Vaccines lower long COVID risk
 Photo: ©iStock/Kuzmik_A (07/25/2024)
VA St. Louis researchers demonstrated vaccination substantially lowered the risk of long COVID. The study included VA medical records of nearly 450,000 Veterans who had COVID-19 between 2020 and 2022, along with 4.7 million Veterans who were not infected during that time. In the COVID group, 3.5% of those who were vaccinated developed long COVID symptoms one year after infection, compared to 7.8% of unvaccinated Veterans. The study also showed the risk of long COVID has declined since the beginning of the pandemic, with the researchers attributing three-quarters of the decline to the availability of vaccines and the remaining quarter to changes in virus strains. (New England Journal of Medicine, Jul. 17, 2024)
|
Residential treatment better manages alcohol use disorder
 Photo: ©iStock/donfiore (07/25/2024)
A study of 19 VA medical centers showed residential treatment programs helped Veterans hospitalized for alcohol withdrawal stay out of the hospital and avoid relapsing. Veterans discharged to a live-in program had 61% reduced odds of being readmitted to the hospital within 30 days and were 2.5 times more likely to remain abstinent from alcohol, whereas being prescribing alcohol use disorder medications did not improve odds of readmission or abstinence. The findings suggest health care systems should invest in residential treatment programs and encourage patients to be discharged to them to help manage withdrawal and avoid a return to heavy alcohol use. (Journal of Hospital Medicine, Jul. 19, 2024)
|
Online training program improves PTSD, depression symptoms
 Photo: ©iStock/Moyo Studio (07/25/2024)
A VA Palo Alto study showed a peer-supported online program can improve PTSD and depression symptoms. A group of 128 Veterans were assigned to either webSTAIR, a six-module online program designed to improve mood and interpersonal regulation, or a waitlist control group. The webSTAIR group had greater improvements in PTSD, depression, emotion regulation, and functional impairment, which they maintained eight weeks after completing the program. Furthermore, Veterans who completed more modules had greater improvements on all outcomes. The results suggest online, peer-supported technology programs can be a low-burden and effective way to help Veterans improve their mental health. (Journal of Medical Internet Research, Jul. 9, 2024)
|
Dual-artery bypass surgery superior to singly-artery surgery
 Photo: ©iStock/Panuwat Dangsungnoen (07/17/2024)
VA researchers in Boston and Maryland showed dual-artery bypass grafting is superior to single-artery grafting for Veterans undergoing bypass surgery. Among nearly 26,000 Veterans who had bypass surgery during a 10-year period, only 5% received dual arterial grafts, in which multiple vessels are used to allow blood to flow past a blocked artery. Compared to those receiving single-artery grafts, those receiving dual-artery grafts were 30% less likely to die during the five-year follow-up period and 20% less likely to have a major cardiac or cerebrovascular event such as heart attack or stroke. The results suggest this method of bypass surgery should be promoted in VA to improve patient outcomes. (Journal of Surgical Research, Jul. 5, 2024)
|
Depression may increase odds of cognitive impairment in Women Veterans
 Photo: ©iStock/Giselleflissak (07/17/2024)
A study by VA researchers and colleagues in Washington, DC, found Vietnam-era Women Veterans with a probable diagnosis of depression had 61% greater odds of cognitive impairment. The researchers surveyed 4,000 Women Veterans 60 or older and found higher symptom severity from PTSD and depression increased the odds of cognitive impairment, but a PTSD diagnosis without depression did not. The results suggest Vietnam-era Women Veterans with depression would benefit from cognitive function screening. (Journal of Women’s Health, Jun. 24, 2024)
|
Camp Lejeune toxic exposure linked to faster Parkinson’s disease progression
 Photo courtesy of DVIDS. (07/17/2024)
VA researchers from San Francisco; Hines, Illinois; and Canandaigua, New York, learned Veterans exposed to contaminated water at Camp Lejeune may have an accelerated progression of Parkinson’s disease. The study included 270 Marines with Parkinson’s disease who lived at Camp Lejeune between 1975 and 1985. The hazards of psychosis, falls, and fractures were twice as high in those exposed to trichloroethylene and other volatile organic compounds in the residential water. Toxic exposure was also linked to earlier presentation of these symptoms. The findings suggest exposure to these toxins may increase Parkinson’s disease risk and speed the disease’s advancement. (Movement Disorders, Jul. 11, 2024)
|
Researchers identify new thyroid cancer biomarker
 Photo: ©iStock/FatCamera (07/10/2024)
VA Nebraska-Western Iowa researchers identified a new biomarker for thyroid cancer. They found high levels of the hormone relaxin-2 in thyroid cancer tumors that were not present in tumor-adjacent tissue or thyroid tissue in people without cancer. Corresponding changes in immune cell expression suggest relaxin-2 may play a role in suppressing the immune system and allowing tumors to grow. This hormone may be a target for developing new thyroid cancer treatments. (Biochemical Pharmacology, July 1, 2024)
|
Some social risks common among Veterans needing hospital readmission
 Photo: ©iStock/peterspiro (07/10/2024)
VA researchers used a social risk assessment tool to analyze more than 150,000 Veterans admitted to a VA hospital between 2016 and 2022. Food insecurity, legal needs, and neighborhood deprivation were the social risk factors most associated with rehospitalization within 30 days of the first hospitalization. Food insecurity, legal problems, and violence were linked to emergency department use. The results suggest a tool to rate social risk could be used to direct specialized interventions and resources to help Veterans after hospital stays. (Health Services Research, Jul. 7, 2024)
|
Veterans less likely to receive treatment for stimulant use than opioid use
 Photo: ©iStock/Emilia Kohn (07/10/2024)
VA Puget Sound and Ann Arbor researchers learned Veterans with stimulant use disorder are less likely than Veterans with opioid use disorder to receive treatment. In a group of more than 130,000 Veterans with at least one health care visit for substance use disorder, those with stimulant use disorder had 44% lower odds of receiving any treatment, and 49% lower odds of receiving outpatient treatment, but were more likely to need residential treatment or be hospitalized. Veterans with both opioid use and stimulant use disorders were more likely to receive treatment than those with stimulant use disorder only. The results highlight a need for stimulant use disorder-specific care and efforts to reduce hospitalizations for these Veterans. (Journal of Addiction Medicine, Jun. 4, 2024)
|
Opt-out treatment approach more likely to help Veterans quit smoking
 Photo: ©iStock/Zhang Rong (07/03/2024)
Minneapolis VA researchers demonstrated an opt-out tobacco treatment program can help Veterans undergoing substance use treatment quit smoking. Veterans in an intensive outpatient program for substance use disorders were either automatically enrolled in an embedded group tobacco cessation program that they could then opt out of, or offered opt-in tobacco treatment they needed to choose to join. Nearly 25% of those in the opt-out group successfully quit smoking, compared with about 3% of the opt-in group. Those in the opt-out group were also more likely to receive tobacco cessation medications. The results show an opt-out approach embedded in treatment is more likely to help Veterans quit smoking than opt-in programs. (Nicotine & Tobacco Research, May 31, 2024)
|
Study finds racial disparity in anticoagulant prescriptions
 Photo: ©iStock/Hailshadow (07/03/2024)
A study by VA Pittsburgh researchers showed Veterans receiving care at VA facilities that serve more minority patients were less likely to receive the recommended anticoagulants, such as warfarin, for atrial fibrillation. The study included data on nearly 90,000 Veterans at 140 VA medical centers across the country. Patients at VA medical centers serving the highest percentage of minority patients had 22% lower odds of beginning recommended anticoagulant therapy. The findings suggest a need to address racial disparities in anticoagulant prescribing and to encourage guideline-recommended treatments for atrial fibrillation. (JAMA Network Open, Jun. 3, 2024)
|
Sleep apnea increases risk of death in younger, but not older people
 Photo: ©iStock/rdegrie (07/03/2024)
Researchers with the Michael E. DeBakey VA Medical Center in Houston learned sleep apnea may be associated with an increased risk of death in younger people, while the opposite seemed true in older people. In a study of more than 146,000 people, 1.9% of those 40 or younger who suffered from severe sleep apnea died during the study period, compared to 1.5% of those without sleep apnea. However, in people 65 or older, 26.4% of those with severe sleep apnea died during the study period, compared to 40.2% of those without sleep apnea. Further study is needed to determine if the harmful effects of sleep apnea actually diminish with age. (Sleep Medicine, Jun. 13, 2024)
|
Nirmatrelvir-ritonavir protects at-risk Veterans from COVID-19 hospitalization, death
 Photo: ©iStock/yacobchuk (06/26/2024)
VA researchers showed nirmatrelvir-ritonavir effectively reduced hospitalization and death in people at risk for severe COVID-19. The study compared more than 24,000 Veterans treated for COVID-19 with nirmatrelvir-ritonavir to an equal number who had COVID-19 but did not receive the medications. Nirmatrelvir-ritonavir reduced the absolute risk of hospitalization or death in the first 30 days by nearly 3% in Veterans at the highest risk for severe COVID, nearly 2% in immunocompromised Veterans, and 1% in Veterans 75 or older. Nirmatrelvir-ritonavir did not change the risk of hospitalization or death for Veterans at the lowest risk or those younger than 65. The results suggest the drugs could be an effective way to protect those most at risk from COVID-19. (Clinical Infectious Diseases, Jun. 12, 2024)
|
VA wait times shorter than in community care for many Veterans
 Photo: ©iStock/Fly View Productions (06/26/2024)
VA Boston researchers learned of racial disparities in community health care wait times for Veterans. In an analysis of more than five million Veterans, overall wait times were 35 days or longer in community care, and less than 35 days at VA facilities. Furthermore, Black Veterans had to wait about 10% longer than White Veterans for community care, but had 5% shorter wait times than White Veterans for VA care. For Hispanic Veterans, community care wait times were only longer than White Veterans’ in rural areas, while VA care wait times were longer in both rural and urban areas. The results highlight a continuing need to promote equitable care access for Veterans regardless of race or location. (JAMA Health Forum, Jun. 7, 2024)
|
Inflammatory bowel disease linked to increased risk of kidney injury
 Photo: ©iStock/mediamasmedia (06/26/2024)
A study by a VA Pittsburgh researcher and colleagues showed patients with inflammatory bowel disease (IBD) were 27% more likely that those without the disease to have an acute kidney injury. Patients hospitalized with IBD were also 32% more likely to have an acute kidney injury than patients hospitalized with collagen vascular diseases, a different class of autoimmune disease. The study included 5.7 million people, 57,000 of whom had IBD. The results suggest coexisting kidney disease should be considered among IBD patients, but more research is needed on possible shared causes of the two conditions. (Kidney Medicine, Jun. 7, 2024)
|
Veterans in highly deprived areas have higher odds of death post-surgery
 Photo: ©iStock/FG Trade (06/20/2024)
VA Pittsburgh and Iowa City researchers learned older Veterans living in disadvantaged neighborhoods had a higher chance of death after surgery. The study included more than 93,000 Veterans at least 65 years old who recently had surgery. Those who lived in areas with fewer education, employment, and quality housing options had 15% higher odds of dying within 30 days of an in-patient hospital stay. Veterans who received care outside VA had slightly higher odds of death compared to Veterans receiving VA care, while Black Veterans and those who lived in rural areas had lower odds of death after surgery. The results show a need for better care outreach for Veterans living in high poverty areas. (Journal of Surgical Research, Jun. 3, 2024)
|
Female Veterans retain higher levels of psychological distress after a suicide attempt
 Photo for illustrative purposes only. ©iStock/ArtistGNDphotography (06/20/2024)
A study by VA Portland researchers and colleagues found female Veterans retain higher feelings of social rejection and institutional betrayal and lower self-compassion and autonomy than male Veterans after a nonfatal suicide attempt. The survey of 968 Veterans included an equal number of men and women. Higher self-compassion was associated with lower suicidal ideation in both men and women, but this connection was stronger in women. Social rejection was the strongest factor in worsening psychological distress in the study group. Unsurprisingly, Veterans with higher overall psychological distress had the greatest odds of further suicide attempts. The results highlight the need for suicide prevention efforts tailored to the needs of female Veterans. (Journal of Affective Disorders, May 28, 2024)
|
Flu increases risk of heart attack, stroke
 Photo: ©iStock/LittleCityLifestylePhotography (06/20/2024)
White River Junction VA researchers and colleagues showed the flu can significantly increase the risk of heart and vascular problems. Researchers analyzed more than 3,400 cases of Veterans hospitalized for coronary or cerebrovascular events between 2010 and 2018. After a lab-confirmed case of the flu, the risk of non-ST-segment elevation myocardial infarction, a type of heart attack, was seven times greater at one week than it was a year before or after. The risk of hemorrhagic stroke was six times greater, and risk of ischemic stroke was four times greater. The flu was also associated with exacerbation of pre-existing asthma, chronic obstructive pulmonary disease, and congestive heart failure. The results emphasize the need for flu prevention measures to guard against serious complications. (Influenza and Other Respiratory Viruses, Jun. 6, 2024)
|
Clinicians agree on outreach for tobacco treatment, disagree on priorities, methods
 Photo: ©iStock/dem10 (06/12/2024)
A VA Minneapolis study interviewed 21 clinicians, including pharmacists, nurses, pulmonologists, and physicians, about a proactive outreach program to inform patients with chronic obstructive pulmonary disease (COPD) who smoke about various options for Tobacco Dependence Treatment (TDT). These included both local options like cessation clinics, individual counseling, and group classes, and nationwide options such as the Quitline (1-855-QUIT-VET), the VA-sponsored cessation app, or the Smokefree text messaging program. While most clinicians agreed that proactive outreach for TDT was needed, many expressed doubt that automated or technology-based methods could be effective, especially in people over 50. Most clinicians preferred a combination of pharmaceutical and therapeutic treatments for COPD, but disagreed on which populations should be prioritized, such as younger vs. older or those most ill vs. groups with the most risk. The study also found many clinicians did not know about all the TDT programs available for Veterans. The researchers encouraged health systems to leverage implementation strategies in order to increase enrollment in tobacco cessation programs. (Journal of General Internal Medicine, June 3, 2024)
|
Women more likely to receive harmful PTSD medication
 Photo: Photo: ©iStock/Domepitipat (06/12/2024)
Researchers with the VA Center for Access and Delivery Research and Evaluation in Iowa found Women Veterans with PTSD were 67% more likely than men to receive medication that VA clinical practice guidelines recommend against, also known as guideline discordant medications (GDM). After adjusting for bipolar disorder, age, or prior psychiatric medication, Women Veterans had a 22% greater risk of receiving a GDM. Of more than 700,000 Veterans with PTSD, 16.9% of women and 10.1% of men received a GDM. These GDMs include benzodiazepines, antipsychotics, select anticonvulsants, and select antidepressants. The study was not able to determine why so many Women Veterans had prescriptions outside of VA guidelines, or how many may have GDM exposure from non-VA sources. The researchers concluded further study is needed to inform clinical practice about the distinct needs of Women Veterans going through PTSD treatment. (The Journal of Clinical Psychiatry, June 5, 2024)
|
Health record tools can reduce clinician burnout
 Photo: ©iStock/metamorworks (06/12/2024)
VA Los Angeles researchers performed several cross-sectional analyses of a VA primary care personnel survey to find nine tools associated with lower odds of burnout. While technological burden is frequently cited as a cause of burnout, this study found those clinicians who used tools that help manage Electronic Health Records (EHR) had lower levels and less frequent symptoms of burnout. VA primary care teams have access to several internally developed tools, including a risk prediction algorithm, quality dashboards and registries, case management software, a housing instability indicator, and many more. The researchers recommended healthcare administrators carefully consider the potential workplace effects of introducing population health management tools for healthcare clinicians and trainees, but also warn of the potential for unintended increased workload related to these tools. (BMC Primary Care, May 15, 2024)
|
Active lifestyle may put older adults at greater risk for traumatic brain injury
 Photo: ©iStock/Zinkevych (06/05/2024)
A VA San Francisco study showed older adults who were healthier and wealthier were more likely to sustain traumatic brain injuries (TBIs). Previous studies suggested people of lower socioeconomic status and poorer health were at greater risk for TBIs, but most of those studies used a younger population. In a group of more than 9,200 adults, with an average age of 75, 13% experienced TBI, mostly from falls. Participants with no cognitive dysfunction, no functional impairment, and no baseline lung disease had the highest risk of TBI. About 31% of participants with TBI were in the highest wealth group, while 22% were in the lowest wealth group. White and female study participants also had elevated rates of TBI, with women representing 58% of the study group but 64% of the TBIs. White participants represented 84% of the study group but 89% of the TBIs. The researchers hypothesized healthier adults who lead a more active lifestyle may engage in activities that put them at greater risk of falls. (JAMA Network Open, May 31, 2024)
|
Increased mental health staffing decreases Veterans’ time to initiating care
 Photo: ©iStock/EmirMemedovski (06/05/2024)
VA Boston researchers learned mental health staffing levels were the most important factor in Veterans beginning VA mental health care soon after leaving active-duty service. The study, which followed more than 54,000 Veterans recently separated from the military who had PTSD, depression, or substance use disorder, showed an increase in mental health staffing led to significantly faster initiation of mental health care. The effect of increased staffing was especially meaningful at smaller VA facilities with fewer mental health staff. Staffing had a greater effect on time to mental health care engagement than all other variables examined, including age, gender, race, driving distance, and income. The findings highlight the importance of mental health professionals’ availability on Veterans’ access to care. (Health Services Research, June 2, 2024)
|
Long COVID risk decreases significantly after three years
 Image: ©iStock/mustafahacalaki (06/05/2024)
A VA St. Louis study showed the risk of death from long COVID decreases significantly after three years. The study of more than 5 million Veterans found people who had been hospitalized with COVID-19 had a risk of death three years after infection that was 29% higher than those who did not contract COVID-19, which was significantly lower than the first year post-infection, which was 217% higher. Likewise, the risk of long COVID symptoms declined three years after infection for all COVID-19 patients, with hospitalized patients having a 34% higher risk, down from a 182% higher risk in the first year. Non-hospitalized patients only had a nominally higher risk in the third year, down from a 23% higher risk in the first year. While the findings show long COVID risks wane over time, the researchers cautioned there is still a substantial health burden for people who contract severe COVID-19. (Nature Medicine, May 30, 2024)
|
Schizophrenia drug may increase blood cancer risk
 Photo: ©iStock/Ole Schwander (05/30/2024)
Iowa City VA researchers learned the schizophrenia medication clozapine may increase the risk of blood cancers. The study included more than 25,000 Veterans with schizophrenia, 2,300 of whom were diagnosed with leukemia, lymphoma, or myeloma. The odds of blood cancer increased by 31% after any clozapine use. Veterans who had been taking clozapine for five or more years had an 88% increase in cancer odds, suggesting longer exposure increases the risk. The findings suggest patients taking clozapine for schizophrenia should be closely monitored for blood cancers. (Journal of Clinical Psychiatry, May 15, 2024)
|
Arthritis drug decreases delirium, coma in critically ill COVID-19 patients
 Photo: ©iStock/Wavebreakmedia (05/30/2024)
A study including a VA Tennessee Valley researcher found the arthritis drug tocilizumab can decrease delirium and coma in critically ill patients with COVID-19. The study included 253 patients with COVID-19 being treated in the ICU, 69 of whom received tocilizumab. The tocilizumab group had a greater number of days without delirium or coma. The drug did not affect mortality, ventilator use, or hospital length of stay. The results indicate tocilizumab could be an effective way to address delirium and comas in severely ill COVID-19 patients. (Scientific Reports, May 23, 2024)
|
Gulf War illness and irritable bowel syndrome often occur together
 Photo: ©iStock/Chaichan Pramjit (05/30/2024)
A study by Houston and Durham VA researchers found nearly half of Gulf War-era Veterans with Gulf War illness (GWI) also had irritable bowel syndrome (IBS). In a group of 578 Gulf War Veterans, 72% were diagnosed with severe Gulf War illness and 50% had been diagnosed with IBS at some point. Those with severe GWI were more likely to have both current and previous IBS diagnoses. The researchers recommend both that Veterans with GWI be screened for IBS and that Veterans with IBS who served during the Gulf War be screened for GWI. (Military Medicine, May 21, 2024)
|
MVP using genetic data to improve Veteran care
 Photo: ©iStock/FatCamera (05/22/2024)
VA researchers in Boston created a pilot program using Million Veterans Program data to directly improve the health care of individual Veteran participants. In the MVP-Return of Actionable Genetic Results (MVP-ROAR) study, researchers recontacted MVP participants and invited them to receive genetic counseling based on their genetic risk for diseases. The pilot study focused on Veterans genetically predisposed to high cholesterol, with participants who received counseling significantly lowering their cholesterol six months after the intervention. The MVP-ROAR study marks a turning point in MVP and demonstrates the feasibility of returning genetic results to individual participants and providers. (American Heart Journal, May 16, 2024)
|
Weight training, bicycling protect against knee pain
 Photo: ©iStock/mikkelwilliam (05/22/2024)
Two studies led by a Houston VA researcher showed different forms of exercise earlier in life can lower the risk of knee pain and arthritis. The first study found people with a history of strength training were 23% less likely to have symptomatic knee arthritis. The second study found people who biked regularly at any point in their lives were 17% less likely to develop knee pain and 21% less likely to develop osteoarthritis. The more frequent the exercise, the less likely a person was to develop knee pain. The results show that exercise that builds muscle around the knee and promotes mobility and weight maintenance are important for knee health later in life. (Arthritis & Rheumatology, March 2024; Medicine and Science in Sports Exercise, Apr. 11, 2024)
|
Adaptive video games improve disabled Veterans’ employment rates
 Photo: ©iStock/Dragos Condrea (05/22/2024)
A VA Pittsburgh study found Veterans with physical disabilities who participated in adaptive gaming in their free time were more likely to be employed. Out of more than 600 participants, 58% were employed either full- or part-time, more than double the national average for people with disabilities. About 75% of employed Veterans reported subjective benefits of playing video games, such as improved mental health, physical function, and cognition. Nearly half of Veterans who were employed used their adaptive video game equipment – such as modified computer mice, keyboards, and joysticks – most or all the time while completing work tasks, and those who used their gaming equipment for work were more likely to be employed full-time. The findings show adaptive gaming offers Veterans employment benefits both from accessible equipment and from mental and physical engagement. (Disability and Rehabilitation, Apr. 9, 2024)
|
New chemotherapy method could improve pancreatic cancer treatment
 Photo: ©iStock/Zinkevych (05/08/2024)
Kansas City VA researchers and colleagues developed a molecular method to deliver pancreatic cancer chemotherapy more effectively to tumors. They created nanoparticles that encapsulate the chemotherapy drug gemcitabine; these nanoparticles respond to the pH and microenvironment inside pancreatic tumors, helping to release the drug in the correct location. The nanoparticles also inhibit the production of cellular chemicals that make the drug less effective. In mouse models of pancreatic cancer, the drug delivery method significantly slowed tumor growth and prolonged survival. The results show nanoparticle encapsulation is a promising approach to enhance pancreatic cancer treatment. (PLoS One, Apr. 30, 2024)
|
Rising blood pressure linked to distress in Veterans with dementia
 Photo: ©iStock/SDI Productions (05/08/2024)
A study of more than 7,000 VA nursing home residents showed increases in blood pressure often preceded episodes of distress in Veterans with dementia. According to Veterans’ health records data, systolic blood pressure began to rise seven days before a distress incident, and the elevated blood pressure persisted one week after. The researchers did not find any significant changes in blood pressure medications during the same time period that could affect the possible co-relation. The results suggest monitoring blood pressure could help predict and help prevent distress in people with dementia. (PLoS One, Apr. 30, 2024)
|
National VA Research Week begins Monday
(05/08/2024)
May 13–17 is National VA Research Week, scheduled to begin with a kick-off event and awards ceremony Monday at the VA Central Office in Washington, DC. Local VA medical centers across the country will hold their own events throughout the week to highlight how VA’s innovative national research enterprise can improve health care for Veterans and people around the world. This year’s theme is “Building Community Through Research,” as VA celebrates researchers’ contributions to both the Veteran community and the health science community as a whole. You can find out more information here.
