Office of Research & Development |
 |
Many Veterans who rely on VA for their health care live in remote areas. Our nation's rural and highly rural Veteran population is large and dispersed. It is also racially, ethnically, and culturally diverse. Providing comprehensive, high-quality health care to these Veterans is a challenge.
VA's Office of Rural Health (ORH), created in 2007, strives to eliminate the barriers between rural Veterans and the services they have earned and deserve, thus improving Veterans' health and well-being by increasing access to care.
According to ORH, 4.7 million Veterans live in rural communities across the United States, and more than 2.8 million rural Veterans rely on VA for their health care—a significantly higher percentage than the 37% enrollment rate of urban Veterans. Veterans are more likely to live in rural areas than Americans who did not serve in the military. While 19% of Americans live in rural areas, almost a quarter of Veterans do.
More than half (56%) of rural Veterans enrolled in VA health care are 65 years old or older. In addition, 8% are women; 15% report being members of racial and ethnic minorities; and nearly 460,000 are Veterans of the recent conflicts in Iraq and Afghanistan. About 18% of rural Veterans have one or more service-related disabilities.
Rural Veterans have lower average household incomes than other Veterans (52% have annual incomes of less than $35,000); 27% do not access the internet at home; they often face long driving distances to access quality health care; and there are fewer health care providers and nurses per capita in rural areas.
VA’s Office of Connected Care works to bring digital technology to Veterans and health care professionals, extending access to care beyond the traditional office business. Connected Care focuses on improving health care through technology by engaging Veterans and care teams outside of traditional health care visits, including telehealth. By bringing together VA digital health technologies under one umbrella, Connected Care is enhancing health care coordination across VA and with community care providers as authorized under the VA MISSION Act of 2018, and supporting Veterans’ participation in their own care. The MISSION Act strengthens VA’s ability to deliver Veterans trusted, easy to access, high-quality care at VA facilities, virtually through telehealth, and through community care providers. Veterans need to be enrolled in VA health care to use community care benefits.
VA research is working with Connected Care by conducting studies that either point to the need, or test, connected care solutions and targeted interventions that improve access to care for rural and other Veterans. Researchers are working directly with the office and other VA organizations to identify research gaps and interventions that can address rural Veterans’ issues and the issues of other Veterans in accessing health care from VA and with authorized community care providers.
VA has recently launched a number of initiatives to expand and ensure access to high-quality health care for Veterans enrolled in the VA health care system who live in rural areas. VA researchers have been instrumental in these efforts by developing and evaluating new technologies, interventions, and models of care.
Veterans who live in remote areas of the country have faced challenges in accessing VA care.
While the MISSION Act will help address those challenges, VA researchers have focused on understanding these Veterans' health care needs and on developing and evaluating new initiatives to fill the gaps. Some VA studies focus specifically on Veterans in rural areas, while others have a broader focus but explore issues or possible solutions that are relevant to rural health care.
With support from the Office of Research and Development, a Collaborative Research to Enhance and Advance Transformation and Excellence (CREATE) group, Improving Rural Veterans' Access/Engagement in Evidence-Based Healthcare, is working with ORH and the Office of Mental Health and Suicide Prevention to ensure rural Veterans receive adequate levels of mental health care.
VA's Charleston Health Equity and Rural Outreach Innovation Center (HEROIC), one of the Office of Research and Development's 19 Centers of Innovation, aims to improve health outcomes among rural Veterans by examining the increasing role of technology on access.
VA Research’s Virtual Specialty Care Quality Research Initiative (QUERI) works with operational partners to determine how emerging technologies in areas such as telehealth can be best incorporated into clinical interventions to better serve rural Veterans.
If you are interested in learning about joining a VA-sponsored clinical trial, visit our research study information page.
Researchers from the White River Junction, Vermont, and Iowa City VA medical centers looked at how often Veterans enrolled with VA for care used VA and non-VA inpatient care, and whether this use varied substantially between rural and urban residents.
They found, in a paper published in 2017, that in states with higher proportions of urban residents, use of non-VA hospitals was lower for small or isolated rural town residents than urban residents; in more rural states it was greater. Rural enrollees also used VA hospitals more than urban enrollees did if they lived in the South. The team concluded that vouchers for non-VA inpatient care might have greater impact in rural states.
