pilot with clinicians and see what they do. Do they use the information? Does it affect prescribing? Will it help in the therapy of these patients long-term? It would be a start."
Przygodzki stresses that genomics doesn't replace more conventional ways of diagnosing illness or deciding on treatment—it's just another tool.
By way of analogy, he says: "You can take a patient and squeeze his skin to see if he's well-hydrated—or you can go and do blood tests. Whichever one is appropriate. It all depends."
And even with a full panel of genomic information, or brain scans or any other newer tools, the skill and insight of the clinician remain vital, says Przygodzki.
"The genotype [a person's gene profile] is important, but it's not going to be the sole determinant of the diagnosis, or of treatment. You always have to have a clinician. Medicine is, as it always was, an art. It requires experience and judgment."
Also, sending blood samples out to a lab for genotyping comes at a cost. But there are ways to offset that cost, suggests Przygodzki.
One would be doing a one-time overall genetic analysis of a Veteran, ideally when he or she first enrolls in VA care. That way, the information could be available in a database as needed for different providers, regardless of what condition is being treated.
This would likely involve "exome sequencing." This is similar to whole-genome sequencing, in which the entirety of a person's DNA is described—every gene, every mutation. That process is dramatically cheaper today than it was even five years ago, and it's likely to get even cheaper in the next few years. But as of now, it' still upwards of $1,000 per person.
The exome represents only a small portion of the genome—less than 2 percent. But it's the part that codes for proteins, which, in rough terms, is DNA's business end. Of the genetic mutations known to cause disease, for example, more than 8 in 10 are found in the exome.
Sequencing the exome, instead of the whole genome, is cheaper and more cost-effective. MVP has already sent out some 25,000 DNA samples for whole exome sequencing. Przygodzki envisions this aspect of MVP being ramped up going forward.
"Doing individual lab tests costs money," he says. "That's part of the quandary. On the other hand, if we were to do exomes on all these people, and have that record ready, it's done once. And now we have a reference we can go back to."
Another cost-saver for VHA, says Przygodzki, would be having core genomics labs to service wide regions, or even the entire VA health system. A few such facilities already exist—in Little Rock and San Antonio, for example.
"With mental health, for example, if we set up a lab at one VA medical center, why would we need a second, or a third, or a ninth, or a 50th? It would be too costly to have this at every VA, and there would be too few tests of any given kind at one site." Rather, he says, "let's have it at only one or two sites, and have them be the experts in doing this. They can live and breathe it. They would be the VA center for it."
The business principle is the same as in even the simplest operations: "If you know how to make hot dogs and get down the process," says Przygodzki, "you can pump out hot dogs day and night. You don't want to have every facility making one hot dog."
Working out such economies of scale is only one of Przygodzki's challenges. Another key area related to his mission is informatics. He works closely with the team at the Massachusetts Veterans Epidemiology Research and Information Center (MAVERIC) who run the Genomic Information System for Integrated Science. The system ties together the huge and disparate pools of data in MVP, from different sources, that have to be linked.
For starters, there's the biospecimen—the actual bar-coded blood sample, which gets deep-frozen at minus 30 Celsius in the VA biorepository in Boston. Robots help process and retrieve the samples for investigators.
There are molecular data that emerge from the analyses done on these samples. What gene variants are present? Are there proteins expressed in abnormal amounts?
There are self-reported data that Veterans fill out in their surveys—including about their military experiences. Were they in combat? Exposed to blasts or chemicals?
There are also clinical data from VA electronic health records, and from other clinical databases in VA. Demographics, lab values, diagnoses—it all goes in the mix. (Names and other personal identifiers are omitted.)
An important related resource is the VA Informatics and Computing Infrastructure, which gives VA researchers access to VA data in a secure virtual workspace, with sophisticated tools for analysis and reporting.
Then there are data from non-VA sources such as the Centers for Medicare and Medicaid Services. Many VA patients also receive health care outside VA, and researchers want to look at this also.
Przygodzki says that to get "MVP rocking and rolling, we need to look at how these systems work together. We need to synch up the genomic data with the medical record data."
Earlier this year, VA funded a set of four studies—beta tests—designed to help work out some of these informatics issues. They'll focus on chronic illnesses like heart or kidney disease, but they'll also help iron out processes, especially when it comes to integrating various data sources, that will set the stage for future large-scale studies based on MVP.
Another frontier entails ethics more than technology. As of now, Veterans who enroll in MVP are not given back any results from their personal genomic analysis. The current system is not set up for that. Among other factors, MVP blood samples are generally not processed in CLIA-certified labs, which is a federal requirement whenever samples are used for diagnosis or treatment.
So MVP participants are not told, for example, if they have a genetic mutation that may increase the risk of a certain cancer, or Alzheimer's disease. By and large, Veterans who enroll do so for altruistic purposes—to help their fellow Veterans, future generations, others in general.
The process may change, though. Przygodzki is looking at what steps would be needed to start informing individual Veterans of their results. Based on past focus group findings, he believes most Veterans would in fact welcome such information.
"The Veterans believe we ought to be doing something with these samples to help others, as well as themselves," he says.
As researchers develop more genomic insights, Veterans' blood tests could yield concrete data to guide treatment. Those with diabetes, for instance, may learn they are good candidates for a certain new drug.
"If this is something that helps them be healthy, from an ethical standpoint we have to provide the information," says Przygodzki.
At the same time, some patients might not want to learn of certain types of results. Think about the Alzheimer's example: Some people might not care to learn that they are at especially high risk for the disease. Without a good treatment on the horizon, that information might cause anxiety and do more harm than good.
The key, says Przygodzki, will be giving patients a choice. That's the direction he wants VA's genomics program to go in: not just setting policy based on general findings from focus groups, but letting each patient decide what VA does with his or her information.
"You have to go the users, the customer base, and find out what they want. If a given person wants to find out, great. If not, that's also great. The free will aspect is important. We need to give Veterans options. By giving everyone a choice, we protect everybody."