|
$6 million approved for intimate partner violence intervention study
 Photo: ©iStock/SDI Productions (05/01/2024)
The Patient-Centered Outcomes Research Institute has awarded VA researchers in Boston and Philadelphia $6 million in funding to study a personalized intervention for Veterans who have experienced intimate partner violence (IPV). The five-year study will compare standard IPV counseling with a program called Recovering from IPV through Strengths and Empowerment (RISE). RISE is a flexible intervention that addresses safety planning, IPV health effects and warning signs, coping and self-care, social support, sexual violence over the lifespan, connecting with resources, and how to move forward. The study will assess self-efficacy and depression symptoms for a year after the RISE intervention. (VA Boston Health Care, April 29, 2024)
|
Long COVID more likely in Veterans with psychiatric disorders
 Photo: ©iStock/Wavebreakmedia (05/01/2024)
VA San Francisco researchers learned Veterans with at least one psychiatric disorder were 28% more likely to be diagnosed with long COVID after a COVID-19 infection. Out of more than 660,000 Veterans who tested positive for COVID-19, those with depression, anxiety, and stress-related disorders had the highest risk of long COVID. The connection between psychiatric disorders and long COVID was most prominent in younger Veterans. The findings highlight a need to improved monitoring for long COVID symptoms in Veterans with psychiatric disorders. (Psychological Medicine, Feb. 5, 2024)
|
Written exposure therapy improves PTSD symptoms
 Photo: ©iStock/Liudmila Chernetska (05/01/2024)
A Southeast Louisiana VA pilot study showed a condensed written exposure therapy program has potential as a treatment for PTSD. Veterans engaged in writing sessions focused on identifying and processing traumatic events once a day for at least five consecutive days. Most participants found the sessions to be useful and acceptable. Assessment revealed significant reductions in PTSD, depression, and functional impairment symptoms after the treatment. The study is the first to show written exposure therapy delivered over consecutive days can improve PTSD, suggesting its usefulness in acute inpatient mental health settings. (Journal of Traumatic Stress, Apr. 7, 2024)
|
Medication to help bowels could harm kidneys
 Photo: ©iStock/Doucefleur (04/25/2024)
VA researchers from Memphis, Tennessee, and Long Beach, California, learned inflammatory bowel disease (IBD) medication may increase the risk of kidney disease. In a study of more than 10,000 Veterans with IBD, those taking anti-tumor necrosis factor inhibitors had a 34% higher risk of progressive decline in kidney function. However, the medications were not associated with any change in risk of death. The findings highlight a need for careful monitoring of kidney function in people being treated for IBD. (JAMA Network Open, Apr. 1, 2024)
|
Virtual program can effectively treat PTSD
 Photo: ©iStock/Renata Angerami (04/25/2024)
A Salisbury, North Carolina, VA study found intensive virtual treatment for PTSD can be just as effective as in-person residential treatment. During the COVID-19 pandemic, VA researchers at the W. G. (Bill) Hefner VA Medical Center developed a Virtual Intensive Outpatient Program for PTSD. In a study of 370 Veterans, those receiving the virtual program had similar PTSD symptom reductions as Veterans receiving residential care. The results show virtual treatment can be a viable PTSD treatment alternative for Veterans who cannot attend residential care. (Psychological Trauma, Apr. 4, 2024)
|
Caring Contacts shows uplifting texts can help prevent suicide
 Photo: ©iStock/Delmaine Donson (04/25/2024)
Southeast Louisiana VA researchers showed the text-based Caring Contacts program holds promise as a means of suicide prevention for Veterans transitioning from military service to civilian life. In this pilot program, the study team sent approximately five text messages over three months expressing care and concern to Veterans recently separated from the military. Participants said they found the messages comfortable and convenient, and that the messages had a positive impact on their mood. This pilot study suggests the Caring Contacts texts could be a simple and effective way to improve Veterans’ health care engagement and ease their post-military transition. (Psychological Services, Apr. 18, 2024)
|
Two antidepressants may protect against chemotherapy-related hearing loss
 Photo: ©iStock/FatCamera (04/18/2024)
VA researchers in Columbia, S.C., found two antidepressant medications that may also protect against hearing problems caused by the chemotherapy drug cisplatin. In a group of more than 20,000 Veterans receiving cisplatin chemotherapy treatment for cancer, those also taking the antidepressants fluoxetine or fluvoxamine were less likely to develop permanent hearing loss or tinnitus. The results suggest these antidepressants could be repurposed to counteract the toxic hearing effects of cisplatin and new medications could be developed based on their molecular effects. (Journal of Investigative Medicine, Apr. 10, 2024)
|
High-protein diets may cause heart problems
 Photo: ©iStock/Yulia Gusterina (04/18/2024)
A team including Pittsburgh and St. Louis VA researchers learned a high-protein diet can cause heart problems by increasing inflammation. The study showed a diet in which more than 22% of the body’s daily calories came from protein increased the levels of the amino acid leucine. This in turn activated blood cells linked to inflammation and increased the risk of atherosclerosis: a buildup of fats, cholesterol, and other substances on the artery walls. The results suggest diets that include more than 25 grams of protein per meal can negatively affect cardiovascular health. (Nature Metabolism, Feb. 19, 2024)
|
Traumatic brain injury may increase brain cancer risk
 Photo: ©iStock/haydenbird (04/18/2024)
VA Salt Lake City researchers and colleagues found traumatic brain injuries (TBI) may be a risk factor for brain cancer in Veterans. Out of nearly 2 million Veterans, those with a moderate to severe TBI were nearly twice as likely to develop brain cancer, while those with a penetrating TBI were more than three times as likely. Veterans with mild TBI had similar rates of brain cancer as those without TBI. Although brain cancer is an uncommon condition, the link between cancer and TBI could put Veterans at greater risk. (JAMA Network Open, Feb. 5, 2024)
|
Cigarette use often increases during military deployments
 Photo: ©iStock/zabelin (04/11/2024)
A study of more than 1,800 Veterans by VA Boston and Puget Sound researchers revealed about 45% of Service members smoked cigarettes during their deployment. Of that 45%, approximately half smoked more often while deployed than when not deployed, and 11% began smoking for the first time while deployed. The study also found that Veterans with multiple deployments were more likely to smoke than those with a single deployment. As expected, those who smoked more cigarettes had poorer lung function later in life. The results showed a need for targeted smoking prevention and cessation efforts among deployed military personnel. (Military Medicine, Mar. 25, 2024)
|
Veterans’ lung cancer survival rates are increasing
 Photo: ©iStock/utah778 (04/11/2024)
A study of nearly 55,000 Veterans showed lung cancer survival is improving in VA. Between the years 2010 and 2017, survival time after cancer diagnosis for VA patients increased for all stages of cancer. For non-small-cell lung cancer, the median survival time increased from 12 to 21 months, with three-year survival increasing from 24% to 28% of patients. For small-cell lung cancer, the median survival time was unchanged but three-year survival increased from 9% to 12%. In 2017, a greater percentage of cancers were diagnosed in stage one, when it is easier to treat. Furthermore, Black Veterans had similar non-small cell survival and higher small-cell survival as White Veterans. The results show improved lung cancer diagnosis and treatment techniques are making a difference for Veterans, and that VA’s equal-access health care system has successfully counteracted the lung cancer racial disparities seen in the general U.S. population. (Clinical Lung Cancer, Mar. 2, 2024)
|
Implanted leg prostheses can improve mobility and reduce back pain
 Photo: ©Vanessa Nunes (04/11/2024)
VA Eastern Colorado researchers and their colleagues showed a leg prosthesis implanted directly to the bone can improve walking and reduce lower back pain in people with amputations. Researchers took a whole-body motion capture of 14 people using traditional prostheses, where the residual limb is fitted into a socket of the prosthesis, and compared it to a second motion capture a year after the same 14 subjects had been implanted with the osseointegrated prostheses. Users showed improved walking mechanics, especially in the back and pelvis areas, and reported significantly less disability on a self-report questionnaire. The results show this kind of implanted leg prosthesis can improve movement coordination over standard prostheses and in turn improve back pain caused by altered spinal loading. (Gait & Posture, Mar. 1, 2024)
|
Michigan VA warns of pneumonia misdiagnoses
 Photo: ©iStock/DragonImages (04/04/2024)
VA researchers in Ann Arbor, Mich., learned that out of a group of 17,000 Michigan patients, 12% of those hospitalized for pneumonia treatments were inappropriately diagnosed. Patients who were older, had dementia, or presented with altered mental states were at the highest risk of being misdiagnosed with pneumonia. Nearly all misdiagnosed patients received a full course of antibiotics, putting them at risk for adverse effects such as allergic reactions and antibiotic-resistant bacteria infection. The results point to a need for improved guidelines on pneumonia diagnosis, especially for older patients. (JAMA Internal Medicine, Mar. 24, 2024)
|
Blast exposure linked to intestinal problems
 U.S. Army photo by Paolo Bovo. (04/04/2024)
A study by New York and Rocky Mountain VA researchers showed blast exposure can cause intestinal permeability, a condition that can lead to gut bacteria entering the bloodstream and causing problems in other parts of the body. Researchers found biomarkers of intestinal permeability in 23 of 30 military “breachers” who were exposed to controlled, low-level explosive blasts during training. Participants also reported headache, dizziness, concentration problems, and slow thinking after blast exposure. Analysis suggested bacterial leakage could add to mild traumatic brain injury to increase mental symptoms. The study was the first to show a connection between blast and intestinal permeability in a real-world operational setting. (International Journal of Molecular Sciences, Mar. 21, 2024)
|
Diabetes medication may increase risk of ketoacidosis
 Photo: ©iStock/Vadym Terelyuk (04/04/2024)
A study by a VA San Diego researcher and colleagues found the medication sotagliflozin may increase the risk of ketoacidosis, a dangerous build-up of acid in the blood, in people with type 1 diabetes. In a group of 1,400 patients taking sotagliflozin, which is used to treat heart failure and improve glycemic control, one-third showed a build-up of beta-hydroxybutyrate, an acid produced in the liver to transport energy when the body does not get enough glucose. The findings highlight the importance of monitoring beta-hydroxybutyrate levels during treatment of patients with type 1 diabetes. (Diabetes Technology & Therapeutics, Mar. 5, 2024)
|
988 suicide hotline rollout increased use of Veterans Crisis Line
 Photo: ©iStock/-zlaki- (03/27/2024)
VA Boston researchers discovered average monthly calls to the Suicide Prevention Hotline increased by 6% for Veterans and 8% overall after the July 2022 rollout of the 988 number. The study also showed the shorter number made it more likely for Veterans who get their health care outside of VA to call, with the overall percentage of callers who are Veterans using a VA health care facility declining by 4%. The results prove the new number increased awareness of the hotline and highlight the potential of national suicide prevention services. (American Journal of Preventive Medicine, Mar. 18, 2024)
|
Stellate ganglion block reduces PTSD symptoms
 Photo for illustrative purposes only. ©iStock/Svitlana Hulko (03/27/2024)
A Providence VA pilot study suggested a stellate ganglion block, an injection of anesthetic medication into a collection of nerves at the base of the neck, can significantly decrease PTSD symptoms when combined with trauma-focused therapy, even in Veterans who do not respond to traditional treatments. Researchers paired this technique with weekly exposure psychotherapy sessions. Participants reported satisfaction with the treatment and only mild, temporary side effects. The study shows a stellate ganglion block holds promise as a new treatment for PTSD. (Psychological Trauma, Mar. 14, 2024)
|
Weight variability increases heart attack, stroke risk
 Photo: ©iStock/gchutka (03/27/2024)
A study of more than 92,000 Veterans who volunteered for the Million Veteran Program revealed large fluctuations in weight significantly raise the risk of cardiovascular events like heart attack, stroke, and death, independent of a person’s overall body mass index (BMI). Analysis of over 65,000 UK Biobank participants confirmed that people with marked weight gain and loss were more likely to die from a cardiovascular event. The results demonstrate a need to monitor BMI variability in addition to treating high BMI. (JAMA Network Open, Mar. 4, 2024)
|
Almost half of Veterans report toxic exposure in military service
 Photo: ©iStock/pixelfusion3d (03/20/2024)
In a study of more than 4,600 Veterans who enrolled at the VA San Diego Healthcare System between 2015 and 2019, nearly 44% reported exposure to environmental toxins during their military service. Exposure to any type of environmental toxin was associated with physical symptoms such as pain, fatigue, and insomnia, as well as psychiatric symptoms such as depression, anxiety, and possibly even PTSD and alcohol misuse. Veterans who experienced combat were more likely to be exposed to toxins than other Veterans. The high prevalence of health problems that can stem from environmental exposures underscores the importance of increased attention and screenings. (Military Medicine, Mar. 4, 2024)
|
Nurse-led strategy improves blood pressure, cholesterol in HIV patients
 Photo: ©iStock/Ake Ngiamsanguan (03/20/2024)
A team including Durham, N.C., VA researchers created a nurse-led program to improve cholesterol and blood pressure control in people with HIV, who are at higher risk for cardiovascular disease. Patients received home blood pressure monitoring guidance and blood pressure and cholesterol management from a dedicated nurse at four in-person visits, along with frequent telephone check-ins, while control patients received general prevention education sessions. The patients in the nurse-led program had significantly lower blood pressure and cholesterol levels after 12 months compared to the control group. The results show this approach can effectively improve cardiovascular risk in HIV-positive patients. (JAMA Network Open, Mar. 4, 2024)
|
Chronic pain more intense in Women Veterans
 Photo: ©iStock/AndreyPopov (03/20/2024)
Minneapolis VA researchers and colleagues found Women Veterans were more likely to have multiple chronic pain conditions, as well as higher pain intensity and more interference with their daily lives. In a group of more than 800 Veterans enrolled in a mindfulness trial for chronic pain, Women Veterans also had higher rates of conditions known to contribute to pain, such as psychiatric conditions, sleep disorders, depression, anxiety, PTSD, fatigue, and stress, but lower levels of pain self-efficacy and participation in social activities. The results highlight a need for pain care that addresses the specific needs of Women Veterans. (Women’s Health Reports, Feb. 12, 2024)
|
Blood pressure control in Veterans declined during COVID-19 pandemic
 Photo: ©iStock/Siarhei Khaletski (03/13/2024)
A multi-institution team led by researchers at the White River Junction VA Medical Center in Vermont found that, in a group of nearly 1.65 million Veterans, 7% had a decline in blood pressure control during the COVID-19 pandemic. Most of the difference was explained by delays in follow-up care in Veterans whose blood pressure had been under control before the pandemic. Conversely, those who had uncontrolled high blood pressure before the pandemic were slightly more likely to gain control during the pandemic, suggesting providers focused more on people with uncontrolled blood pressure during this time. (Medical Care, Mar. 1, 2024)
|
Medical scribes increase VA doctor productivity
 Photo: ©iStock/Ridofranz (03/13/2024)
VA Boston researchers proved medical scribes can increase physicians’ productivity and lower costs in VA specialty care. Twelve VA medical centers participated in a trial program in which scribes were hired to perform documentation and clerical work for physicians for two years. This increased productivity by 30% in cardiology departments and 20% in orthopedic departments. The researchers estimated hiring physicians instead of scribes to achieve the same productivity benefits would cost nearly $1.7 million more. The findings suggest medical scribes could be an effective tool to increase Veterans’ access to care. (Value in Health, Mar. 8, 2024)
|
Number of Veterans receiving community emergency care increasing
 Photo: ©iStock/Wirestock (03/13/2024)
VA Palo Alto researchers learned the percentage of Veterans’ emergency department visits that took place in community hospitals rather than VA facilities increased from 18% in 2016 to 37% in 2022. The study analyzed nearly 20 million emergency department visits by Veterans. The most common reasons for visits were chest pain, abdominal pain, and sepsis. The results suggest policies may be needed to minimize fragmentation of care as more Veterans receive emergency care in the community, paid for by VA, rather than directly from VA facilities. (JAMA Network Open, Mar. 4, 2024)
|
Study reveals genetic link to chronic pain
 Photo: ©iStock/andreswd (03/06/2024)
Philadelphia VA researchers and colleagues identified 126 genetic locations that affect a person’s susceptibility to chronic pain, 69 of which were previously unknown. The genetic study involved nearly 600,000 VA Million Veteran Program (MVP) participants. The analysis also revealed anticonvulsant, beta-blocker, and calcium channel blocker medications all have the potential to be repurposed as a treatment for chronic pain based on their molecular effects. This study improves on the understanding of the genetic component of chronic pain, especially since most genetic pain studies have been limited to people of European ancestry whereas MVP is a more diverse database. (Nature Medicine, Mar. 1, 2024)
|
Black patients may face disparity in lung cancer care
 Photo: ©iStock/ljubaphoto (03/06/2024)
A study led by an Indianapolis VA researcher found racial disparities in diagnosis, treatment, and mortality of lung cancer patients. The study included more than 3,000 non-small cell lung cancer patients treated at a university hospital, 12% of whom were Black. The Black patients were more likely to be diagnosed at a more advanced disease stage, were less likely to receive stage-appropriate treatment, and had a lower five-year survival rate. However, social determinants such as insurance type and marital status explained the disparity rather than just race alone, highlighting the need to address those socioeconomic factors that may prevent Black patients with lung cancer from receiving the care they need. (Translational Lung Cancer Research, Jan. 31, 2024)
|
Transcranial stimulation increases success rate of VR treatment for PTSD
 Photo courtesy of Dr. Noah Philip (03/06/2024)
VA Providence, R.I., researchers showed pairing transcranial stimulation with virtual reality (VR) can improve PTSD symptoms. Veteran volunteers with PTSD received transcranial direct current stimulation, a low-intensity electrical current applied to the brain non-invasively through electrodes to affect the brain’s electrical signals, while viewing a virtual immersion program of Iraq or Afghanistan through a VR headset. Those who received electrical stimulation had more significant decreases in PTSD severity one month after treatment compared to participants who only did the VR training. The results show adding transcranial stimulation to exposure therapy has the potential to improve PTSD treatment. (JAMA Psychiatry, Mar. 6, 2024)
|
VR helps teach mindfulness skills
 Photo: ©iStock/Kobus Louw (02/28/2024)