Cigarette smoking and rural Veterans—Previous studies have shown that, compared to the general U.S. population, military Veterans and those living in rural areas smoke cigarettes at higher rates, leading to increased health consequences. In a study published in 2019, researchers from the Durham VA Health Care System assessed more than 3,000 Iraq and Afghanistan era Veterans who had participated in a VA Mental Health study, and found that rural Veterans and Veterans with psychiatric issues were at increased risk of smoking and were also more severely dependent on nicotine than urban Veterans.
The team concluded that these findings underscored the need to reduce barriers for treatment for both smoking cessation and mental health care for Veterans who live in the nation’s most rural areas.
Reasons rural Veterans don't seek mental health care—In 2016, a team of researchers from the Central Arkansas Veterans Healthcare System in Little Rock and the VA Puget Sound Health Care System in Seattle interviewed 25 rural Veterans and 11 rural mental health care providers on the attitudes they thought most influenced rural Veterans' decisions to seek and continue to use mental health care. Both Veterans and providers agreed that the most important barrier was the importance rural Veterans place on independence and self-reliance. Stoicism, stigma associated with mental illness and health care, and a lack of trust in VA as a caring organization were also mentioned.
According to the survey participants, reluctance to seek care can be overcome by a perceived need for care and the support of other Veterans. Veterans are best encouraged to continue with care when they receive "warm handoffs" from medical to mental health care providers, when they perceive they are respected by providers and that the providers are perceived as caring about them, and when these providers are accessible to them and do not change over the course of treatment.
Use of psychotherapy among rural Veterans increasing—A 2015 study by researchers at three VA medical centers evaluated changes in rural and urban Veterans' use of psychotherapy between 2007 and 2010, a period in which VA was making significant efforts to engage rural Veterans in mental health care. They found that in those years the percentage of rural Veterans receiving psychotherapy increased from 17% to 22%, which the percentage of urban Veterans receiving such care increased from 24% to 28%.
The team concluded that gaps between rural and urban Veterans' use of psychotherapy were decreasing, and that efforts by VA to engage rural Veterans in care have been successful in reducing differences between the two groups.
Agricultural work has therapeutic value for rural Veterans—Growing Veterans is an organization that manages an organic farm in the Pacific Northwest staffed by Veterans and those who support them. The organization serves as a professional steppingstone, giving Veterans an opportunity to build their resumes and develop their individual skill sets. Members of local communities also volunteer to help out, creating lasting friendships and helping to bridge the gap between the Veteran and civilian populations.
A 2017 study led by researchers at the James A. Haley Veterans Hospital in Tampa, Florida, found that Veterans who participated in the program reported improvements in both their physical and mental health—factors that have an important impact on Veterans’ reintegration into society.
The Veterans harvested food that was sold at a farmer's market. They told researchers that their sleep, nutrition, and fitness levels improved and that they had a new sense of purpose and mission. The Veterans also reported declines in anxiety, pain, depression, the levels of medication they required, and substance abuse. Currently, there are more than 250 agricultural reintegration initiatives in the United States, according to the Farmer Veteran Coalition, an organization that helps Veterans advance their careers in agriculture by providing them with access to funding and other support services.
VA researchers have led the way in exploring the use of telehealth. Telehealth includes care provided through means such as the telephone, the Internet, videoconferencing, email, and text messaging.
These technologies are particularly important for Veterans living in rural areas, but also play a role in the delivery of care for other Veterans, such as those who are homebound because of illness or disability.
SCAN-ECHO program supports rural providers—VA's Specialty Care Access Network-Extension for Community Healthcare Outcomes (SCAN-ECHO) program uses video teleconferencing technology to link primary care providers, many of whom work in rural communities, to specialists at VA medical centers.
This exchange of information enables rural primary care clinicians to get access to the latest advances in health care research from VA experts throughout the nation. It also helps rural clinicians provide levels of care to Veterans that were not previously available in rural communities. This can benefit Veterans with chronic conditions who require complex care by eliminating the need to travel long distances for medical care.
Antimicrobial stewardship at rural hospitals—Misuse and overuse of antimicrobial medicines (medicines that kill microorganisms in the body or stop their growth) is a pressing public health program. Infectious organisms adapt to the antimicrobials designed to kill them, making the drugs ineffective. People affected with antimicrobial-resistant organisms are more likely to have longer, more expensive hospital stays, and may be more likely to die as the result of an infection. Antimicrobial stewardship is a coordinated program that promotes the appropriate use of the drugs, which includes antibiotics.