VA Palo Alto researchers and colleagues demonstrated a self-guided virtual reality (VR) mindfulness program that has the potential to improve substance use disorder treatment. A pilot group of participants from a residential substance use program completed a single session of a self-guided mindfulness lesson designed to help them connect with their thoughts and feelings without distraction. Both patients and providers reported high satisfaction with the program. Participants said the intervention helped them focus attention on the present moment, induced a state of calm and relaxation, and reduced negative thoughts and emotions. They recommended improvements such as better integration of audiovisual elements, a more personalized and longer intervention, and more comfortable VR headsets. The results show VR could be a useful tool to deepen mindfulness skills. (Journal of Substance use and Addiction Treatment, Feb. 18, 2024)
|
Enzyme linked to rheumatoid arthritis increases risk of interstitial lung disease
 Photo: ©iStock/Christoph Burgstedt (02/28/2024)
VA Nebraska-Western Iowa Health Care System researchers and colleagues identified an enzyme that increases the risk of interstitial lung disease in people with rheumatoid arthritis. In a group of more than 2,300 participants with rheumatoid arthritis, those with the highest concentrations of plasma matrix metalloproteinase (an enzyme involved in inflammation) had nearly four times the risk of interstitial lung disease, a condition characterized by scarring of the lungs. The results suggest dysregulation of this enzyme could be responsible for the high rates of interstitial lung disease in rheumatoid arthritis patients and may help with early detection of the lung condition. (Arthritis & Rheumatology, Jan. 25, 2024)
|
Multiple factors linked to loneliness in Veterans with spinal cord injury
 Photo: ©iStock/Edwin Tan (02/28/2024)
Edward Hines, Jr., VA Hospital researchers learned paraplegia, being unmarried, worse general health, sleep problems, bowel dysfunction, and fewer years since injury all independently increased the odds of feeling loneliness. The researchers surveyed nearly 2,500 Veterans with a spinal cord injury. They suggest efforts to address loneliness in paralyzed Veterans should focus specifically on these issues, especially in more recently injured Veterans. (Archives of Physical Medicine and Rehabilitation, Jan. 26, 2024)
|
VA researchers develop potential blood test for schizophrenia
 Photo: ©iStock/peakSTOCK (02/21/2024)
VA Indianapolis researchers and colleagues identified biomarkers that could lead to a blood test for schizophrenia risk. The researchers followed 135 patients with psychiatric conditions for more than a decade to track changes in gene expression linked to hallucinations and delusions. For example, they identified changes in blood levels of multiple enzymes at times when patients reported increased hallucinations or delusions. Testing for these biomarkers could help diagnose and treat schizophrenia, which is often hard to quantify due to the subjective nature of the disease. The results could also lead to the development of new medications targeting the molecular processes involved. (Molecular Psychiatry, Feb. 8, 2024)
|
More than half of antibiotics prescribed by dentists may be unnecessary
 Photo: ©iStock/Alexander Shelegov (02/21/2024)
A study by Edward Hines, Jr., VA Hospital and VA Pittsburgh researchers found 64% of antibiotics prescribed by dentists did not follow prescriptions guidelines. The study examined more than 90,000 antibiotic prescriptions by dentists listed in VA electronic health records for 2019. The most common reason listed for these prescriptions was prevention of post-treatment complications. The results demonstrate a need to reduce unnecessary dental antibiotic prescribing to combat the rise of antibiotic-resistant infections. (Infection Control and Hospital Epidemiology, Feb. 20, 2024)
|
Combat stress can affect brain function decades later
 Photo for illustrative purposes only. ©iStock/DisobeyArt (02/21/2024)
A study using data from VA’s Vietnam-Era Twin Registry showed exposure to combat early in life continues to impact brain function later in life. Researchers compared functional magnetic resonance imaging (MRI) scans to measure brain function in 16 pairs of identical twins in their 60s, of whom only one of each pair experienced combat stress early in life. Forty years after combat exposure, the Veterans showed blunted responses in the amygdala of the brain, while their non-combat-exposed siblings did not. The findings suggest traumatic stress can permanently alter brain function. (Journal of Psychiatric Research, Jan. 16, 2024)
|
Researchers find different biomarkers for alcohol-related, nonalcoholic liver diseases
 Photo: ©iStock/BlackJack3D (02/14/2024)
A study led by a VA San Diego researcher was able to differentiate between alcohol-associated liver disease and nonalcoholic fatty liver disease by fungal gut microbiota. The researchers showed the two types of liver disease cause increases to different species of fungal microbes in fecal matter. They were further able to differentiate between the two diseases at different progressions based on shifting levels in the microbiota. The findings may provide important biomarkers for diagnosing the type of liver disease in unclear cases and could help doctors adjust treatment accordingly. (Gut Microbes, Feb. 1, 2024)
|
Prescription opioids may increase risk of atrial fibrillation
 Photo: ©iStock/radub85 (02/14/2024)
A VA Connecticut study found Veterans prescribed opioids had a nearly 50% higher risk of developing atrial fibrillation, an irregular and often rapid heart rhythm that can lead to blood clots. In a study of more than 600,000 Veterans, the 20% who were prescribed opioids during the five-year study period had an increased the risk of atrial fibrillation whether they were taking immunomodulating or non-immunomodulating opioids. The results suggest opioid use may be a modifiable risk factor for this dangerous heart condition. (American Heart Journal, Feb. 1, 2024)
|
Elder abuse screening inconsistent at VA facilities
 Photo: ©iStock/golfcphoto (02/14/2024)
A nationwide survey of VA facilities showed screenings for elder abuse varied greatly from location to location. Out of 130 medical centers, 48% screen patients of all ages for general abuse or neglect using the current tool, 5% screen using an unstudied or locally developed tool, 4% use a previously published tool, and 44% do not screen for elder abuse at all. These results highlight a need to standardize and improve elder abuse screening in a system that has successfully deployed screening programs for other issues. (Journal of General Internal Medicine, Jan. 8, 2024)
|
Cognitive decline in those with dementia may actually be from cirrhosis
 Photo: ©iStock/Shidlovski (02/08/2024)
A Richmond VA study suggested in some cases the cognitive impairment suffered by people with dementia may actually be caused by undiagnosed liver cirrhosis, which is a treatable condition. In a group of more than 177,000 Veterans diagnosed with dementia, about 5% to 10% had signs of undiagnosed cirrhosis. When the damaged liver does not remove toxins from the blood, it can lead to hepatic encephalopathy, which is a loss of brain function. The researchers recommend patients with dementia be screened for cirrhosis and hepatic encephalopathy, particularly as treating these conditions might reverse the cause of cognitive decline. (JAMA Network Open, Jan. 31, 2024)
|
Interventions may be needed for unstable housing financial assistance to work
 Photo: ©iStock/yavorskiy (02/08/2024)
VA researchers discovered those who received temporary financial assistance from VA’s Supportive Services for Veteran Families (SSVF) program were at the same risk for unstable housing after slightly more than one year as those who did not receive assistance. The study of nearly 35,000 Veterans confirmed the SSVF program does lower Veterans’ risk of unstable housing in the short term, with improvement peaking at approximately 45 days after entering the program, but then decreasing over the months that follow. The results show that while temporary financial assistance can rapidly reduce the risk of unstable housing, additional interventions may be needed to maintain long-term housing stability for Veterans who have exited SSVF. (Health Affairs, Feb. 5, 2024)
|
Memory test could help predict suicide risk
 Photo for illustrative purposes only. ©iStock/Jovanmandic (02/08/2024)
VA New Jersey researchers showed a recognition memory test could help predict an increased risk of suicide. Veterans at a high-risk for suicide completed a computer-based memory test in which they were shown a list of words and then asked to recall which words were on the list after a delay. Several of those with the worst test performances went on to attempt suicide in the next 90 days. Previous research has suggested cognitive changes and memory deficits are connected to suicidal behavior. The findings suggest the test could improve predictions of when at-risk individuals may be transitioning into a period of heightened risk for suicide attempt. (Journal of Affective Disorder, Jan. 12, 2024)
|
Study suggests many ER visits could be resolved by phone
 Photo: ©iStock/Inside Creative House (01/31/2024)
VA Palo Alto researchers learned a VA medical advice line can reduce emergency department visits by connecting callers directly to an emergency care provider. The study analyzed over a million calls to a VA medical advice line over a four-year period. When callers were able to connect directly with an emergency clinician, 65% had their issue resolved or were directed to a less intensive setting for further evaluation. The findings suggest enhancing standard nurse triage phone services with direct patient access to emergency care providers can not only improve Veterans’ care, it can help facilities avoid overcrowding and reduce costs. (Health Affairs Scholar, Dec. 6, 2023)
|
Neural network allows for brain control of multiple devices
 Image: ©iStock/Shutthiphong Chandaeng (01/31/2024)
A team including a Providence VA researcher used an artificial intelligence (AI) neural network to enable a paralyzed user to move two computer cursors simultaneously with a brain-computer interface. Brain-computer interfaces let users move devices such as cursors and prosthetic arms with their thoughts by way of implanted electrodes interpreting brain signals. While all previous brain-computer interfaces have involved controlling a single object, the team was able to train the AI to interpret multiple different commands. With more development, this advance could lead to people with paralysis and amputation being able to control more complex devices such as whole-body exoskeletons or multiple prosthetic limbs. (Scientific Reports, Jan. 18, 2024)
|
Frailty, arthritis medication increase infection risk by 50%
 Photo: ©iStock/towfiqu ahamed (01/31/2024)
A study by VA Puget Sound, Nebraska-Western Iowa, and Philadelphia researchers and colleagues found frailty was linked to a 50% increased risk of serious infection and a 40% higher risk of inpatient admission among patients beginning drug treatment for rheumatoid arthritis. While some rheumatoid arthritis medications have been known to increase the risk of infections, such as pneumonia, by weakening the immune system, this risk appears to be much greater in frail patients. Frailty should be considered when weighing the risks and benefits of these medications. (Arthritis Care and Research, Dec. 20, 2023)
|
Cross-sector networks can better meet Veterans’ needs
 Photo: ©iStock/ferrantraite (01/24/2024)
A study by VA Pittsburgh researchers and colleagues proved patient needs are more likely to be met when cross-sector partnerships between VA medical centers and network programs achieve three conditions: gaining buy-in from health care system users; using a shared referral platform that is accessible to and used by social service organizations; and achieving strong relational coordination to sustain the partnership. The study specifically examined the VA facility’s interaction with AmericaServes, a coordinating program that builds and sustains regional networks of public and private organizations working to support Veterans. The researchers concluded advancing collaboration past the most basic networking level can connect at-risk Veterans with resources to address unmet social needs related to their health and well-being. (Health Services Research, Jan. 22, 2024)
|
Study identifies genetic risk of glaucoma in people of African ancestry
 Photo: ©iStock/Hiraman (01/24/2024)
A study using VA’s Million Veteran Program data identified 46 locations on the human genome related to risk of glaucoma in people of African ancestry. The study, which included more than 11,000 participants of African ancestry, allowed researchers to create a genetic risk score for glaucoma that more accurately predicted the eye disease than a score derived from studies of individuals of European ancestry. The results could lead to targeted treatments for glaucoma, which disproportionately affects people of African ancestry. (Cell, Jan. 18, 2024)
|
Patient portal improves Veterans’ HIV management
(01/24/2024)
VA Palo Alto and Bedford researchers showed the VA patient portal, My HealtheVet, could lead to better health outcomes for Veterans with HIV. In a group of more than 18,000 Veterans living with HIV, use of the prescription refill and secure messaging tools improved antiretroviral medication adherence, while use of the view labs tool was linked to improved viral load suppression. Also, Veterans who used the view appointments tool had an improved viral load test receipt. The results highlight the valuable role the patient portal plays in improving chronic disease management. (Journal of General Internal Medicine, Jan. 22, 2024)
|
Injectable gel could help treat degenerative back pain
 Image: ©iStock/Rasi Bhadramani (01/17/2024)
A team including researchers from the Michael J. Crescenz VA Medical Center in Philadelphia created an injectable gel that shows potential as a treatment for degenerative disc disease. The new substance, a hyaluronic acid granular hydrogel, is made of many microparticles that can be injected easily into the discs between vertebrae to provide cushioning and shock absorption, which could help eliminate back pain in people with degenerative disc disease. The granular nature of the gel allows for improved cell infiltration and lets the material self-repair from friction. The gel also appears opaque under X-ray, allowing for easy monitoring. In animal models, the new gel successfully stopped disc height loss from degeneration and helped maintain disc structural integrity. (Advanced Healthcare Materials, Dec. 23, 2023)
|
Liver infection increases risk of colorectal cancer
 Image: ©iStock/LEOcrafts (01/17/2024)
Iowa City VA researchers showed patients with pyogenic liver abscesses, a type of bacterial infection, were more than twice as likely to develop colorectal cancer. Out of 8,000 Veterans with pyogenic liver abscess, 1.9% developed colorectal cancer in the first three years compared with 0.8% of more than 23,000 Veterans without the infection. The findings suggest patients with this infection should be screened for colorectal cancer. (JAMA Network Open, Dec. 1, 2023)
|
Telehealth palliative care improves quality of life
 Photo: ©iStock/AJ_Watt (01/17/2024)
VA Eastern Colorado and Puget Sound researchers found a nurse and social worker palliative telecare team significantly improved quality of life for Veterans with chronic obstructive pulmonary disease (COPD), heart failure, and interstitial lung disease. The program involved six phone calls with a nurse to help with symptom management and six calls with a social worker to provide psychosocial care over six months, in addition to usual care. As well as quality of life improvements, participants also showed COPD and heart failure health status, depression, and anxiety improvements compared to patients receiving only usual care. (JAMA, Jan. 16, 2024)
|
Alzheimer’s drug may help prevent age-related eye disease
 Photo: ©iStock/Bill Oxford (01/10/2024)
VA researchers from Columbia, South Carolina, found Veterans taking acetylcholinesterase inhibitors, a class of Alzheimer’s disease drug, had a 6% lower risk of the eye disease age-related macular degeneration (AMD) for every year they were on the medication. The study included data from nearly 22,000 Veterans between 55 and 80 years old diagnosed with Alzheimer’s disease. The researchers hypothesize anti-inflammatory properties of the drug may help combat AMD since inflammation is one proposed cause of the eye disease. The findings could lead to new treatments for AMD. (JAMA Ophthalmology, Jan. 4, 2024)
|
Military sexual trauma linked to worse menopause symptoms
 Photo for illustrative purposes only. ©iStock/Highwaystarz-Photography (01/10/2024)
A San Francisco VA study showed female Veterans with a history of military sexual trauma were significantly more likely to experience hot flashes, vaginal symptoms, depression, anxiety, and probable PTSD during menopause. Out of 232 Veterans 45 to 64 years old, 73% reported experiencing military sexual trauma. The results highlight the importance of trauma-informed care and acknowledgment of military sexual trauma across women’s lifespans. (Journal of General Internal Medicine, Nov. 13, 2023)
|
Opioid prescribing linked to heart problems
 Photo: ©iStock/Rattankun Thongbun (01/10/2024)
VA Connecticut researchers learned Veterans with opioid prescriptions had a 16% higher risk of incident cardiovascular disease events, including heart attack, stroke, and angina (chest pain caused by restricted blood flow to the heart). The study included more than 49,000 Veterans, 30% of whom received opioids. The risk of incident cardiovascular disease increased with higher opioid doses. The results show reducing or avoiding opioid prescriptions could help lower cardiovascular risk. (Journal of Pain, Nov. 27, 2023)
|
Liver stiffness could predict liver cancer risk
 Photo: ©iStock/Shidlovski (01/04/2024)
A team including researchers from four different VA systems found liver stiffness can be used to predict liver cancer risk in patients cured of a hepatitis C infection. In the study of 1,850 VA patients, liver cancer risk increased by 3% for every one unit of increased liver stiffness. The study also showed nondiabetic patients with a liver stiffness below five kilopascals were at a low risk of cancer. The findings show measuring liver stiffness could offer a single, easily tested measure of liver cancer risk, identifying which hepatitis C patients no longer require surveillance and which are at an increased risk. (Clinical Gastroenterology and Hepatology, Dec. 5, 2023)
|
Strict cholesterol goals with statin prescriptions can worsen diabetes
 Photo: ©iStock/rogerashford (01/04/2024)
An Orlando VA researcher and colleagues learned strict cholesterol-lowering does not prevent cardiovascular problems better than lenient cholesterol lowering and may even increase diabetes progression. In a group of more than 42,000 Veterans with diabetes who were prescribed statins to lower cholesterol, those with a strict goal of LDL cholesterol below 70 mg/dL and those with a more lenient goal had similar rates of major adverse cardiovascular events, microvascular diabetes complications, and mortality. Those with the stricter cholesterol goal, which often requires higher statin doses, also demonstrated an increased progression of their diabetes. The results suggest more lenient cholesterol goals may protect patients from the potential of statins to worsen diabetes. (Drug Safety, November 2023)
|
Unlike alcohol, substance use does not directly affect PTSD treatments
 Photo: ©iStock/mediaphotos (01/04/2024)
A Minneapolis VA study showed Veterans receiving concurrent, exposure-based PTSD and substance use disorder treatment had improved PTSD symptoms regardless of whether they continued to use substances such as cannabis, cocaine, and opioids. While increased alcohol use was linked to slightly higher PTSD symptoms during treatment, no other substances affected treatment outcomes. Substance use also did not affect treatment discontinuation. The results suggest active substance use during treatment is not directly responsible for the reduced treatment efficacy often seen in Veterans with both PTSD and substance use disorder, meaning other factors such as neurocognitive impairments may be at play. (Journal of Traumatic Stress, Dec. 12, 2023)
|
Both COVID and flu increase long-term health risks, but COVID’s risk is greater
 Photo: ©iStock/AsiaVision (12/19/2023)
VA St. Louis researchers proved COVID-19 confers a higher risk of death and long-term health outcomes than the flu in nearly every organ system. The study included more than 81,000 VA patients admitted to the hospital with COVID-19 and nearly 11,000 admitted with seasonal influenza. Over an 18-month follow-up period, the risk of long-term health problems was only higher from the flu for the pulmonary system. However, both viruses caused a substantial risk in long-term health loss, prompting the researchers to call for greater prevention efforts and more attention to the needs of people with long-term health effects from either COVID-19 or influenza.
(The Lancet Infectious Diseases, Dec. 14, 2023)
|
Study finds link between homeless Veterans and Alzheimer’s disease
 Photo: ©iStock/RapidEye (12/19/2023)
A VA study of more than 88,000 Veterans showed those experiencing housing instability were 53% more likely to have Alzheimer’s disease or related dementia diagnosis. Veterans with stable housing at the beginning of the study who became homeless over the nine-year study period had a higher rate of Alzheimer’s disease than Veterans who did not become homeless, suggesting Alzheimer’s disease is a risk factor for homelessness. The researchers recommended cognitive screenings for homeless Veterans to improve supportive housing services. The study team included VA researchers from Bedford, Massachusetts; Providence, Rhode Island; and Tampa, Florida.
(Journal of the American Geriatric Society, Dec. 6, 2023)
|
Enlarged prostate drug has potential as Parkinson’s disease treatment
 Photo: ©iStock/ExcaliburMedia (12/19/2023)
An Iowa City VA study found a class of medication used to treat enlarged prostate may also delay the progression of Parkinson’s disease. In the study of more than 127,000 Veterans with Parkinson’s disease, those prescribed alpha-1-adrenergic receptor antagonists (AARA) that activate an enzyme called PGK1 had fewer Parkinson’s-related negative events than those taking AARA medication without the PGK1 activation. The results suggest prostate enlargement medications such as terazosin have potential as treatments for Parkinson’s disease, although the researchers caution randomized controlled trials are needed to confirm this effect.
(Journal of the American Pharmacists Association, Dec. 12, 2023)
|
Veterans treated in VA hospitals have lower mortality, readmission
 Photo: ©iStock/monkeybusinessimages (12/18/2023)
VA Palo Alto and Salt Lake City researchers learned Veterans hospitalized in VA medical centers had significantly lower risk of death from heart failure and stroke and lower 30-day hospital readmission for coronary artery bypass graft, gastrointestinal hemorrhage, heart failure, pneumonia, and stroke compared to Veterans in non-VA hospitals. However, Veterans in VA medical centers had longer length of stay and higher costs for most conditions. The study included more than 400,000 Veterans. The findings show VA can offer better care to many Veterans, with the tradeoff of higher resource use. (JAMA Network Open, Dec. 1, 2023)
|
Rural Veterans less likely to use telemedicine
 Photo: ©iStock/fizkes (12/18/2023)
An Iowa City VA study found Veterans living in rural areas were less likely than urban-living Veterans to use telemedicine, even with equal internet access. Out of 350 Veterans surveyed, 96% had in-home internet and 90% had functional connection speeds. Rural Veterans were more likely to rate telemedicine visits as worse than in-person visits. Regardless of where they lived, Veterans recommended technology training and help accessing the internet to improve telemedicine access. The study shows steps beyond infrastructure improvements are needed to increase rural Veterans access and use of telemedicine. (Journal of Rural Health, Nov. 7, 2023)
|
Virtual coaching program can help diabetic patients lose weight
 Photo: ©iStock/Liudmila Chernetska (12/18/2023)
VA Boston researchers showed a virtual coaching intervention combined with a ketogenic diet can reduce body mass index and lower medication usage in patients with diabetes. Participants showed improvements after five months of coaching and eating a very low carbohydrate diet. The intervention also decreased spending on prescription drugs. Blood sugar levels, blood pressure, and health care use were not affected by the intervention. (Diabetes, Obesity & Metabolism, Dec. 11, 2023)
|
Study shows families prefer VA’s end-of-life care
 Photo: ©iStock/Drazen Zigic (12/06/2023)
Family members of Veterans receiving end-of-life hospice care rated VA-run nursing homes substantially better than community nursing homes in a recent survey. Whether the Veterans received care in hospice and palliative care units or in general nursing home units, the VA care was consistently rated as superior. The study also revealed quality gaps in VA-contracted community nursing homes, particularly in areas such as communication, emotional support, management of PTSD, and assistance with VA burial and survivor benefits. The findings highlight the need to address potential inadequacies in non-VA end-of-life care for Veterans. (Journal of the American Geriatric Society, Nov. 10, 2023)
|
Hormone linked to heart failure may predict kidney disease risk
 Image: ©iStock/magicmine (12/06/2023)
A study led by San Francisco VA researchers identified a biomarker that could help monitor kidney function in patients undergoing blood pressure treatment. In a group of more than 8,000 participants of an intensive blood pressure treatment trial, high baseline levels and increases in NT-proBNP, a hormone associated with heart failure, predicted decreases in eGFR, a measure of kidney function. The association was strongest in patients with chronic kidney disease and was independent of changes in blood pressure. Testing NT-proBNP levels may offer a new way to assess kidney disease risk. (American Journal of Kidney Disease, Nov. 20, 2023)
|
Traumatic brain injury linked to recurring episodes of dizziness
 Photo: ©iStock/Antonio_Diaz (12/06/2023)
VA Portland researchers found Service members and Veterans with traumatic brain injuries (TBIs), both from blast exposure and from other causes, were three to four times more likely to report recurring dizziness. Those with blast exposure but no TBI history were not more likely to experience dizziness. The study included 916 Service members and Veterans, about 27% of whom reported dizziness. The findings suggest treatments for TBI-related dizziness do not need to be tailored specifically to the injury mechanism. (Military Medicine, Nov. 8, 2023)
|
Hub-and-spoke program improves access to opioid use disorder medication
 Photo: ©iStock/stevecoleimages (11/29/2023)
VA researchers in Syracuse and Western New York were able to rapidly improve opioid use disorder treatments by creating a central hub specialized in buprenorphine prescriptions with various spoke locations to increase access. In two years, this hub-and-spoke model reached nearly half of the patients in the region with opioid use disorder; of those, 97% had at least one appointment after intake, and 79% received a buprenorphine prescription. Patients in the hub-and-spoke program were more than twice as likely to have a buprenorphine prescription, proving the potential of this system to improve treatment access. (Medical Care, Oct. 6, 2023)
|
Study highlights racial disparities in pancreatic cancer care
 Image: ©iStock/libre de droit (11/29/2023)
A study at the Michael E. DeBakey VA Medical Center, Texas, found Black Veterans were 19% more likely than White Veterans to have late-stage pancreatic cancer and 25% less likely to undergo surgery to remove the cancer. Black Veterans had a higher mortality risk, but this difference was no longer significant after accounting for cancer stage and treatment received. While the extent of racial disparities in pancreatic cancer care are lower in VA than in the general population, likely due to VA’s equal-access care system, the study showed efforts are still needed to address gaps in care. (Pancreas, Nov. 13, 2023)
|
Risk of cannabis use disorder varies by race
 Image: ©iStock/Dr_Microbe (11/29/2023)
A VA Million Veteran Program study revealed multiple new locations on the genome that affect a person’s risk for cannabis use disorder, depending on race: 22 gene loci in people of European descent, two in people of African descent, two in people of East Asian descent, and one in people of mixed ancestry. The study included data on more than a million participants, making it the largest genetic study of cannabis use to date. The researchers also identified a potential link between the genetic risks of cannabis use disorder and lung cancer. The findings shed new light on how cannabis use disorder develops and highlight potential public health consequences of cannabis use. (Nature Genetics, Nov. 20, 2023)
|
Burn pit, environmental exposures could increase breathing problems
 Photo: ©iStock/Solange_Z (11/22/2023)
A VA study of Veterans who served in Afghanistan and Southwest Asia showed exposure to burn pit smoke increased the risk of breathing trouble and chronic bronchitis, while exposure to job-related vapors, dust, or fumes increased the risk of breathing trouble and wheezing. Out of nearly 2,000 Veterans surveyed, 73% reported exposure to burn pit smoke and 72% to other inhaled irritants. Of these Veterans, 7.3% had trouble breathing and 8.2% had chronic bronchitis. The results support the need for post-deployment assessment for a wide range of occupational and environmental exposures to better treat Veterans’ respiratory health. (Occupational and Environmental Medicine, Nov. 15, 2023)
|
Intimate partner violence increases likelihood of age-related, psychiatric disorders
 Photo: ©iStock/ChayTee (11/22/2023)
A San Francisco VA study found intimate partner violence increases the risk of a broad range of age-related and psychiatric health conditions. In a group of nearly 7,000 Veterans, both men and women who experienced intimate partner violence had higher rates of sleep disorder, hypertension, diabetes, and dementia, as well as psychiatric disorders such as depression, PTSD, alcohol use disorder, and substance use disorder. Traumatic brain injury appeared to worsen the symptoms of psychiatric conditions. The findings highlight the importance of addressing intimate partner violence in both men and women Veterans. (Journal of General Internal Medicine, Nov. 14, 2023)
|
Opioid use disorder medication may cause weight gain
 Photo: ©iStock/gchutka (11/22/2023)
Researchers from the Connecticut and Palo Alto, Calif., VA systems learned medication to treat opioid use disorder could lead to moderate weight gain. Veterans taking methadone trended toward about 10 pounds of weight gain over a year of treatment, while those on buprenorphine gained about five pounds in a year. This weight gain is significantly less than gains found in other studies of the two medications, but it may still warrant discussion between doctors and patients beginning opioid use disorder treatment. (Journal of Psychiatric Research, October 13, 2023)
|
Most Veterans continue mental health services after PTSD treatment
 Photo for illustrative purposes only. ©iStock/Drazen Zigic (11/16/2023)
VA Boston and Minneapolis researchers learned nearly all Veterans who completed prolonged exposure or cognitive processing therapy for PTSD continued to use VA mental health services afterward. Of nearly 6,000 Veterans sampled, 98% attended at least one mental health appointment after completing their PTSD treatment, with an average of 28 appointments per patient in the year after treatment. Veterans said they chose to attend additional treatment to continue practicing and applying skills learned in the initial treatment and because they were worried about being able to maintain treatment gains without support. The findings illustrate the need for continued support after primary PTSD treatment ends. (Psychological Services, Nov. 2, 2023)
|
High sodium levels may increase lethality of chronic kidney disease
 Photo: ©iStock/monkeybusinessimages (11/16/2023)
A study led by an Albuquerque VA researcher found increased sodium levels may increase the risk of death in patients hospitalized with chronic kidney disease. In a group of 1.7 million patients analyzed, 6% developed hypernatremia, a high concentration of sodium in the blood that may be caused by impaired kidney function. About 12% of patients with hypernatremia died in the hospital, compared to only 1% without the condition. Those with hypernatremia were also more likely to be discharged to a hospice of nursing facility. The results show a need for increased monitoring and treatment of hospital-acquired hypernatremia, especially in patients with kidney dysfunction. (Clinical Journal of the American Society of Nephrology, Nov. 1, 2023)
|
Insomnia increases risk of heart problems
 Photo: ©iStock/amenic181 (11/16/2023)
A VA Connecticut study showed Veterans with insomnia had a 32% greater risk of atrial fibrillation, an irregular and often rapid heart rhythm that can lead to blood clots, strokes, and even heart failure. The researchers analyzed the medical records of more than a million Veterans, a little over 4,000 of whom developed atrial fibrillation between 2001 and 2017. The link between insomnia and atrial fibrillation persisted after accounting for obstructive sleep apnea, a well-known risk factor for atrial fibrillation. The results suggest screening for insomnia is important to protect Veterans from future heart problems. (Journal of the American Health Association, Oct. 17, 2023)
|
VA’s COVID-19 genomic surveillance programs expand to new scale
 Image: ©iStock/peterschreiber.media (11/08/2023)
Two VA programs created for the COVID-19 response are now leveraging their role in the country’s largest integrated health care system to enable the study of diseases and pandemics at an unprecedented scale. Sequencing for Research Clinical and Epidemiology (SeqFORCE) allowed VA to perform genetic sequencing of samples from Veterans and employees with COVID-19 to understand patterns of virus variant evolution, vaccine and treatment response, health care-associated outbreaks, and virus transmission. Sequencing Collaborations United for Research and Epidemiology (SeqCURE) studied the COVID-19 genome to understand how the virus functions and how best to combat it. How these two consortia focused on genetic COVID-19 surveillance to understand and track the changing situation of the pandemic – and how they have evolved post-pandemic – is described in detail in a special edition of the Federal Practitioner, November 2023.
|
Peer-supported mobile program may improve Veterans’ mental health
 Photo: ©iStock/LaylaBird (11/08/2023)
VA Palo Alto and Syracuse researchers showed a peer-supported mobile health program can improve Veterans’ stress levels and help them progress on personal health goals. In the pilot study, 39 Veterans with depression who were not currently in mental health treatment participated in four phone sessions with a peer over eight weeks. They were also introduced to mobile apps designed to help with mental health issues. Participants used an average of three of the apps and were highly satisfied with the program. The researchers recommend a larger clinical trial of the intervention to test how it can reduce depression symptoms. (Psychological Services, November 2023)
|
VA’s 3D printed nasal swab study proves collaboration can address supply shortages
 Photo: ©iStock/hobo_018 (11/08/2023)
During the COVID-19 pandemic, the VA Office of Research and Development and the Office of Healthcare Innovation and Learning launched a study to evaluate the safety and efficacy of 3D-printed nasal testing swabs to mitigate supply shortages. The trial yielded two production processes and identified which swab designs were as safe and effective as standard tests. The successful trial showed how close collaboration between VA researchers and government, industry, and academic partners can help to prepare for and respond to national health crises. (Federal Practitioner, November 2023)
|
Homeless Veterans at risk for dangerous benzodiazepine, opioid prescriptions
 Photo: ©iStock/bieshutterb (11/02/2023)
A VA National Center on Homelessness Among Veterans study found homeless Veterans were more likely to have a dangerous combination of both benzodiazepine and opioid prescriptions. The study compared more than 240,000 homeless Veterans who used VA mental health services to nearly one million non-homeless Veterans. The study also found homeless Veterans were less likely to be prescribed benzodiazepine overall, but those who were prescribed the drug were more likely to have multiple concurrent prescriptions. These findings suggest a need for doctors to be careful when prescribing benzodiazepine to homeless Veterans. (Psychiatric Services, Oct. 31, 2023)
|
Loud noises can cause tinnitus through synapse damage
 Photo: ©iStock/Daria Kulkova (11/02/2023)
VA Portland researchers believe they have discovered how loud noises cause tinnitus. After finding Veterans with tinnitus may have the equivalent amount of inner-ear synapse loss as 20 years of aging, investigators theorize loud noise can permanently damage the synapses, resulting in tinnitus. Although the number of synapses in the cochlea cannot be directly measured in living humans, the researchers used hearing-based physiological measures that have shown to be good indicators of synapse loss. Veterans with normal hearing tests who experienced tinnitus performed worse on two such tests when compared with non-Veterans. (Journal of Speech, Language, and Hearing Research, Oct. 27, 2023)
|
Financial housing aid reduced Veterans’ suicidal ideations
 Photo: ©iStock/Hispanolistic (11/02/2023)
A recent VA study of the VA Supportive Services for Veteran Families program found enrollment in the program’s rapid re-housing component was the main driver of risk improvement in all-cause mortality and suicidal thoughts. The researchers analyzed data on nearly 42,000 Veterans enrolled in the program between 2015 and 2018, many of whom were facing housing instability. While the temporary financial aid did not affect the number of suicide attempts, the results of the study show housing assistance can improve Veterans’ mental and physical health. (Journal of General Internal Medicine, Oct. 26, 2023)
|
New AI program predicts irregular heart rhythm
 Image: ©iStock/natrot (10/25/2023)
San Francisco VA researchers and colleagues developed a computer algorithm with the potential to detect the irregular heart rhythm called atrial fibrillation a month before it occurs using electrocardiogram (ECG) data. To train the artificial intelligence program, researchers entered nearly one million ECG scans from six VA facilities and one non-VA facility into the computer system. The program proved accurate at predicting atrial fibrillation within 31 days even across diverse demographics and patient conditions. The algorithm could help doctors find which patients are at risk for atrial fibrillation and take preventative steps before problems develop. (JAMA Cardiology, Oct. 18, 2023)
|
Veterans switch colonoscopies to non-VA providers after MISSION Act
 Photo: ©iStock/Vadym Terelyuk (10/25/2023)
VA researchers in Houston learned VA’s share of colorectal cancer screening decreased as many Veterans received colonoscopies from non-VA providers after implementation of the MISSION Act. While the source of colonoscopies shifted, the total number of colonoscopies did not change, meaning the MISSION Act did not increase overall screening. Veterans who lived the farthest away from VA facilities were most likely to receive non-VA colonoscopies. The findings show VA-purchased care may increase access to health care services, but the researchers caution it may be necessary to increase care coordination and efforts to ensure quality of care as a result. (Health Services Research, Sept. 26, 2023)
|
Many Veterans require childcare assistance during health care visits
 Photo: ©iStock/Halfpoint (10/25/2023)
In a survey of 2,000 Veterans using VA health care, more than 75% stated they needed childcare assistance during health care appointments and childcare problems compromised their quality of care. Nearly 58% of those surveyed had missed or canceled VA health care appointments because they could not find childcare, and 35% reported bringing their children with them to appointments. Survey participants explained how having their children present during appointments hampered communication with health care providers. The findings highlight the need for a national childcare assistance program in VA, implementation of which is underway. The study group included VA researchers from Durham, Greater Los Angeles, and Washington, D.C. (Women’s Health Issues, Oct. 12, 2023)
|
Gene variant protects against kidney disease in Black Veterans
 Image: ©iStock/Rasi Bhadramani (10/19/2023)
VA Million Veteran Program researchers discovered a gene mutation that lowers the risk of chronic kidney disease and kidney failure in Black patients. In a genetic study of more than 120,000 Veterans with African ancestry, Veterans with specific mutations of the APOL1 gene – particularly common in people of African ancestry – had an increased risk of kidney disease. But a different gene variation actually reduced the risk in people with the risky APOL1 variant. The discovery could lead to medications that mimic the protective gene’s effects, protecting people from kidney problems. (Journal of the American Society of Nephrology, Oct. 6, 2023)
|
Disrupted care during pandemic likely led to excess deaths
 Photo: ©iStock/Ridofranz (10/19/2023)
An analysis of nearly 6 million VA health care patients revealed excess mortality, a measure of additional deaths beyond expected numbers, increased during the COVID-19 pandemic even after accounting for direct COVID-related deaths. Older people and those with more health conditions had a higher risk of death during the pandemic, but younger and healthier people experienced a greater change in excess mortality rates. The fact that excess deaths remained elevated for many groups, even after patients diagnosed with COVID-19 were removed, emphasizes societal and health care disruptions caused by the pandemic likely led to even more deaths. The study group included researchers from the White River Junction, Palo Alto, and Connecticut VA health care systems. (International Journal of Epidemiology, Oct. 6, 2023)
|
Rural Veterans with HIV and alcohol use disorder receive less video telehealth
 Photo: ©iStock (10/19/2023)
Researchers at the Michael E. DeBakey VA Medical Center in Houston learned rural Veterans with HIV and alcohol use disorder receive less video telehealth services than their urban counterparts. Veterans with both conditions living in either rural or urban locations received similar face-to-face and phone treatment. The results suggest a need to increase access and improve the uptake of video-based mental health treatment in this vulnerable population to ensure equal access to care. (Journal of Rural Health, Sept. 27, 2023)
|
Bright light therapy improves sleep in people with sleep apnea
 Photo: ©iStock/oatawa (10/10/2023)
In a pilot study, Pittsburgh VA researchers showed morning bright light therapy can improve sleep and reduce daytime sleepiness and depression symptoms in people with obstructive sleep apnea. For four weeks, participants with continuous positive airway pressure (CPAP)-resistant sleep apnea were exposed to bright green-blue light in the morning via special glasses, resulting in improved sleep-wake cycles. The researchers believe bright light therapy can be a safe and inexpensive way to reset circadian rhythms and help patients with sleep apnea. (Journal of Clinical Sleep Medicine, Sept. 28, 2023)
|
Smallpox vaccines reduce risk of mpox
 Photo: ©iStock/Hailshadow (10/10/2023)
VA researchers found smallpox vaccines were between 72% to 75% effective at preventing mpox (formerly called monkeypox). The study analyzed data on Service members and Veterans who received a smallpox vaccination as a routine part of their military deployment. Out of nearly 300 military members who tested positive for mpox in 2022, only 20 had received a smallpox vaccine. The findings suggest existing smallpox vaccines could be an effective way to defend against the ongoing mpox global outbreak. (New England Journal of Medicine, Sept. 21, 2023)
|
Biomarker of metabolic dysfunction linked to worsening asthma
 Photo: ©iStock/PixelsEffect (10/10/2023)