A pilot study conducted at two rural VA medical centers, published in 2018, found that telehealth can be a helpful tool for implementing antibiotic stewardship in hospitals, especially rural hospitals, that lack infectious disease specialists. In the study led by researchers at the VA Northeast Ohio Healthcare System, staff at the two hospitals formed teams that discussed infections and antimicrobial use among their patients during a weekly one-hour videoconference with an offsite infectious disease physician at another VA facility.
While the study did not assess whether the intervention reduced overall antibiotic use at either hospital, interviews with participants indicated that the sessions increased their awareness of antimicrobial stewardship principles and gave them greater confidence in their ability to make more targeted antibiotic choices and reduce the time Veterans are on antibiotics. The video component facilitated the process by allowing for face-to-face communication and helped build rapport with the off-site infectious disease physician.
Telehealth and HIV infection—VA's Center for Comprehensive Access and Delivery Research and Evaluation (CADRE), located in Iowa City, develops, implements, and tests innovative strategies that expand access to high-quality primary and specialty care, especially for rural Veterans, while ensuring that the care delivered is safe and free of preventable infections.
In 2013, CADRE researchers looked at the feasibility of telehealth collaborative care (TCC) for 24 Veterans with HIV infection in Iowa and Illinois. They found that, over the course of a year, the average travel time for health care over the course of a year for these patients decreased from 320 minutes to 170 minutes. VA's performance measures for HIV care were met for more than 90% of the patients in the study, and the team determined that this type of care is a feasible way to provide accessible and comprehensive care for rural Veterans with HIV.
In 2018, the CADRE team began a study to determine how effective TCC was compared with usual care for Veterans with HIV in rural areas. They are looking at whether TCC will provide the same levels of control of the virus, whether it will lead to improved retention in HIV care, and whether it can reduce mean blood pressure among Veterans with HIV and high blood pressure. Investigators will also attempt to determine whether the TCC program should be rolled out nationwide and hope to set the stage for future efforts to advance TCC implementation for HIV and potentially other chronic conditions. The study is expected to be completed in 2019.
Providing tablets leads to improved access and quality of care—In 2016, VA began distributing video-enabled computer tablets to Veterans with mental disorders and barriers to accessing care, including rural Veterans. A VA research team, led by investigators with the VA Palo Alto Health Care Center, looked at more than 700 tablet recipients and more than 1,000 Veterans in a control group to evaluate the implementation of this initiative.
The team found, in a study published in 2019, that Veterans who received the tablets had an increased number of psychotherapy visits and had their medications managed more intensively compared to the control group. Tablet recipients also were significantly more likely than control group participants to meet VA’s continuity of care measures for psychotherapy, and also had a lower rate of missed or canceled appointments. There were no significant differences between the two groups in the number of emergency department or urgent care visits.
Telemental health and women Veterans—Telemental health holds a great deal of promise for reducing barriers to mental health care. A team of researchers with the VHA HSR&D Center for the Study of Healthcare Innovation, Implementation and Policy located at the VA Greater Los Angeles Healthcare System conducted interviews with 40 VA leaders at facilities throughout the nation, as part of a study published in 2019.
The team found that VA leaders believe that telemental health increases access to mental health care, especially for rural women and those with other limiting circumstances. Women were particularly able to benefit from telemental health, because of responsibilities associated with child care, spousal care, and elder caregiving. The leaders were enthusiastic about telemental health’s potential and were eager to expand VA’s services in this area, including mental health groups for women only.
An ongoing study led by researchers with the VA Palo Alto Health Care System is looking at a skills-training treatment, called Skills Training in Affective and Interpersonal Regulation (STAIR), to be delivered by home-based video to help reduce posttraumatic stress disorder (PTSD) in women Veterans who have experienced military sexual trauma. The team hopes the use of this therapy will improve social functioning among these women and will provide a significant benefit to them, especially those women who reside in rural areas.