Researchers from the Michael E. DeBakey VA Medical Center in Houston, TX, found elevated levels of triglyceride-glucose index, a measure of metabolic conditions such as diabetes, are a risk factor for worsening asthma. The study included more than 100,000 Veterans receiving asthma care from VA. The results suggest triglyceride-glucose index could be used as a biomarker for patients who may need more intensive asthma treatment and support the idea that metabolic dysfunction can severely exasperate asthma. (Journal of Allergy and Clinical Immunology, Sept. 14, 2023)
|
Largest-ever genetic study of suicide finds genetic risk factors
 Image: ©iStock/Dr_Microbe (10/05/2023)
In the largest-ever genetic study of suicide, researchers identified 12 gene variants that increase the risk of suicide attempts. The international study used data from VA’s Million Veteran Program and the International Suicide Genetics Consortium to analyze the genomes of more than 43,000 people with documented suicide attempts and 915,000 controls without a history of suicidal behavior. The findings showed suicide attempts share genetic risk factors with several other conditions, such as attention deficit hyperactivity disorder, smoking, and risk tolerance, which is associated with engaging in dangerous behavior. The results increase understanding of the biological causes of suicide and could lead to improved suicide prevention and treatment. (American Journal of Psychiatry, Oct. 1, 2023)
|
PTSD, alcohol use disorder can speed up aging
 Photo: ©iStock/Christogra4 (10/05/2023)
VA Boston researchers showed PTSD and alcohol use disorder symptoms cumulatively cause human cells to age at a faster rate than would be expected based on chronological age alone, meaning the longer a person has one of the conditions the greater the deterioration of their cells would be. The results provide insights into the biological effects of these conditions and may help lead to interventions to slow accelerated aging. (Journal of Mood and Anxiety Disorder, Sept. 22, 2023)
|
Sleep breathing problems lengthen hospitalizations, but effect on mortality varies
 Photo: ©iStock/cherrybeans (10/05/2023)
A Louis Stokes Cleveland VA Medical Center researcher learned hospitalized patients with obesity hypoventilation syndrome or obstructive sleep apnea had longer lengths of stay and larger hospital costs, but the two conditions had opposite effects on mortality. In an analysis of more than 6 million hospitalized patients, those with obesity hypoventilation syndrome had a higher risk of death, but those with obstructive sleep apnea actually had a lower risk of death. The researcher theorized the lower mortality of obstructive sleep apnea patients may be due to a higher sense of vigilance than for patients with undiagnosed sleep disordered breathing. (Annals of the American Thoracic Society, Sept. 25, 2023)
|
Antidepressant discontinuation common during pregnancy
 Photo: ©iStock/PeopleImages (09/27/2023)
A study led by a Michael E. DeBakey VA Medical Center researcher found, of Veterans with mental health disorders who became pregnant, only 34% continued using antidepressants through the pregnancy. About 31% chose to stop taking antidepressants on their own, while 31% had antidepressants discontinued by their doctors. Veterans with past suicidal behavior and more severe mental health diagnoses were more likely to stop taking the medication. The findings suggest a need in VA for education on risks and benefits regarding antidepressant use during pregnancy, as well as availability of alternative therapies. (Archives of Women’s Mental Health, Sept. 23, 2023)
|
Video-enabled tablets increase mental health access for older Veterans
 Photo: ©iStock/Ridofranz (09/27/2023)
VA Palo Alto researchers learned providing video-enabled tablets helps older Veterans with alcohol use disorder overcome barriers to mental health services. More than 11,000 Veterans aged 60 or older with alcohol use disorder were given tablets to access telehealth mental health services like video visits, which increased from 8.7% to 26.2%. Veterans who were older, male, and had more physical health conditions were less likely to use video visits. Those who were married, lived in urban areas, had a history of housing instability, and had more mental health conditions were more likely to use video visits. The results show that video-enabled tablets can increase mental health access, but more support may be needed to help certain groups use the technology. (Aging & Mental Health, Sept. 18, 2023)
|
Anemia treatment may increase risk of kidney disease
 Photo: ©iStock/PeopleImages (09/27/2023)
A study by Memphis and Long Beach VA researchers and colleagues found that oral iron treatments for anemia are associated with increased risk of chronic kidney disease. In a study of nearly 150,000 Veterans, those taking iron supplements had a significantly higher risk of new-onset kidney disease and worse measures of kidney function. The researchers hypothesize oral iron could harm the gut microbiome and lead to kidney damage. The results reveal a need to monitor patients on iron replacement therapy for kidney function. (European Journal of Haematology, Sept. 5, 2023)
|
Adding suicide prevention to addiction treatment prevents rise in ideations
 Photo: ©iStock/Marco VDM (09/20/2023)
A White River Junction pilot trial for the VA Brief Intervention and Contact Program (VA BIC) showed improvements in suicidal ideation and perceived burdensomeness among Veterans completing addiction treatment, while those receiving only the standard care worsened in both measures. All the Veterans in the trial were participating in a 28-day in-patient substance use disorder program, which also involves an educational session and follow-up contacts over several months to encourage treatment engagement and self-efficacy. Those in the VA BIC group also had modest improvements in treatment engagement after discharge. The results suggest that VA BIC could be a useful addition to addiction treatments to increase participation and prevent suicide. (Journal of Substance Use and Addiction Treatment, Aug. 29, 2023)
|
Pittsburgh study finds racial, gender disparities in prescriptions of cholesterol medication
 Photo: ©iStock/rogerashford (09/20/2023)
VA Pittsburgh researchers discovered racial and gender disparities in prescriptions for statin, a drug used to reduce cholesterol. In a nationally representative group of patients eligible for statin, Black men and women, multiracial men, Hispanic women, and White women all had lower rates of being prescribed statin than White men. Neither disease severity nor structural factors such as health insurance or income played a role in the difference. The results highlight the need to address systemic problems like bias, stereotyping, and mistrust to counteract health disparities. (Annals of Internal Medicine, August 2023)
|
Self-efficacy training could improve chronic pain care for Black Veterans
 Photo: ©iStock/IURII KRASILNIKOV (09/20/2023)
Self-efficacy refers to a person’s belief in their capacity to execute behaviors necessary to reach a certain goal, and it is often a reflection of their own self-confidence. Indianapolis VA researchers and colleagues found interventions to increase patient self-efficacy can also improve chronic pain treatment among Black Veterans. The Communication and Activation in Pain to Enhance Relationships and Treat Pain with Equity (COOPERATE) intervention is a patient-centered program that aims to increase patients’ knowledge and confidence to manage their own health. Black Veterans participating in COOPERATE described feeling more confident and able to take ownership of their pain care after the program, which led to improved pain management. Participants cultivated skills such as preparing a list of questions before an appointment, expressing concerns effectively, and communicating about goals, values, and preferences. The researchers concluded that COOPERATE is a promising approach to address racial disparities in pain care. (Journal of General Internal Medicine, Sept. 19, 2023)
|
TBI increases suicide risk directly and indirectly
 Photo: ©iStock/jaminwell (09/13/2023)
A VHA Rocky Mountain Mental Illness Research Education and Clinical Center study showed that traumatic brain injury (TBI) both directly and indirectly increases suicide risk. Researchers studied data on more than 860,000 U.S. Soldiers, 12.6% of whom had at least one TBI documented on their military health record. Those who experienced a TBI had significantly higher rates of new-onset mental health conditions. Analysis showed that TBI both directly increased suicide risk and indirectly increased risk by increasing the likelihood of mental health conditions. TBI-related substance use disorder was the greatest contributor to increased suicide risk. The findings highlight a need to monitor both the primary and secondary effects of TBI to prevent suicide. (JAMA Network Open, July 3, 2023)
|
At-home cardiovascular rehabilitation can improve heart health
 Photo: ©iStock/AsiaVision (09/13/2023)
Atlanta VA researchers found that remote cardiac rehabilitation can reduce cardiovascular risk and increase healthy behaviors. Patients with heart problems were offered a digital health intervention consisting of a three-month home exercise program enhanced with a smartphone app, coaching, and a wearable activity tracker. Patients using the program showed significant improvements in heart health and cholesterol measures, as well as decreases in smoking. However, only 16% of patients referred to cardiovascular rehabilitation consented to using the digital health intervention. The results show that at-home, digital cardiovascular rehabilitation can help Veterans with heart conditions, but more work is needed to get patients to accept the technology. (BMC Cardiovascular Disorders, Sept. 12, 2023)
|
Insomnia, alcohol use disorder share genetic risk factors
 Photo: ©iStock/Filmstax (09/13/2023)
A VA Million Veteran Program study found that genetic risk factors for insomnia may also increase risk of alcohol use disorder. Using data from the largest available genome-wide association studies of insomnia, sleep duration, and alcohol use disorder, the researchers found that insomnia and alcohol use disorder shared overlapping genetic risk traits. Analysis showed insomnia and alcohol use disorder share a symbiotic relationship, with each condition increasing the risk of the other. The findings suggest that treating both disorders at the same time could be an effective way to treat these related conditions. (Drug and Alcohol Dependence, July 27, 2023)
|
Tryptophan may protect against hip fractures
 Photo: ©iStock/fotostorm (08/28/2023)
A study led by VA researchers in Augusta, Georgia, suggested the amino acid tryptophan could help prevent hip fractures in older adults. The researchers analyzed the blood of study participants and examined their health outcomes for 12 years. During that time period, those with higher levels of tryptophan in their blood had a significantly lower risk of hip fractures, but similar risk for mortality or frailty. The results suggest that tryptophan supplementation could support bone health and help prevent fractures, although optimal intake amounts would need to be studied. (JBMR Plus, Aug. 18, 2023)
|
Self-injury more than twice as likely in Gulf War Veterans who experienced military sexual assault
 Photo: ©iStock/kitzcorner (08/28/2023)
A Durham VA study showed that Gulf War-era Veterans who experienced military sexual assault were two-and-a-half times more likely to engage in nonsuicidal self-injury. In more than 1,000 Veterans assessed, this association remained true after controlling for related demographic and medical factors. Self-injury was strongly associated with probable PTSD, but the link between military sexual assault and self-injury was present even in Veterans without probably PTSD. The findings highlight the importance of screening for self-injury in Veterans who experience military sexual trauma. (Military Psychology, June 9, 2023)
|
Majority of Veterans with TBI use both community and VA care
 Photo: ©iStock/shapecharge (08/28/2023)
A study by VA Portland researchers and their colleagues found VA-purchased community care use is common for Veterans with traumatic brain injury (TBI). Out of more than 65,000 Veterans with TBI, 51% used community health care paid for by VA during the four-year study period. Nearly all also used VA-delivered care during the same period. Veterans with more severe TBI, those with higher health risk scores, and those with PTSD, depression, anxiety, substance use disorder, or pain-related conditions were more likely to use community care, along with those with high risk of suicide. The researchers concluded that more research is needed on the best ways to balance greater access to care with potential care fragmentation among Veterans with TBI. (Journal of Head Trauma Rehabilitation, Aug. 14, 2023)
|
Suicide rates higher in western U.S.
 Photo: ©iStock/Grand Warzawski (08/17/2023)
Researchers from VA Rocky Mountain Mental Illness Research, Education, and Clinical Center for Veteran Suicide Prevention (MIRECC) and their colleagues learned suicide rates are higher in western parts of the country. The researchers analyzed Centers for Disease Control and Prevention data from nearly 3,000 counties across the United States and found counties in the western U.S. had up to two additional deaths each year per 100,000 people, compared to eastern counties. The researchers theorize a misalignment between circadian rhythm and exposure to daylight caused by time zone differences and daylight savings time could increase the risk of suicide. (Journal of Affective Disorders, July 20, 2023)
|
Disparity in opioid prescriptions can put all ethnic groups at risk
 Photo: ©iStock/Bet_Noire (08/17/2023)
A VA Pittsburgh analysis of VA electronic health records found Non-Hispanic White Veterans were more likely than all other racial and ethnic groups – except American Indian/Alaskan Native Veterans – to receive opioid prescriptions. The study also found about 15% of Veterans receive an opioid prescription, with White Veterans having higher odds of having overlapped opioid prescriptions and high-dose prescriptions. White Veterans had the highest odds of opioid-benzodiazepine prescription overlap, which can be a dangerous combination. The results show a need to examine disparities in opioid prescribing, both for possible undertreatment of pain in minority Veterans and high-risk overprescribing in White Veterans. (American Journal of Preventative Medicine, June 10, 2023)
|
Veterans in disadvantaged neighborhoods at higher risk for dementia
 Photo: ©iStock/DenisTangneyJr (08/17/2023)
A study led by a San Francisco VA researcher suggests that Veterans who live in disadvantaged neighborhoods have an increased risk for dementia. The research team looked at VA data on more than 1.6 million Veterans from between 1999 and 2021. During an average follow-up of 11 years, Veterans who lived in areas with a higher Area Deprivation Index – a scale that quantifies neighborhood disadvantage based on income, education, employment, and housing – were more likely to develop dementia than Veterans living in more affluent areas. The results suggest that socioeconomic factors can negatively affect brain health even among Veterans with equal access to health care. (JAMA Neurology, July 19, 2023)
|
Tinnitus has exponentially negative impacts on Veterans’ ability to work
 Photo: ©iStock/Aleksej Sarifulin (08/10/2023)
A study by VA Portland researchers showed that every one-point increase on a measure of tinnitus severity (ringing in the ears) corresponded to an 8% increase in the odds of high-level interference with work functioning. The study examined a nationally representative group of Veterans, and while researchers also found Veterans with traumatic brain injury (TBI) were more likely to have tinnitus impact their work, the relationship between tinnitus and work impairments persisted in both Veterans with and without TBI. The findings suggest that tinnitus therapies may need to include vocational rehabilitation services. (Seminars in Hearing, July 24, 2023)
|
Colorado VA collaborates with community to improve suicide prevention
 Photo: ©iStock/dragana991 (08/10/2023)
VA researchers in Colorado partnered with 13 community organizations to implement 92 Veteran suicide prevention program components as part of a 16-month long learning collaborative. The program had a large footprint, interacting with more than 24,000 community members who serve, interact with, or employ more than 5,000 Veterans in the Denver and Colorado Springs area. Suicide prevention components included distribution of suicide prevention materials, staff training, and Veteran mental health screenings. The pilot proves that community collaboration can lead to rapid implementation of Veteran suicide prevention practices, even across an entire city. (Suicide & Life Threatening Behavior, July 21, 2023)
|
Aromatherapy eases end-of-life cancer pain
 Photo: ©iStock/dragana991 (08/10/2023)
A pilot study by researchers at the John D. Dingell VA Medical Center in Detroit suggested aromatherapy may help ease pain in cancer patients near the end of their lives. Veterans in hospice care answered questions about their pain levels before and after receiving aromatherapy. Fifteen minutes after aromatherapy treatment, Veterans had lower self-reported pain scores. The need for opioid pain medication also decreased after aromatherapy. Participants said they found the aromatherapy to be soothing and described a decreased pain experience, with most participants wanting to continue receiving aromatherapy. The researchers concluded that aromatherapy could be an effective complementary treatment for end-of-life cancer pain. (Clinical Journal of Oncology Nursing, August 1, 2023)
|
VA, firearm retailers partner to promote safe gun storage
 Photo: ©iStock/M-Production (08/02/2023)
VA researchers in New Orleans collaborated with firearm retailers to create an out-of-home firearm storage program that reduces Veteran suicide rates by limiting rapid access to firearms during periods of emotional crisis. VA and three firearm retailers developed a program in which Veterans would voluntarily store their firearms at gun shops. The four-month pilot showed that the program was feasible and acceptable to firearm retailers and their staff. The program also led to changes in staff beliefs regarding the role of secure firearm storage in suicide prevention. Storage of customers’ firearms, conversations about secure storage, and dispersal of materials about out-of-home storage all increased as well. The results suggest that by partnering with the gun retail community, VA can encourage safer firearm storage practices among Veterans at risk for suicide. (Suicide & Life Threatening Behavior, July 14, 2023)
|
Traumatic brain injury increases risk of suicide and mental health conditions
 Photo: ©iStock/zim286 (08/02/2023)
A study by VA Rocky Mountain Mental Illness Research Education and Clinical Center researchers showed that suicide and mental health conditions can be linked to a traumatic brain injury (TBI). The study included data from more than 860,000 soldiers, 12.6% of whom had at least one documented TBI. Researchers noted a history of TBI both directly and indirectly increased the risk of suicide. Rates of new-onset mental health conditions such as anxiety, posttraumatic stress, and substance use disorder were also higher in soldiers with TBI. The researchers concluded that TBI should be considered a risk indicator for suicide and mental health issues that can accumulate over an individual’s lifetime. (JAMA Network Open, July 3, 2023)
|
Rheumatoid arthritis increases risk of heart valve problems
 Photo: ©iStock/Shidlovski (08/02/2023)
A team including researchers from VA health care systems in Philadelphia, Salt Lake City, and Nebraska-Western Iowa learned that rheumatoid arthritis increases the risk of aortic stenosis – a narrowing of the aortic valve that causes the heart’s left ventricle to work harder. Using VA and Medicare data, the researchers compared more than 70,000 patients with rheumatoid arthritis with more than 600,000 patients without. Those with arthritis had a 48% higher risk of aortic stenosis, as well as higher risk of heart surgery and death. The findings suggest that heart valve problems may be an understudied complication of rheumatoid arthritis. (JAMA Internal Medicine, July 31, 2023)
|
Diabetes medicine may reduce heart and kidney damage from cardiac arrest
 Photo: ©Boston VA Medical Center (07/27/2023)
Pittsburgh VA researchers discovered diabetic patients taking Metformin had less evidence of damage to the heart and kidneys after an incident of cardiac arrest. As the high mortality rate of cardiac arrest stems from the multi-system organ damage, VA researchers tested metformin and found that two weeks of pretreatment protected blood flow in both the heart and kidneys, even in non-diabetic cases. Despite the positive impacts of pretreatment, the drug had no effect when used during or after resuscitation. The researchers theorize that metformin’s activation of the Adenosine Monophosphate-Activated Protein Kinase (AMPK), a fuel-sensing enzyme present in the cells of all mammals, is what provided the extra protection. The study shows that while metformin could work well as a form of pretreatment, it would not work as a rescue therapy. (Journal of Molecular and Cellular Cardiology Plus, June 1, 2023)
|
Social and mental quality of life is key to Veterans’ reintegration to civilian life
 Photo: ©Getty Images/ Drazen Zigic (07/27/2023)
Researchers from the Richard L. Roudebush VA Medical Center in Indianapolis found that post-9/11 Veterans with social support networks and a higher mental health-related quality of life had less difficulty reintegrating into civilian life, even when they had cognitive or mental health conditions. Researchers studied data from the standardized measures of 75 Veterans to investigate possible connections between reintegration difficulties and their health and well-being outcomes. They found that reintegration difficulties were often associated with low functioning mental health and lower social support, while those reporting fewer perceived limitations with reintegration attended more medical appointments and were positively associated with social support. Findings from this study suggest that post-9/11 Veterans with mental health or cognitive conditions can have an easier transition out of the military if they maintain social networks and invest time into their mental health. (Journal of Veteran Studies, July 5, 2023)
|
Vets with complex health conditions more likely to abuse alcohol, but less likely to be treated for it
 Photo: ©Getty Images/Dani DG (07/19/2023)
A study by Pittsburgh VA researchers found that Veterans with more complex medical conditions may face disparities in care for unhealthy alcohol use. The researchers looked at data for more than 280,000 Veterans who received primary care from VA, about 4% of whom screened positive for unhealthy alcohol use. Those with multiple chronic health conditions and at high-risk of hospitalization were slightly less likely to screen positive for unhealthy alcohol use compared to low-complexity patients. However, high-complexity patients were more likely to have more severe alcohol use and were less likely to receive a brief intervention treatment. Factors such as competing medical demands, lack of resources, and lack of provider knowledge may partially explain this health disparity. (Journal of Substance Use and Addiction Treatment, June 23, 2023)
|
Diabetes genetic risk linked to dementia risk
 Image: ©Getty Images/Shutter2U (07/19/2023)