Telemental health shows improvements in PTSD symptoms—Community based outpatient clinics (CBOCs) provide primary care-based mental health services to rural Veterans who live long distances from VA hospitals. In a 2017 study, a team of researchers led by investigators from the Central Arkansas Veterans Healthcare System in Little Rock found that Veterans diagnosed with PTSD who receive their mental health treatment in large and medium-sized CBOCs were likely to have their levels of medication managed by CBOC providers, often by clinical video telehealth (CVT), a technology that enables patients and providers to use video conferencing software to hear and see each other. Very few of the Veterans studied, however, received evidence-based psychotherapy.
One researcher on the team, Dr. John Fortney, is now leading a study of a new program called Telemedicine Outreach for PTSD (TOP). The program is using telemedicine techniques to engage Veterans who receive care at 12 CBOCs throughout the nation in evidence-based, trauma-focused technology without their having to travel to a distant VA medical center. The study will be completed in 2020. It is hoped the results will lay the groundwork for national implementation of the TOP program.
Fortney and his team are guided by the Principles for Digital Development, a set of guidelines intended to help health care practitioners succeed in applying digital technologies to development programs. Using those principles as a guideline, the team designed, developed, and deployed a smartphone app to support collaborative care, in this case for Veterans with complex psychiatric conditions who receive care in rural health centers.
In a study published in 2018, the team found Veterans liked the system developed for them, and that it showed promise for sustained use. The team suggested future efforts to use health technologies to improve care for patients with psychiatric conditions should be designed for their public health impact, add value for all users, test the product and the process, acknowledge that there will be disruption, and anticipate variability.
HEROIC study—The Charleston VA Health Equity and Rural Outreach Innovation Center (HEROIC) is one of 18 nationally funded VA HSR&D Centers of Innovation (COINs) aimed at increasing the impact of health-services research on the health and health care of Veterans. HEROIC's mission is to improve access and equity in health care for all Veterans by eliminating geographic, racial, ethnic, and gender-based disparities.
In 2015, a study led by HEROIC researchers found that talk therapy delivered by two-way video calls is at least as effective as in-person treatment delivery for older Veterans with depression.
In the study, the research team recruited 241 Veterans aged 58 or older with major depression. The Veterans were randomly assigned to receive either telemedicine or same-room psychotherapy. Both groups received the same kind of treatment: behavioral activation, a talk therapy that emphasizes reinforcing positive behaviors.
The team found that telemedicine-delivered psychotherapy produced similar outcomes to in-person treatment. After a year of treatment, 39% of telemedicine patients and 46% of in-person therapy patients were no longer depressed, according to structured clinical interviews.
The team concluded that telemedicine is a good option for depressed older adults who live in geographically isolated areas, have barriers to mobility, or have some kind of stigma.
Use of interactive clinical video telemedicine—CVT enables patients and providers to use video conferencing software to hear and see each other. In certain situations, it can be used instead of a trip to the doctor’s office or to a clinic. A team of researchers led by investigators from the VA Puget Sound Health Care System and the University of Washington reviewed the use of CVT among 7.65 million Veterans using VA for care from 2009 to 2015.
The team found, in a study published in 2019, that there was a 300% growth in the use of CVT over that time period, and that the growth rate was faster among rural Veterans than urban Veterans. In fiscal year 2015, 3.2% of urban and 7.2% of rural Veterans used CVT for nearly 725,000 clinical encounters. These rates exceed published rates in the private health care market. The team concluded the availability of CVT has increased access to VA care for rural Veterans.
Regional and rural opioid prescribing—In a study published in 2019, researchers from the Iowa City VA Healthcare System and the University of Iowa looked to see whether rural Veterans received more prescriptions for opioids from VA clinicians compared to Veterans living in urban areas.
The team looked at the records of nearly 5 million VA patients and found that rural Veterans received 30% more opioids than their urban counterparts. They concluded that further research is needed to identify and address the causes of these differences, which could include the fact that it is more difficult for rural Veterans to access treatments for chronic pain that do not require medication, the researchers hypothesized.
Increasing mental health care access, continuity, and efficiency for Veterans through telehealth with video tablets. Jacobs JC, Blonigen DM, Kimerling R, Slightam C, Gregory AJ, Gurmessa T, Zulman DM. Distributing video-enabled tablets to Veterans with mental health conditions appeared to improve access to and continuity for mental health services while improving clinical efficiency by decreasing missed opportunities for care. Psychiatr Serv. 2019 Aug 5:applps201900104. (Epub ahead of print)
Utilization of interactive clinical video telemedicine by rural and urban Veterans in the Veterans Health Administration Health Care System. Adams SV, Mader MJ, Bollenjer MJ, Wong ES, Hudson TJ, Littman AJ. CVT utilization in VHA has increased quickly and exceeds published rates in the private health care market. J Rural Health, 2019 Jun;35(3):308-318.