A VA Million Veteran Program study suggested that diabetes may play a role in the development of dementia. Researchers analyzed genetic data from more than 330,000 Veterans with type 2 diabetes. They found that when Black or White Veterans has a genetic predictor of diabetes, they also had greater odds of being diagnosed with dementia, and the risk of dementia increased with more diabetes predictors. However, this connection did not occur in Hispanic Veterans. The findings suggest that diabetes prevention efforts could also help lower the risk of dementia. (Alzheimer’s & Dementia, July 7, 2023)
|
Herpes antibodies may partly protect against shingles
 Image: ©Getty Images/Dr_Microbe (07/19/2023)
A study by VA San Diego researchers and colleagues showed that prior infection with the herpes simplex virus, which is commonly spread by oral or genital contact, partly protects against the herpes zoster virus, better known as shingles. Researchers tested the blood of participants for antibodies of herpes simplex, and found that those without herpes simplex antibodies were significantly more likely to test positive for herpes zoster. The findings suggest that the decrease of herpes simplex prevalence in recent years may be tied to increasing cases of shingles. (Journal of Infectious Diseases, July 6, 2023)
|
New AI algorithm improves suicide prediction model
 Photo: ©Getty Images (07/12/2023)
VA White River Junction researchers created an artificial intelligence algorithm to improve suicide risk prediction from Veterans’ electronic health records. The researchers used natural language processing to look for suicide risk factors in unstructured electronic health records data, such as clinical notes. The prediction model was 19% more accurate than a model that strictly used structured health records data, where clinicians enter information such as diagnoses, demographic data, and medications into specific fields. The new model was even more accurate for the patients at highest risk. The findings suggest that adding unstructured data to suicide prediction models already in use can better identify Veterans at risk. (Journal of Clinical Psychiatry, June 19, 2023)
|
Dog ownership linked to lower blood pressure, cholesterol
 Photo: ©Getty Images/hobo_018 (07/12/2023)
Researchers from the Palo Alto and Connecticut VA health care systems learned dog ownership may promote heart health in Veterans. In a group of more than 3,000 Veterans, dog ownership was linked to lower odds of high blood pressure and high cholesterol, while cat ownership was not. Dog ownership was also indirectly linked to lower odds of heart disease because dog owners tended to get more exercise. However, older Veterans who owned dogs had higher odds of diabetes and stroke than those who did not have dogs. The researchers conclude that dog ownership could provide heart-related health benefits, but more research is needed on possible negative effects for some groups. (Scientific Reports, July 8, 2023)
|
Most Veterans with PTSD delay psychotherapy treatment
 Photo for illustrative purposes only. ©Getty Images/SDI Productions (07/12/2023)
Researchers from the Portland and White River Junction VA health care systems found that few patients with PTSD begin evidence-based psychotherapy treatment within the first year of diagnosis. Out of more than 260,000 Veterans who began PTSD treatment in a VA facility between 2017 and 2019, only 11.6% started psychotherapy during their first year of treatment. Older patients were less likely to initiate psychotherapy but more likely to receive an adequate treatment dose when they did initiate. Black, Hispanic, and Pacific Islander Veterans were as likely to begin psychotherapy as White Veterans but were less likely to receive an adequate treatment dose. Veterans with depression, bipolar disorder, psychotic disorders, or substance use disorder were also less likely to initiate psychotherapy, while those reporting military sexual trauma were more likely. Understanding these treatment disparities could improve participation in evidence-based psychotherapy. (Administration and Policy in Mental Health, June 20, 2023)
|
Agent Orange exposure increases risk of bladder cancer
 Image: ©Getty Images/magicmine (07/06/2023)
A study by Durham VA researchers and colleagues found a slightly increased risk of bladder cancer among male Vietnam Veterans exposed to Agent Orange. The study assessed the ties between exposure to Agent Orange, a chemical defoliant used by U.S. forces during the Vietnam War, and bladder cancer among 2,517,926 male Vietnam Veterans treated in VA hospitals from 2001 to 2019. The study showed a modestly increased risk of bladder cancer, but no change in the aggressiveness of the disease. In 2021, bladder cancer was added to VA’s list of presumptive conditions related to Agent Orange exposure, and the research team said these findings support that designation. (JAMA Network Open, June 27, 2023)
|
Unmet social needs linked to worse health care access
 Photo: ©Getty Images/FG Trade (07/06/2023)
A study by VA Boston researchers showed that unmet social needs adversely affect Veterans’ access to health care. Veterans with unmet social needs, such as food insecurity and loneliness, were more likely not to show for medical appointments and not adhere to their prescribed medications. This association existed for both rural and urban Veterans. Social disconnection and legal needs were the strongest predictors of care access problems. The researchers suggest that unmet social needs are associated with stress and negative attitudes toward prevention and self-care, and they recommend interventions on these unmet needs to improve care access. (Journal of General Internal Medicine, June 20, 2023)
|
Black Veterans face racial disparities in uterine fibroid treatment
 Photo: ©Getty Images/FatCamera (07/06/2023)
VA Puget Sound researchers and colleagues identified racial disparities in uterine fibroid treatment in VA patients. Uterine fibroids are common, nonmalignant tumors in the uterus that disproportionately impact Black women. In a group of more than 8,000 Veterans with symptomatic uterine fibroids who used VA health care, Black Veterans were less likely than White Veterans to receive any uterine fibroid treatment. This disparity was most pronounced among those with more severe cases of the disease. Black Veterans were also less likely to have a hysterectomy and more likely to have fertility-sparing treatments as their first treatment. The researchers suggest that dismissal or misattribution of symptoms by health care providers and medical mistrust by Black patients may explain this disparity, which needs to be addressed systematically. (Women’s Health Issues, July-August 2023)
|
Telehealth improves access to neurology care
 Photo: ©Getty Images/Hispanolistic (06/28/2023)
Researchers from the Richard L. Roudebush VA Medical Center in Indianapolis and their colleagues showed that remote telehealth resulted in more timely neurological care for Veterans. VA implemented the National Teleneurology Program (NTNP) at 12 VA sites in 2020. The NTNP consults were completed significantly faster than neurology consults in the community, taking place an average of 44 days after the appointment was requested, compared with 97 days for community care. Veterans also reported they were highly satisfied with NTNP care. The findings suggest that telehealth can help overcome barriers to care, especially in rural settings where neurological specialists are rare. (Journal of General Internal Medicine, June 20, 2023)
|
Medical scribes could decrease VA wait times
 Photo: ©Getty Images/SDI Productions (06/28/2023)
A VA Boston study found that medical scribes have the potential to lower patient wait times in VA. Medical scribes, who assist providers in navigating electronic health records and entering patient information, worked in cardiology and orthopedics specialty clinics at 18 VA medical centers. The scribe program led to an 8.5-day decrease in orthopedic appointment wait times, but no changes in cardiology wait times. Employment of medical scribes was also linked to increased provider productivity for both disciplines. The scribe program did not affect patient satisfaction either positively or negatively. The results suggest that scribes may be a useful tool to improve access to VA care. (Journal of General Internal Medicine, June 20, 2023)
|
VA Central Texas doctor invents hospital disinfection tracking system
 Photo courtesy of Xenex Disinfection Services. (06/28/2023)
Dr. Chetan Jinadatha of the VA Central Texas Healthcare System invented a device to track the disinfection of portable medical equipment, which will help reduce the spread of infections in hospitals. TrackMate, licensed for production by Xenex Disinfection Services, is a small device that connects to equipment such as IV pumps and vital monitoring machines. It senses moisture from liquid cleaning chemicals or UV light irradiation to keep a log of cleaning, allowing health care workers to quickly see the disinfection history of a piece of equipment before moving it to a new patient’s room. Studies have shown that using TrackMate doubled the amount of equipment cleanings. The device stores data both locally and online, allowing for easier record keeping and compliance monitoring. TrackMate is the world’s first automated disinfection tracking system. (Business Wire, June 26, 2023)
|
Vascular condition linked to memory problems in Alzheimer’s disease
 Photo: ©Getty Images/wenht (06/22/2023)
VA San Diego researchers and colleagues found that the blood flow problems from cerebrovascular disease can contribute to cognitive decline in people with Alzheimer’s disease. The researchers used positron emission tomography (PET) scans to measure the volume of white matter hyperintensities, which are brain lesions caused by cerebrovascular disease. They found that these white matter hyperintensities interacted with a build-up of amyloid-beta, a biomarker of Alzheimer’s disease, to negatively affect memory. This interaction was independent of levels of tau protein, another Alzheimer’s biomarker that is most directly associated with cognitive decline. The results highlight the importance of incorporating vascular health when assessing Alzheimer’s disease. (Journal of Alzheimer’s Disease, June 7, 2023)
|
Peer-support program helps minority Veterans engage with mental health care
 Photo: ©Getty Images/SDI Productions (06/22/2023)
VA researchers from Indianapolis, Boston, and Minneapolis interviewed racial and ethnic minority Veterans about PARTNER-MH, a program in which fellow Veterans help VA patients from minority groups navigate VA’s health care system and teach them how to advocate for themselves. Participants said the program increased their engagement and improved the patient-clinician relationship. The study also identified barriers in the program, including limited flexibility in peers’ schedules and lack of available peers of the same gender. The researchers concluded that peer support could be a good way to help Veterans communicate their needs in mental health care, especially for groups who often face health care disparities. (Patient Education and Counseling, June 13, 2023)
|
VA hospitals had lower COVID-19 mortality rates than community hospitals
 Photo: ©Getty Images/gorodenkoff (06/22/2023)
Iowa City VA Health Care System researchers learned that Veterans hospitalized for COVID-19 in VA hospitals were less likely to die than those treated in community hospitals. The study included data on nearly 65,000 Veterans 65 years old or older who were hospitalized with COVID-19 between March 2020 and December 2021. Veterans in community hospitals had a 27% risk of death within 30 days of hospitalization, compared with an 18% risk for those admitted to VA hospitals. However, about 74% of Veterans were admitted to community hospitals rather than VA hospitals. The results show that quality of VA health care compares favorably to non-VA care, but more efforts may be needed to ensure Veterans receiving care in the community get the best quality care. (JAMA Network Open, May 1, 2023)
|
Military sexual trauma often not captured in electronic health record, especially for minorities
 Photo: ©Getty Images/Portra (06/14/2023)
Researchers from the San Francisco, Minneapolis, and Greater Los Angeles VA health care systems learned that instances of military sexual trauma were often not properly identified in electronic health records. Among more than 1,000 women Veterans surveyed, 61% reported experiencing military sexual trauma but only 35% had this noted in their electronic health record. Furthermore, Black and Latina Veterans were more likely than White Veterans to have trauma missing from their electronic health record. Women who reported sexual harassment in the survey, as opposed to sexual assault, were five times more likely to have military sexual trauma not captured in the record, but multiple screenings for military sexual trauma increased the odds of it being captured in the record. The researchers concluded that efforts to address military screening disparities are needed, especially for minority Veterans. (Journal of General Internal Medicine, June 8, 2023)
|
Supervised electrical stimulation may reduce posttraumatic headaches
 Photo: ©Frontiers Media SA (06/14/2023)
VA researchers in Columbia, S.C., showed that at-home electrical stimulation can reduce persistent posttraumatic headaches. Twenty-five Veterans with persistent headaches linked to traumatic brain injury received 20 sessions of either transcranial direct current stimulation or a sham procedure to serve as a control group. After in-person training, Veterans in the stimulation group used a device to apply low-intensity direct electrical current through electrodes placed on the head while being remotely supervised by a member of the study team. Adherence rates were high, with 88% of participants completing the full treatment. The stimulation group experienced significantly fewer moderate-to-severe headaches, and the total number of headache days was also reduced. The results show that remote direct-current stimulation may provide a safe, non-invasive, and accessible way to treat posttraumatic headaches. (Frontiers in Neurology, May 5, 2023)
|
PTSD-related distress may surface at Veterans’ end of life
 Photo: ©Getty Images/LPETTET (06/14/2023)
VA Boston researchers identified several factors associated with PTSD distress at the end of life, such as pain, negative mood, and poor sleep. The study included retrospective data on more than 42,000 Veterans who died between 2009 and 2018. Almost one in ten experienced PTSD-related distress at the end of their life. Combat exposure, age, gender, and race all played a factor, with young, male minorities having the greatest association with PTSD-related distress. Veterans with more medical conditions – such as dementia, mental illness, and greater pain conditions – were also more likely to experience end-of-life PTSD distress. However, palliative care and emotional support were often linked to decreased odds of distress. The findings suggest that PTSD screening and increased specialized medical care are critical for decreasing PTSD-related distress at the end of life. (Journal of Pain and Symptom Management, April 19, 2023)
|
Veterans deployed to Southwest Asia exhibit more breathing difficulty
 Photo: ©Getty Images/SeventyFour (06/07/2023)
A study by VA New Jersey researchers showed that Veterans who deployed to Southwest Asia had greater breathing problems during exercise. The researchers measured breathing and heart rate for both deployed and non-deployed Veterans while they ran on a treadmill. Those who had deployed exhibited shortness of breath and a greater difficulty breathing. This lower respiratory frequency existed only in the deployed Veterans. The results support a link between deployment to Southwest Asia and respiratory problems, most likely due to exposure to particulate matter and toxic substances. (PLoS One, May 24, 2023)
|
Repeated tobacco screens increase likelihood of attempt to quit smoking
 Photo: ©Getty Images/Doucefleur (06/07/2023)
VA Greater Los Angeles researchers learned that repeatedly asking Veterans about their smoking habits increases the likelihood they would accept treatment to help them quit. Of about 6,000 Women Veterans who were screened for tobacco use during at least one VA health care visit in a five-year period, 49% said they were current or former smokers. Of those, about 14% accepted a prescription or referral to behavioral counseling for smoking cessation. Comparatively, 42% of those Veterans who were screened on five or six occasions in the same time period accepted treatment. The results suggest that persistence with screening Women Veterans for smoking can help inspire them to try cessation treatments. (Journal of General Internal Medicine, June 5, 2023)
|
Food insecurity increases risk of suicidal thoughts
 Photo: ©Getty Images/coldsnowstorm (06/07/2023)
A team including researchers from Durham VA, Providence VA, and the National Center on Homelessness among Veterans found that Veterans with food insecurity are at an elevated risk of suicidal ideation. The study included survey data from more than a thousand Veterans who represented all 50 states and all military branches. Veterans with food insecurity had nearly four times higher rates of suicidal ideation. Those with both food insecurity and mental health disorders had more than a nine-fold increase in the probability of suicidal ideation. The researchers concluded that regularly assessing for food insecurity and intervening accordingly could help reduce Veteran suicide. (Archives of Suicide Research, May 10, 2023)
|
VA tests new screening tool for early cancer detection
 Photo: ©Getty Images/FluxFactory (06/01/2023)
VA is partnering with Grail, LLC, to test a new cancer screening tool with the potential to detect cancer at an early stage through blood testing. The Wilkes-Barre VA Medical Center is the first of 10 VA sites to participate in the study, which will eventually make the Galleri multi-cancer early detection blood test available to 10,000 Veterans to test its effectiveness. In an earlier clinical trial, the Galleri test was able to detect more than 50 types of cancer, more than 45 of which currently lack recommended screening tests. If successful, the new blood test could make it possible to detect many different forms of cancer at early stages, when treatment is most likely to succeed. (May 25, 2023)
|
Researchers use rock-paper-scissors to test new brain-computer interface
 Photo: ©Getty Images/Baranova Valentina (06/01/2023)
VA San Diego researchers developed a noninvasive brain-computer interface capable of decoding hand gestures. The team used magnetoencephalography – measuring the brain’s magnetic fields to decode the electrical activity of neurons – to predict what gestures participants were thinking of during a rock-paper-scissors game. A machine learning algorithm was then able to decode the correct hand gestures from brain scans with high accuracy. The results show the potential of this noninvasive approach to allow users to control prosthetic devices with their minds. (Cerebral Cortex, May 13, 2023)
|
PTSD treatment could lower cardiovascular risk
 Photo: ©Getty Images/eyecare productions (06/01/2023)
Durham VA and Duke University researchers learned that psychotherapy treatments for PTSD may also lower the risk of coronary heart disease. Researchers compared cardiovascular biomarkers between participants with PTSD receiving cognitive processing therapy and those on a waiting list. Those receiving psychotherapy showed significant improvements in several measures of heart rate variability, which is a sign of cardiovascular risk. The researchers concluded that effective treatment of PTSD not only reduces psychological distress but could also lower risk of heart disease. (Journal of Psychosomatic Research, May 2, 2023)
|
Providers can use PACT Act to help Vets with feelings of institutional betrayal
 Photo: © Getty Images/Johnrob (05/25/2023)
A New Jersey VA research team interviewed a small group of Veterans to assess feelings of institutional betrayal, specifically, the perception that the U.S. government has failed to adequately prevent, acknowledge, and treat conditions caused by military environmental exposures, and in doing so has betrayed its promise of caring for Veterans. The interviews also explored the notion of institutional courage, a term developed to describe organizations that proactively protect and care for their members. Veterans’ depictions of courageous institutions contained key themes of being accountable, proactive, and mindful of unique experiences, supporting advocacy, addressing stigma related to public benefits, and offering safety. The study found the Sergeant First Class Heath Robinson Honoring our Promise to Address Comprehensive Toxics Act of 2022 (PACT Act) provides an opportunity to improve care for Veterans with environmental exposure concerns, mitigate institutional betrayal, and promote institutional courage. (MDPI, May 17, 2023)
|
New AI tool better identifies Vets with evictions who need additional help
 Photo: © Getty Images/Ole_CNX (05/25/2023)
VA researchers in Massachusetts recently developed a new natural language processing (NLP) model, which is a branch of artificial intelligence, to identify eviction status in electronic health records. The new system, known as the Knowledge Injection based on Ripple Effects of Social and Behavioral Determinants of Health (KIRESH), has already been shown to substantially outperform other state-of-the-art NLP models. When combined with a novel prompt the team designed, KIRESH was able to automatically detect Veterans’ eviction status from VA electronic health records. Researchers aim to use KIRESH as an eviction surveillance system to help address commonly related effects for Veterans, such as housing insecurity, unemployment, long-term poverty, and mental health problems. (Journal of the American Medical Informatics Association, May 18, 2023)
|
New treatment may reduce abdominal aortic aneurysms, preventing rupture
 Photo: © Getty Images/Ozgu Arslan (05/25/2023)
A VA-funded study found that mesenchymal stromal cells (MSCs), a type of stem cell, may be effective in slowing the growth of abdominal aortic aneurysms by reducing inflammation. Investigators at the Indianapolis VA Medical Center administered intravenous MSCs from a healthy donor to a patient with a small abdominal aortic aneurysm. The analysis found the procedure was safe, causing no allergic reactions. Seven days after treatment, there was a significant increase in the concentration of anti-inflammatory IL-10 among participants in both the high- and low-dose MSC groups compared with the placebo group. At day 14, there was a significant decrease in the percentage of inflammatory Th17 cells in both the high- and low-dose MSC groups. The researchers say further study is recommended. (American Heart Association, May 10, 2023)
|
VA, Denmark test AI model to predict pancreatic cancer
 Photo: © Getty Images/magicmine (05/17/2023)
A Boston VA study applied artificial intelligence (AI) methods to clinical data from 6 million patients in the Danish National Patient Registry and 3 million patients in the VA’s Corporate Data Warehouse to create a machine learning model that can predict pancreatic cancer as much as five years in advance. Approximately 80% of patients with pancreatic cancer are diagnosed in the late stage, when long-term survival is extremely uncommon: just 2% to 9% at five years. This makes early detection critical, but current methods such as biomarkers and family history only catch a fraction of cases. The AI was based on predictive machine learning models for other types of cancer, and researchers designed it to report risk scores for pancreatic cancer occurrence at intervals of three, six, 12, 36, and 60 months of the date of risk assessment. These results improve the ability to design realistic surveillance programs for patients at elevated risk and could provide life-saving early detection of an aggressive cancer. (Nature Medicine, May 8, 2023)
|
VA program provides Veterans self-care skills for chronic pain
 Photo: ©Getty Images/rudi_suardi (05/17/2023)
The Empower Veterans Program (EVP) is a 10-week interdisciplinary group medical appointment that provides Veterans with a host of chronic pain self-care skills for a whole-health driven approach to pain management. The initiative is in alignment with the 2016 Comprehensive Addiction and Recovery Act and VA’s Stepped Care Model, and it is funded by the Offices of Rural Health and Pain Management, Opioid Safety, and Prescription Drug Monitoring Program. A sample of 639 Veterans enrolled in EVP between May 2015 and December 2017 indicated participants showed significant improvement in three primary pain outcomes – intensity, interference, and catastrophizing – and 12 of 17 secondary outcomes, including quality of life, acceptance, and mindfulness measures. The data proves positive psychological and physical outcomes are possible through nonpharmacological means. (BMC Health Services Research, May 3, 2023)
|
VA considers multiple factors for telehealth, foremost is patient preference
 Photo: © Getty Images/MTStockStudio (05/17/2023)
A study by Greater Los Angeles VA researchers revealed that primary care team members consider several factors when assessing both the suitability of telehealth for appointments and whether to use phone or video. The decisions were largely guided by patient-related factors, including patient preferences, specific health issues, and access to technology. Additional considerations centered on team members’ personal preferences and factors that supported the wellbeing of the team, such as the flexibility to work from home and protection from infection. Generally, participants viewed the option of both telephone and video telehealth modalities as useful tools in the care of patients, although a few respondents emphasized its inferiority to in-person care. The findings determined that telehealth should be considered a useful tool both for care of patients and employee well-being, but suitability should be determined by multiple factors like resources, preferences, and timing. (Journal of Primary Care & Community Health, May 12, 2023)
|
VA care is better than or equal to non-VA care
 Photo: ©Getty Images/monkeybusinessimages (05/03/2023)
A review by VA Greater Los Angeles researchers found that VA care is consistently as good or better than non-VA care. The researchers looked at 37 studies published between 2015 and 2023 comparing care in the VA health care system with VA-paid community care. Clinical quality and safety of VA care was rated better than non-VA care in most studies. All studies found patient experience in VA to be better than or equal to non-VA care. Results on care access, cost, and efficiency were mixed, although few studies addressed these areas. (Journal of General Internal Medicine, April 19, 2023)
|
VA study identifies potential new treatment for fatty liver disease
 Image: ©Getty Images/wildpixel (05/03/2023)
VA Nebraska-Western Iowa Health Care System researchers discovered a potential new treatment for alcoholic fatty liver disease. Their work with ethanol-fed rats showed that alcohol consumption leads to the formation of lipid droplets, which is a type of fat accumulation in the liver. Rats given supplements of betaine, a compound naturally created in the liver, developed fewer and smaller lipid droplets. The researchers concluded that treatment with betaine has the potential to slow or prevent the development of alcoholic fatty liver disease. (Biology, March 16, 2023)
|
Personality disorders frequent in justice-involved Veterans
 Photo: ©Getty Images/simpson33 (05/03/2023)
A VA Rocky Mountain Mental Illness Research, Education and Clinical Center for Suicide Prevention study found that justice-involved Veterans were much more likely than other Veterans to have a personality disorder diagnosis. Researchers examined data on more than 1.6 million Veterans, about 12% of whom had been involved with the criminal justice system. Veterans who accessed VA justice-related services were about three times more likely to have a personality disorder. This connection was true for both male and female Veterans. The researchers suggested that VA’s justice-related services be augmented with psychotherapy to address possible personality disorders in these Veterans. (Journal of Nervous and Mental Disease, May 1, 2023)
|
Sleep apnea may explain link between anger and PTSD, chronic pain
 Photo: ©Getty Images/Evgeniy Anikeev (04/28/2023)
VA researchers showed that sleep problems may be to blame for anger issues linked to mental health conditions in Veterans. In a group of more than 1,500 Veterans and service members, PTSD symptoms; pain interference, the extent to which pain interferes with life; and hazardous alcohol use were associated with uncontrolled or chronic anger. Analysis revealed that obstructive sleep apnea largely accounted for the link between anger and both PTSD and pain. The researchers concluded that treating obstructive sleep apnea could be a new way to reduce anger problems caused by PTSD and chronic pain. (Journal of Psychiatric Research, March 2023)
|
Frailty increases risk of death after bypass surgery
 Photo: ©Getty Images/HRAUN (04/28/2023)
A study of more than 13,000 Veterans found that frail Veterans were significantly more likely to die after bypass surgery for coronary artery disease. Frail Veterans had a 75% higher risk of dying from any cause within five years of coronary artery bypass grafting surgery compared to Veterans without frailty, while Veterans assessed as pre-frail had a 20% higher risk. Frail and pre-frail Veterans were more likely to die or return to the hospital in the first year after surgery. The results suggest a need to address frailty before coronary surgery. The study group included researchers from the Cleveland, Boston, and Pittsburgh VA health care systems. (Journal of the American Geriatric Society, April 21, 2023)
|
Researchers develop potential new liver cancer treatment
 Image: ©Getty Images/CIPhotos (04/28/2023)
VA San Diego and University of California San Diego researchers created a potential new way to treat liver cancer. The researchers developed nanoparticles derived from the cowpea (black-eyed pea) mosaic virus, a virus that normally only infects legumes. Using a mouse model of liver cancer, they tested the nanoparticles on tumors along with cryoablation, a process that uses extreme cold to destroy tumor cells. The combined treatment delayed and inhibited cancer growth and also caused some shrinking in tumors not directly targeted by the treatment. This treatment triggered an increase in immune cells and reduced expression of compounds that promote tumor growth. The therapy could lead to an effective treatment for hepatocellular carcinoma, the most common form of liver cancer. (Journal of Vascular and Interventional Radiology, March 28, 2023)
|
Sepsis treatments accelerated while decreasing use of antibiotics
 Photo: ©Getty Images/dblight (04/19/2023)
A VA Ann Arbor Healthcare System study proved it was possible to hasten sepsis treatment while simultaneously decreasing overall antibiotic use. The study reported on temporal trends in antibiotic prescribing among more than 1.5 million hospitalizations in nationwide VA and Kaiser Permanente Northern California health care systems. Between 2013 and 2018, the average time to administer antimicrobial treatments among sepsis hospitalizations decreased by 37 minutes, while overall antibiotic use also decreased in the majority of instances. Clinical outcomes, such as mortality from sepsis, also improved over time. Researchers believe this study shows the feasibility of accelerating sepsis care while reducing overall antibiotic use. (JAMA Internal Medicine, June 27, 2022)
|
Cardiovascular risk factors linked to Alzheimer’s disease
 Photo: ©Getty Images/FG Trade (04/19/2023)
A team including researchers from the San Diego and San Francisco VAs found that cardiovascular risk factors could play a critical role in the development of Alzheimer’s disease. The study assessed adults 50 and older without dementia for cognition, biomarkers of Alzheimer’s disease in the blood, and cardiovascular risk factors such as high blood pressure, diabetes, and obesity. Those with high cardiovascular risk factors were more likely to have increased Alzheimer’s biomarker levels and lower cognitive processing. The results suggest that poor cardiovascular health is linked to cognitive degeneration. (Alzheimer’s & Dementia, March 8, 2023)
|
Serious adverse events from dentist-prescribed opioids rare in Veterans
 Photo: ©Getty Images/SbytovaMN (04/19/2023)
VA researchers from Hines, Ill., and Pittsburgh showed that poisoning or death from opioids prescribed by VA dentists were rare. Dentists are one of the leading prescribers of opioids, and dentist-prescribed opioids have been linked to serious adverse events. Out of nearly 140,000 Veterans prescribed an opioid by a dentist between 2015 and 2018, only 0.1% suffered opioid poisoning, and 1.1% died from any cause within six months of a dental visit. The rates of adverse events from VA dental prescriptions were lower than those reported in other studies on dental prescribing. (Journal of Public Health Dentistry, Feb. 17, 2023)
|
Suicidal ideations among Veterans fell during pandemic
 Photo: ©Getty Images/AnnaStills (04/13/2023)
Despite concerns that Veterans would be at a high risk of suicide because of the COVID-19 pandemic, a recent study by VA Connecticut researchers found that rates of suicidal thoughts in Veterans actually decreased after the onset of the pandemic. The study included more than 2,000 Veterans assessed for suicidal thoughts. In this group, 9.3% reported suicidal thoughts pre-pandemic in 2019, which dropped to 6.8% in 2020 before increasing slightly to 7.7% in 2022. Only 0.4% of participants attempted suicide during the pandemic, a rate consistent with pre-pandemic numbers. The factors most associated with new suicidal thoughts were higher education, lifetime substance use disorder, pre-pandemic loneliness, and lower pre-pandemic purpose in life. (JAMA Psychiatry, April 5, 2023)
|
Risk of death from COVID-19 decreased, still higher than flu risk
 Photo: ©Getty Images/Halfpoint (04/13/2023)
St. Louis VA researchers learned that the risk of death from COVID-19 is still higher than the risk of death from the flu despite a decreasing COVID-19 mortality risk. The researchers analyzed VA hospital admissions between October 2022 and January 2023. Death rates for patients admitted for COVID-19 were 6%, while death rates for flu patients were 4%. In 2020, 17% to 21% of patients hospitalized with COVID-19 died, compared with 4% of patients hospitalized for the flu. The researchers attribute the decreased COVID-19 death rate to vaccinations and improved clinical care, as well changes in virus variants. (JAMA, April 6, 2023)
|
Anti-HIV drug could lower diabetes risk
 Photo: ©Getty Images/YakubovAlim (04/13/2023)
Researchers from the VAMC in Columbia, S.C., alongside colleagues from the University of Virginia, have identified an HIV medication with the potential to help prevent diabetes. The research team analyzed data on more than 32,000 Veterans with HIV who were treated in VA facilities from 2000 to 2021. Those exposed to nucleoside reverse treascriptase inhibitors (NRTIs) had a reduced risk of developing prediabetes and type 2 diabetes. Previous research with cells and animal models showed that NRTIs can improve insulin sensitivity and uptake. The results suggest that NRTIs could help lower the risk of diabetes in both people with HIV and the general population. (MedComm–Future Medicine, April 3, 2023)
|
Rheumatoid arthritis linked to increased health burden
 Photo: ©Getty Images/digitalskillet (04/06/2023)
A VA San Diego study found that Veterans with rheumatoid arthritis were more likely to be older, in a minority ethnic group, unpartnered, or have a lower income. They were also more likely to be combat Veterans with a greater trauma burden, as well as having medical conditions such as osteoarthritis, chronic pain, cardiovascular conditions, insomnia, PTSD, or alcohol use disorder. On average, 1 in 20 Veterans will have rheumatoid arthritis. The results suggest an elevated health burden may be associated with rheumatoid arthritis. (Journal of Psychiatric Research, March 2021)
|
Veterans receive equal heart care whether rural or urban
 Photo: ©Getty Images/andresr (04/06/2023)
VA researchers in White River Junction, Vermont, proved rural and urban Veterans receive equal levels of care for congestive heart failure in VA clinics. The VA study analyzed electronic health records from nearly 300,000 VA patients who had congestive heart failure between 2012 and 2017. Unlike disparities often seen in non-VA care, researchers found there was no meaningful differences in care received between rural and urban Veterans. The study also found that rural Veterans were slightly less likely to use specialty care in VA, but more likely to use VA primary care and telemedicine. The findings suggest that VA may have successfully addressed access and health disparities typically seen in rural patients with congestive heart failure. The study also suggested the Veterans Choice Program may have enabled more patients to receive heart care at non-VA facilities. (Journal of Rural Health, April 2, 2023)
|
Veterans support suicide screenings as part of primary care
 Photo: ©Getty Images/pcess609 (04/06/2023)
VA Portland researchers and colleagues surveyed 868 Veterans about VA’s suicide risk screening initiative, Risk ID, and more than 90% of Veterans said it was appropriate for doctors, nurses, or medical assistants to ask Veterans about thoughts of suicide during primary care visits. About half thought Veterans should be asked about suicidal thoughts at every visit. While Veterans were supportive of the screening process, they did indicate that additional staff training would be useful to ensure patients felt heard and to increase patient understanding of the purpose of the screenings. The survey suggests a patient-centered approach can encourage disclosure of suicidal thoughts in Veterans. (Journal of General Internal Medicine, March 20, 2023)
|
Paxlovid lowers risk of COVID post-conditions, hospitalization, death
 Photo: ©Getty Images/Rafmaster (03/30/2023)
A study by VA St. Louis researchers found that the antiviral drug Paxlovid lowers the risk of long COVID and death. The researchers looked at outcomes of more than 280,000 high-risk VA COVID-19 patients, nearly 36,000 of whom had been prescribed Paxlovid (generic name nirmatrelvir). Patients who were given the medication within five days of a positive COVID-19 test had a 26% lower risk of developing post-COVID conditions, a 47% lower risk of death from the disease, and a 24% lower risk of needing hospitalization. Paxlovid reduced the risk of long COVID symptoms in people who were unvaccinated, vaccinated, and boosted, and in people with their first infection or a reinfection. Study author Dr. Ziyad Al-Aly said the findings support using Paxlovid for high-risk patients both to treat acute COVID-19 and to lower the risk of lasting effects. (JAMA Network Open, March 23, 2023)
|
Electronic analysis identifies social determinants of health as suicide risks
 Photo: ©Getty Images/Marco VDM (03/30/2023)
A team led by VA National Center of Homelessness Among Veterans researchers used a computer program to show that social factors affecting health are risk factors for suicide among Veterans. The researchers developed a program using natural language processing to identify social determinants of health — factors such as socioeconomic status, education, and housing — from both structured and unstructured electronic health record notes. By analyzing records of more than 6 million Veterans, the team found that social factors that negatively affect health also increased suicide risk. The social determinants of health with the largest effect on suicide risk were legal problems, violence, and nonspecific psychosocial needs. The results suggest that natural language processing could help identify risk factors for suicide that may otherwise be missed. (JAMA Network Open, March 1, 2023)
|
Heart problems linked to kidney problems
 Image: ©Getty Images/HYWARDS (03/30/2023)
Early signs of heart failure may be linked to the development of kidney disease. A team including VA researchers from Chicago, San Francisco, and San Diego compared heart and kidney function in more than 2,000 participants of a cardiovascular health study. Those who showed signs of strain on the heart muscles and heart dysfunction that did not yet rise to the clinical definition of heart failure also had higher levels of markers for kidney dysfunction. The results suggest that heart problems may lead to a decline in kidney function even in people without clinical heart failure. (Kidney360, March 8, 2023)
|
VA group intervention decreases intimate partner violence
 Photo: ©Getty Images/Vladimir Vladimirov (03/23/2023)
A new VA group intervention program called Strength at Home proved cognitive behavioral therapy and motivational approaches can lead to reductions in intimate partner violence. VA researchers from Central Texas, Boston, and Washington, DC, evaluated results of the program at 73 VA health care facilities. Strength at Home led to a 17% decrease in the use of physical aggression in relationships, a 23% decrease in psychological intimate partner violence, and an 18% decrease in coercive control behavior. Symptoms of PTSD and alcohol misuse also declined as a result of the program. The results show the importance of intimate partner violence intervention as part of routine health care. (JAMA Network Open, March 14, 2023)
|
Study identifies chemical that could protect kidneys from inflammation
 Photo: ©Getty Images/peakSTOCK (03/23/2023)
Researchers with the VA Calcium Signaling Laboratory in Washington, DC, identified a chemical that could help protect the kidneys from damage caused by inflammation. The team showed that the amino acid L-Arginine, which occurs naturally in the body, activates a receptor that controls how much calcium enters kidney cells. In this way, the chemical can lower the levels of chemicals that can cause scarring, inflammation, and death in kidney cells. The findings suggest that L-Arginine has the potential to help prevent kidney damage caused by conditions such as diabetes, high blood pressure, and COVID-19. (International Immunopharmacology, Feb. 22, 2023)
|
Veterans with past firearm injuries twice as likely to die by suicide
 Photo: ©Getty Images/cmannphoto (03/23/2023)
VA Portland researchers found that past nonfatal firearm injuries were linked to increased risk of Veterans dying by suicide. Out of nearly 10 million Veterans included in the study, more than 11,000 experienced nonfatal firearm injuries: 65% were unintentional injuries, 12% were intentional self-harm, and 19% were assault. Of the Veterans with previous injuries, 69 later died by suicide. Veterans with a previous firearm injury were more than twice as likely as those without a previous injury to die by suicide, even when the previous injury was accidental. The results suggest that nonfatal firearm injuries, regardless of intent, should be included in suicide risk assessments. (Academic Emergency Medicine, March 4, 2023)
|
VA health care protects Veterans from medical financial hardship
 Photo: ©Getty Images/sturti (03/16/2023)
A VA study showed that low-income Veterans who use VA health care were less likely to face financial hardships caused by medical issues than those who did not. Out of more than 2,000 low-income Veterans surveyed, about 35% had VA health coverage. Those Veterans were less likely to experience both objective and subjective medical financial hardships compared to Veterans with Medicare and no VA coverage. Hardships included spending a high percentage of income on health care, difficulty paying medical bills, worrying about health care expenses, and delaying or forgoing care. VA provides low- or no-cost care to Veterans with low income, yet many eligible Veterans are not enrolled. The study team, made up of researchers from Portland, Oregon; Greater Los Angeles; and San Francisco VA health care systems, called for efforts to address Veterans’ lack of health coverage. (American Journal of Preventive Medicine, March 9, 2023)
|
Self-perceived hearing loss may be linked to PTSD
 Photo: ©Getty Images/PaulCalbar (03/16/2023)
VA Pittsburgh researchers found that PTSD assessments could be useful for identifying potential hearing problems that don’t show up on normal hearing tests. The researchers looked at medical records from 286 Veterans who reported difficulties with their hearing despite normal audiometric results, and they found 16 different health conditions that may be linked to the self-reported hearing loss, with PTSD and related symptoms being the most prevalent conditions. The researchers concluded that Veterans with a higher number of diagnosed medical conditions, especially including PTSD, were more likely to have self-perceived hearing impairment as well. (Journal of the American Academy of Audiology, Jan. 19, 2023)
|
Veteran cannabis, stimulant use disorder diagnoses have increased in recent years
 Photo: ©Getty Images/gradyreese (03/16/2023)
A study by San Francisco and Greater Los Angeles VA researchers revealed that substance use disorder diagnoses among Veterans have increased over the last decade, especially for cannabis and amphetamine use. Looking at medical records data, the researchers found substance use disorders increased for most substances between 2010 and 2015. Alcohol, cannabis, and stimulant use disorders increased by between 4% to 18% annually for 2016 to 2019, while cocaine, opioid, and sedative use disorders changed less than one percent in that time frame. Alcohol use disorder was the most common diagnosis. Amphetamine and cannabis misuse increased the most rapidly in both time periods, and older Veterans had the largest increases in diagnoses across substances. The findings highlight a need to address cannabis and amphetamine misuse, which have fewer treatment options than alcohol or opioid use disorders. (American Journal of Addictions, March 8, 2023)
|
Veterans with dementia more likely to visit emergency departments
 Photo: ©Getty Images/pablohart (03/09/2023)
In a study of data from more than 3 million Veterans, VA researchers from Durham, North Carolina, and Palo Alto, California, learned that Veterans with dementia are significantly more likely to use emergency departments than those without. In the study group of Veterans 65 years and older, about 8% had a dementia diagnosis. These Veterans were nearly twice as likely to have an emergency department visit and were admitted to the hospital at higher rates. The most common reasons for emergency department visits were falls, weakness, and abnormal mental state, all of which were more common in Veterans with dementia. The results show that emergency departments are common health care access points for Veterans with dementia and suggest that targeted interventions may be needed to improve acute care for these Veterans. (Academic Emergency Medicine, Feb. 9, 2023)
|
Stressful life events increase Veterans’ risk of homelessness
 Photo: ©Getty Images/urbazon (03/09/2023)
A VA study showed that stressful life events after transitioning from military to civilian life are a key factor in the risk of homelessness. The researchers surveyed more than 16,500 military members while they were on active duty and again after they returned from service. Those who faced stressful life events such as serious illness, financial crisis, and interpersonal problems were significantly more likely to experience homelessness after their service. Personal betrayal by a loved one and economic problems played the largest roles in homelessness risk. The study team included VA researchers from Birmingham, Alabama, Washington, DC, and San Diego. They conclude that Veteran homelessness might be reduced by gearing interventions toward the effects of stressful life events experienced during the transition back to civilian life. (Public Health Reports, Feb. 1, 2023)