Differences in receipt of alcohol-related care across rurality among VA patients living with HIV with unhealthy alcohol use. Among people living with HIV with unhealthy alcohol use, those in rural areas may be vulnerable to under-receipt of specialty addictions treatment. J Rural Health. 2019 Jun;35(3):341-353.
Regional and rural-urban variation in opioid prescribing in the Veterans Health Administration. Lund BC, Ohl ME, Hadlandsmyth K, Mosher HJ. Rural Veterans receive over 30% more opioids than their urban counterparts in VHA. Mil Med. 2019 May 21 (Epub ahead of print)
Rural and urban differences in the adoption of new health information and medical technologies. Haggstrom DA, Lee JL, Dickinson SL, Skanersi S, Roberts JL, Teal E, Baker LB, Rawl SM. Differences in health information technology use between rural and urban populations may be modified by social determinants. J Rural Health. 2019 Mar;35(2):144-154.
Cigarette smoking rates among Veterans: association with rurality and psychic disorders. Coughlin LN, Wilson SM, Erwin MC, Beckham JC; VA Mid-Atlantic MIRECC Workgroup, Calhoun PS. Rural Veterans and Veterans with psychiatric comorbidities are at increased risk of smoking and are more severely dependent on nicotine than urban Veterans. Addict Behav. 2019 Mar;90:119-123.
Outcomes comparison in patients admitted to low complexity rural and urban intensive care units in the Veterans Health Administration. O’Shea AMJ, Fortis S, Vaughan Sarrazin M, Moeckli J, Yarbrough WC, Schacht Reisinger H. Low complexity ICUs in rural facilities fare similarly to urban counterparts in mortality, length of stay, and interhospital transfer measures. J Crit Care. 2019 Feb;49:64-69.
Facilitators and barriers to seeking mental health care among primary care Veterans with posttraumatic stress disorder. Possemato K, Wray LO, Johnson E, Webster B, Beehler GP. Strategies to help Veterans overcome barriers to care may benefit from a focus on negative treatment-seeking beliefs and tailoring based on a Veteran’s rural or urban status. J Trauma Stress. 2018 Oct;31(5):742-752.
A pilot study using telehealth to implement antimicrobial stewardship at two rural Veterans Affairs medical centers. Stevenson LD, Banks RE, Stryczek KC, Crnich CJ, Ide EM, Wilson MB, Viau RA, Ball SL, Jump RLP. A pilot study successfully demonstrates the feasibility of using telehealth to support antimicrobial stewardship at rural VAMCs with limited access to local infectious disease expertise. Infect Control Hosp Epidemiol. 2018 Oct;39(10):1163-1169.
The impact of a change in the price of VA health care on utilization of VA and Medicare services. Nelson RE, Hicken B, Vanneman M, Liu CF, Rupper R. VA outpatient care may be a substitute for Medicare outpatient care for Medicare-enrolled Veterans living in rural areas. Med Care. 2018 Jul;56(7):569-576.
Applying the Principles for Digital Development: case study of a smartphone app to support collaborative care for rural patients with posttraumatic stress disorder or bipolar disorder. Bauer AM, Hodsdon S, Bechtel JM, Fortney JC. Adhering to the Principles for Digital Development, the team successfully created and deployed a mobile health system to support collaborative care for patients with complex psychiatric conditions in rural health centers. J Med Internet Res. 2018 Jun 6;20(6):e10048.
Availability of healthcare providers for rural veterans eligible for purchased care under the Veterans Choice Act. Ohl ME, Carrell M, Thurman A, Web MV, Pharm TH, Mengeling M, Vaughn-Sarrazin M. Initiatives to purchase care for Veterans living more than 40 miles from VHA facilities may not significantly improve their access to care, as these areas are underserved by non-VHA providers. BMC Health Serv Res. 2018 May 29;18(1):315.
The use of telemental health to meet the mental health needs of women using Department of Veterans Affairs services. Moreau JL, Cordasco KM, Young AS, Oiehl SM, Rose DE, Canelo I, Yano EM, Haskell SG, Hamilton AB. Telemental health is a good fit for helping address the perceived needs of women Veterans, especially in addressing the geographical barriers experienced by rural women and those with a limited ability to travel. Womens Health Issues. 2018 Mar-Apr;28(2):181-187.
Rooted in the community: assessing the reintegration effects of agriculture on rural Veterans. Besterman-Dahan K, Chavez M, Njoh E. Veterans who participated in a community agriculture initiative reported general improvements in physical and mental health, including improvements in sleep, nutrition, and exercise, and decreases in anxiety, pain, depression, and medication and substance use, all known factors that affect Veteran reintegration. Arch Phys Med Rehabil. 2018 Feb;99(2S):S72-S78.
Justice involvement and treatment use among rural Veterans. Finlay AK, Harris AHS, Rosenthal J, Blue-Howells J, Clark S, Flatley B, Timko C. Telehealth, outreach services, and integrated treatment may help address challenges to treatment entry experienced by rural Veterans and justice-involved Veterans. Rural Ment Health. 2018 Jan;42(1):46-59.
Barriers and facilitators to implementation of VA home-based primary care on American Indian reservations: a qualitative multi-case study. Kramer BJ, Cole SD, Lee DI, Creekmur B, Saliba D. Opportunities for shared learning would benefit federal health care organizations to expand other medical services to additional American Indian communities and other rural and underserved communities, as well as to coordinate with other health care organizations. Implement Sci. 2017 Sep 3;12(1):109.
Usual care for rural Veterans with posttraumatic stress disorder. Grubbs KM, Fortney JC, Kimbrell T, Pyne JM, Hudson T, Robinson D, Moore WM, Custer P, Schneider R, Schnurr PP. Veterans diagnosed with PTSD who receive their mental health treatment in large and medium CBOCs are likely to receive medication management, and very few Veterans received evidence-based psychotherapy. J Rural Health. 2017 Jun:33(3):290-296.
Overcoming barriers to sustained engagement in mental health care: Perspectives of rural veterans and providers. Fischer EP, McSweeney JC, Wright P, Cheney A, Curran GM, Henderson K, Fortney JC. System support for peer and provider behaviors that generate trust and demonstrate caring may help overcome attitudinal barriers to treatment-seeking and sustained engagement in mental health care among rural veterans. J Rural Health. 2016 Sep;32(4):429-38.
Health and health care access of rural women veterans: Findings from the National Survey of Women Veterans. Cordasco KM, Mengeling MA, Yano EM, Washington DL. Rural women Veterans have significantly worse physical health function and were more likely to exclusively use VA care compared with urban women Veterans. Affordability and transportation are major barriers to care for rural women veterans. J Rural Health. 2016 Sep;32(4):397-406.

Download PDF
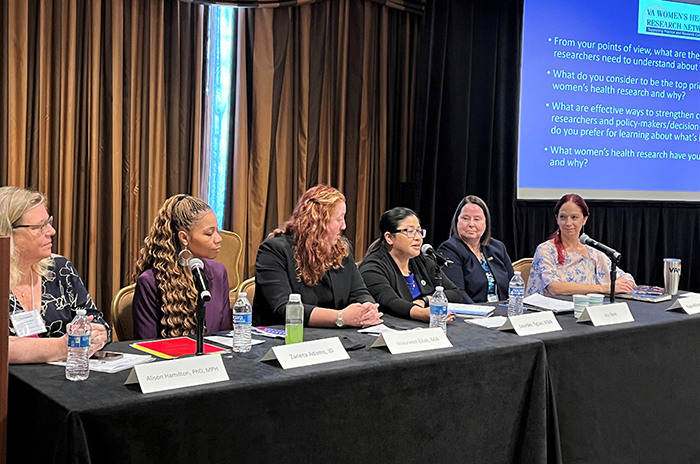 2023 VA Women's Health Research Conference
2023 VA Women's Health Research Conference
 Photos shed light on food insecurity in post 9/11 Veterans
Photos shed light on food insecurity in post 9/11 Veterans
 VA clinical trial examines optimal treatment for Veterans with early stage lung cancer
VA clinical trial examines optimal treatment for Veterans with early stage lung cancer