|
Interaction between other medications and genes could make opioids less effective
 Photo: ©Getty Images/DNY59 (03/09/2023)
An analysis of how different medications interact with genes showed that many Veterans are taking drug combinations that make opioid treatment less effective. Researchers looked at data on 2.4 million Veterans with at least one opioid prescription for pain. About 22% had an elevated risk of an undesirable response to opioid medication based on the other drugs they were taking and their genetic profiles. A gene called CYP2D6 influences how the body metabolizes opioids. Some antidepressants also interact with CYP2D6, which can alter how opioids act in the body. Based on these gene interactions, the researchers found that about 4% of Veterans studied had drug combinations that increased the risk of toxicity and 17% were taking combinations that could lead to poorer metabolization of opioids, which can make them less effective. The researchers conclude that using genetic testing to find these interactions could make precision medicine and pain management more effective. (Pain, Dec. 1, 2022)
|
Veterans with or without head trauma benefit from magnetic treatment for depression
 Photo by Jeff Bowen (03/02/2023)
VA researchers demonstrated that traumatic brain injury does not lower the effectiveness of transcranial magnetic stimulation (TMS) to treat depression. In a group of more than 600 Veterans who received TMS for depression, both those with and without a history of mild traumatic brain injury saw depression symptom improvement regardless of how many traumas they had. TMS applies a magnetic field to the outside of the head to alter brain electrical signals, but researchers weren’t previously sure whether a history of traumatic brain injury would make the TMS less effective at treating depression. The research team consisted of investigators from Providence, Rhode Island, and San Diego and Palo Alto in California. The results show that mild traumatic brain injury should not disqualify Veterans from TMS treatment. (Neuromodulation, Feb. 1, 2023)
|
Rural Veterans more likely to be overprescribed antibiotics
 Photo: ©Getty Images/Ridofranz (03/02/2023)
VA researchers from Providence, Rhode Island, found that inappropriate antibiotic prescribing is more common in rural areas. Excessive antibiotic use can lead to drug-resistant infections and side effects. The researchers looked at data for 1.4 million Veterans who received outpatient antibiotic prescriptions in VA over a 10-year period. Veterans living in rural areas were more likely than Veterans in urban areas to be prescribed fluoroquinolones, which are broad-spectrum antibiotics often overprescribed when more selective antibiotics are available. Rural Veterans were also more likely to receive longer antibiotic prescriptions. The researchers conclude that outpatient antibiotic prescribing must be improved, particularly for rural Veterans. (Antibiotics (Basel), Jan. 20, 2023)
|
Cancer drug has potential for repurposing as arthritis treatment
 Photo: ©Getty Images/scyther5 (03/02/2023)
A team including researchers from the Jesse Brown VA Medical Center in Chicago identified a drug with potential to reduce arthritis pain and prevent joint damage. Using a mouse model, the researchers tested the effects of pazopanib, a drug normally used to treat kidney cancer, on osteoarthritis pain. They found that injections of pazopanib immediately relieved pain and also prevented cartilage degeneration. The drug suppresses the expression of proteins involved in pain signaling and cell growth. The researchers are hopeful that pazopanib can be developed into an effective treatment for osteoarthritis in humans. (International Journal of Biological Sciences, Jan. 1, 2023)
|
Homeless Veterans receive better depression care in homeless-tailored clinics
 Photo: ©Getty Images/FatCamera (02/24/2023)
VA Greater Los Angeles researchers and colleagues looked at treatment data for nearly 3,000 homeless Veterans who screened positive for depression, 13% of whom were treated in homeless-tailored primary care clinics. About 63% of Veterans receiving homeless-tailored care had a follow-up appointment within 84 days of depression screening, compared with 46% of those receiving standard care. The study also found that slightly more Veterans in homeless-tailored care received the correct amount of mental health treatment: 89% versus 82% in standard care. The results highlight the benefit of tailoring mental health care to the specific needs of homeless Veterans. (Journal of General Internal Medicine, Feb. 21, 2023)
|
Insomnia only indirectly linked to suicidal thoughts
 Photo: ©Getty Images/nong2 (02/24/2023)
VA Rocky Mountain researchers showed that insomnia is linked to mental health disorders, but not directly to suicidal thoughts. In an analysis of more than 300 Veterans, those with insomnia were more likely to have depression, PTSD, and anxiety symptoms than Veterans without insomnia. The researchers did not find a direct link between insomnia and suicidal thoughts after the other mental health conditions were taken into consideration. The findings suggest that insomnia may contribute to suicide risk through worsening mental health symptoms, rather than directly increasing risk. (Journal of Clinical Psychology, Jan. 25, 2023)
|
Physical activity improves memory in older adults
 Photo: ©Getty Images/Lordn (02/24/2023)
VA San Diego researchers and colleagues demonstrated that engaging in physical activity can help improve memory and cognitive function in older people. Forty-three older adults wore accelerometers for a week to measure their activity levels before undergoing cognitive testing. More time spent in moderate to vigorous activity was linked to better memory and executive function. MRI scans showed that physical activity may also improve cerebrovascular health. The results add to the evidence that exercise not only improves physical health, but also mental health. (Journal of the International Neuropsychological Society, Feb. 15, 2023)
|
Memphis study proves providing support to parent caregivers helps Veterans
 Photo: ©Getty Images/puhimec (02/16/2023)
Memphis VA researchers provided either six one-hour, one-on-one, behavioral sessions or six 30-minute prerecorded, online, educational webinars to 163 parent caregivers of Veterans and then assessed them for mental health outcomes. Parents in both groups improved significantly in depression, anxiety, and burden. Their ability to report troubling behaviors in the Veterans under their care also improved. Parents in the one-on-one group reported greater satisfaction, understanding of post-9/11 injuries, and coping skills. Both groups said the interventions improved their self-reflection, feelings of loneliness, self-efficacy, and ability to help. The results show that organizations with varying resources can provide meaningful support to caregivers of Veterans. (NeuroRehabilitation, Jan. 20, 2023)
|
Medication for gout, kidney stones may help preserve diabetic patients’ vision
 Photo: ©Getty Images/FG Trade (02/16/2023)
Columbia VA researchers found that allopurinol, a medication used to treat gout and kidney stones, could reduce the risk of diabetic macular edema, a condition that can lead to blindness. Allopurinol stops the release of substances in the body that cause inflammation, which may prevent fluid build-up in the retinas. In a group of Veterans with type 2 diabetes, those taking allopurinol had a 25% lower risk of diabetic macular edema, which is one of the major causes of vision problems in people with diabetes. The researchers concluded that this drug has the potential to be repurposed for diabetic patients. (Ocular Immunology and Inflammation, Feb. 7, 2023)
|
Computer model could help predict response to depression treatment
 Photo: ©Getty Images/Visivasnc (02/16/2023)
VA researchers developed a machine learning model to predict how well Veterans would respond to combined antidepressants and psychotherapy treatment for depression. The computer model accurately predicted the 30% of Veterans who responded favorably to the combined treatment out of more than 600 Veterans in the study. The most important predictors of treatment response were psychological resilience, symptoms and co-occurring health conditions, recent stressors, and treatment characteristics. This type of machine learning approach could help doctors predict how patients with depression will respond to treatment and allow them to adjust accordingly. (Journal of Affective Disorders, Jan. 26. 2023)
|
Vitamin D supplementation linked to lower suicide risk
 Photo: ©Getty Images/Helin Loik-Tomson (02/08/2023)
A VA study found that vitamin D supplements might drastically reduce suicidal ideations in Veterans. Canandaigua VA Medical Center researchers looked at data from 2010 to 2018 and found that Veterans with vitamin D prescriptions had a 45% lower risk of suicide attempts and a 48% lower risk of self-harm. The difference in risk level was even higher in Black Veterans and those with lower starting vitamin D levels. Vitamin D deficiency is more common in people with darker skin tones. Researchers also found that Veterans prescribed higher doses of vitamin D supplements had lower suicide risk than those given lower doses. The results suggest that vitamin D supplements hold promise as a treatment to help prevent suicide. (PLoS One, Feb. 1, 2023)
|
Female Veterans report frequent mental distress
 Photo: ©Getty Images/fizkes (02/08/2023)
A VA Pittsburgh study found female Veterans are more likely to experience mental distress than male Veterans or female non-Veterans. Researchers analyzed data on self-reported mental distress in a national sample of people over a 17-year period. In each year, female Veterans reported significantly more days of mental distress and a higher prevalence of frequent mental distress than male Veterans. In several of the years studied, female Veterans also reported greater levels of mental distress than non-Veteran women. The findings highlight the need for more specific efforts to address mental health among female Veterans. (Journal of Behavioral Health Services and Research, January 2023)
|
Racial disparities in chronic pain care
 Photo: ©Getty Images/Igor Vershinsky (02/08/2023)
Iowa City VA researchers identified potential racial disparities in Veteran chronic pain treatment. The study included more than 2 million Veterans who received treatment in VA for chronic pain in 2018. The researchers found no differences based on race in pain-related primary care visits. However, Black Veterans were less likely than White Veterans to receive pain clinic visits. Black Veterans who lived in rural areas were even less likely to visit a pain clinic. Black and Hispanic Veterans were more likely than White Veterans to go to the emergency department or urgent care for chronic pain. On the other hand, Black, Hispanic, and Asian Veterans were more likely to receive pain-related physical therapy visits than White Veterans. Although rates of primary care visits were similar, the researcher concluded that lower pain clinic visits and increased use of urgent care could indicate inadequate chronic pain management among Black Veterans. (Journal of Rural Health, Jan. 25, 2023)
|
Study tests how long anti-clotting drugs should be taken after heart surgery
 Photo: ©Getty Images/AsiaVision (02/01/2023)
VA Boston researchers determined that nine months may be the ideal amount of time for patients to take anti-clotting medication after heart surgery. Doctors prescribe antiplatelet medicines to prevent clotting after implanting a stent to clear blocked arteries. While these medications are needed to lower the risk of heart attack and other heart concerns, they also raise the risk of major bleeding problems. Researchers compared outcomes of more than 40,000 patients who had stent surgery and were prescribed dual antiplatelet therapy for different lengths of time. The risk of death was higher when patients stopped taking the medications less than nine months after surgery, compared with longer medication times. Discontinuing medication after nine months was linked to lower risk of death, heart attack, and major bleeding compared to continuing the medication for longer. Many current guidelines call for prescribing the medications for more than 12 months, but the results clearly support stopping dual antiplatelet therapy after nine months. (Journal of the American Heart Association, Jan. 17, 2023)
|
Effects of military service on brain injury symptoms vary
 Photo: ©Getty Images/DanielBendjy (02/01/2023)
A VA study found that combat deployment, era of service, and length of service all affect how Veterans are affected by traumatic brain injury (TBI). Researchers looked at data on nearly 8,000 people with TBI treated at private-sector hospitals. One year after the injury, those with a history of combat deployment were more likely to have lung disorders, PTSD, and sleep disorders than non-Veterans and Veterans who did not see combat. Veterans who served in the post-draft era were more likely than non-Veterans and Veterans from earlier eras to have chronic pain, liver disease, and arthritis. Veterans who served for more than four years had increased risk of high cholesterol, PTSD, and sleep disorder compared to those who were in the military for a shorter period. Veterans who did not see combat had better cognition and psychological health in the first five years after injury than non-Veterans. The results show that multiple individual factors need to be considered when assessing Veterans’ post-TBI health. (Journal of Neurotrauma, Dec. 28, 2022)
|
VA doctors develop elder abuse screening tool
 Photo for illustrative purposes only. ©Getty Images/SDI Productions (02/01/2023)
VA researchers and clinicians at the Louis Stokes Cleveland VA Medical Center emergency department developed a tool to screen older patients for elder abuse during visits. Emergency visits for injury or illness may be the only time isolated older Veterans leave their homes, but most VA emergency departments do not have standardized elder abuse assessment protocols. Out of 251 Veterans screened with the new tool, nine screened positive for possible elder abuse: a screen rate similar to those found by other measures of elder abuse. Based on the success of the pilot, six additional VA emergency departments began using the screening tool, and work is underway to add the tool to the VA electronic health record system. (Academic Emergency Medicine, Dec. 27, 2022)
|
Military sexual trauma increases suicidal thoughts and attempts
 Photo: ©Getty Images/SanyaSM (01/26/2023)
A VA Rocky Mountain Mental Illness Research, Education and Clinical Center (MIRECC) for Suicide Prevention study showed military sexual trauma is frequently associated with suicidal thoughts and attempts in female Veterans. More than 300 female Veterans receiving reproductive health care through VA participated in the survey, and about 69% screened positive for military sexual trauma. Women who had experienced either sexual harassment or sexual assault had increased risk of suicidal thoughts following military service. Furthermore, 31% of study participants reported military sexual trauma on the survey but had a negative screen in their electronic health record, highlighting the problem of military sexual trauma underreporting. The researchers recommend increasing efforts to remove barriers to military sexual trauma disclosure. (Journal of Interpersonal Violence, Jan. 25, 2023)
|
Back hunching linked to increased risk of death in older men
 Photo: ©Getty Images/FG Trade (01/26/2023)
A study by VA researchers and colleagues found that back hunching caused by age is linked to increased risk of death in older men. Many older people develop an exaggerated, forward rounding of the upper back, called hyperkyphosis, usually caused by weakening of the spinal bones. Researchers followed more than 6,000 men age 65 or older for an average of eight years after measuring back curvature. Those with greater back curvature had a higher chance of death than those with straighter posture. The association remained even when the researchers adjusted for other measures of physical function such as bone density and walking speed. The findings suggest that hyperkyphosis identified during a physical exam should be evaluated and treated to prevent worsening health. (Journal of the American Geriatrics Society, Oct. 28, 2022)
|
Trauma-associated sleep disorder common in Veterans
 Photo: ©Getty Images/PeopleImages (01/26/2023)
A study by VA Durham researchers found that trauma-associated sleep disorder is common in Veterans. Trauma-associated sleep disorder refers to nightmares and disturbed sleep linked to traumatic experiences. While nightmares are often associated with PTSD, trauma survivors commonly report nightmares even when they don’t have PTSD. In a group of nearly 4,000 Veterans, 12% had trauma-associated sleep disorder. Male and female Veterans had similar rates of sleep disorder. Veterans with the condition had almost four times the prevalence of PTSD and major depressive disorder, compared with those without the sleep disorder. The results highlight the need for improved screening for trauma-associated sleep disorder in Veterans, which is not currently part of routine clinical practice. (Sleep Advances, Jan. 12, 2023)
|
VA tablet program increased Veterans’ telehealth use during pandemic
 Photo: ©Getty Images/Charday Penn (01/19/2023)
The VA Office of Connected Care widely expanded its video-enabled tablet program at the onset of the pandemic, increasing the number of Veterans who received tablets nearly six-fold. When VA Palo Alto researchers and colleagues compared pandemic access numbers to those from 2019 and 2020, they found that Veterans who received tablets during the pandemic were more likely to use video care, and they did so more frequently than those who received tablets before the pandemic. However, older Veterans, or those unstably housed, were less likely to use video visits than other groups. The researchers concluded interventions may be needed to improve telehealth access for Veterans with unstable housing or who are less familiar with technology. (Journal of Medical Internet Research, Dec. 20, 2022)
|
Patients who have had surgery for lung cancer might not need extra surveillance
 Photo: ©Getty Images/shironosov (01/19/2023)
A VA St. Louis study found that high-frequency surveillance may not improve outcomes for patients who had surgery for lung cancer. Researchers followed Veterans who had surgery for non-small cell lung cancer for an average of seven years. About half had computed tomography (CT) scans every 6 to 12 months, while the other half had CT scans every 3 to 6 months. The analysis did not show any difference in cancer recurrence rates or overall survival between the two groups. The researchers suggest that future lung cancer treatment guidelines consider less frequent surveillance imaging to reduce patient anxiety and mitigate costs. (Journal of the National Cancer Institute, Nov. 29, 2022)
|
VA identifies predictors of Veteran homelessness
 Photo: ©Getty Images/Srdjanns74 (01/19/2023)
Researchers analyzed data from 2012 to 2021 on more than 570,000 Veterans in order to identify predictors for who is most likely to use VA’s Supportive Services for Veteran Families (SSVF) program and achieve stable housing. SSVF is the nation’s largest program for homelessness prevention and rapid rehousing services. Veterans with higher levels of education had longer and more frequent SSVF use and were less likely to exit the program for stable housing — researchers speculated this may be due to higher prevalence of vulnerabilities, such as lack of social support or more time searching for jobs that met Veterans’ qualifications. Veterans with greater disease burden were also less likely to achieve stable housing. However, those with mental health diagnoses or higher VA outpatient costs were more likely to find stable housing, suggesting greater engagement. Naturally, Veterans with a higher income were associated with a higher likelihood of exiting the program for stable housing, as well as shorter time in SSVF and fewer repeat usage episodes. Rural Veterans were also more likely to exit SSVF for stable housing and had fewer repeat uses than urban Veterans. These findings could help the VA to better direct resources to Veterans most in need of homelessness assistance. (Evaluation and Program Planning, Dec. 26, 2022)
|
Potential new treatment to prevent dementia
 Image: ©Getty Images/MediaProduction (01/10/2023)
James A. Haley Veterans Hospital researchers and colleagues developed a potential new approach to preventing dementia onset caused by aging. Previous research has shown defective insulin signaling in the brain plays a role in the early stages of dementia. Using a mouse model, the researchers showed that the RNA gene GAS5 regulates insulin signaling and affects neuron health. Nasal spray treatment with a molecular compound called NPC86, which binds to GAS5, increased GAS5 expression and improved neuron cellular function in mice. The results suggest that medications targeting the GAS5 gene have potential to slow or prevent the beginning of neurodegenerative diseases, such as Alzheimer’s disease. (Scientific Reports, Jan. 6, 2023)
|
Social workers in primary care teams lead to more palliative care use
 Photo: ©Getty Images/Dean Mitchell (01/10/2023)
Adding social workers to primary care teams increased palliative care use by Veterans in VA health care. Palliative care refers to health care aiming to improve quality of life and ease suffering in patients with serious, complex illnesses rather than focusing only on the condition. Researchers analyzed data on more than 43,000 Veterans receiving care at 71 VA primary care sites. Adding social workers to Patient Aligned Care Teams led to a two-fold increase in the number of Veterans who used palliative or hospice care after a hospital stay. Researchers concluded that including social workers in primary care teams can improve Veterans’ quality of care and use of high-value services. (JAMA Network Open, Jan. 3, 2023)
|
Higher suicide rates among lower-ranking soldiers
 Photo: ©Getty Images/SDI Productions (01/10/2023)
A study by the VA Rocky Mountain Mental Illness Research Education and Clinical Center found that lower-ranking enlisted soldiers had higher suicide rates than higher ranks. The study included more than 860,000 Army soldiers who returned from deployment in Afghanistan or Iraq from 2008 through 2014. The lowest-ranking soldiers had a suicide rate 1.58 times higher than higher-ranking enlisted soldiers and 2.41 times higher than officers. Suicide rates for lower-ranking soldiers remained higher for 11 years after deployment. This difference between ranks was consistent between both men and women. The results highlight the importance of targeting lower-ranking military members for post-deployment suicide prevention efforts. (Injury Epidemiology, Dec. 23, 2022)
|
Horse riding program could benefit Veterans with PTSD
 Photo: ©Getty Images/nd3000 (01/05/2023)
A VA Salt Lake City study showed Veterans with PTSD may benefit from a horse-riding program. Eighteen Veterans with PTSD demonstrated mood symptom improvement after participating in a pilot program of horsemanship lessons and trail rides. Participants also showed signs of enhanced psychological flexibility, defined as the ability to be present in the moment and fully aware of emotions and thoughts. No injuries occurred, showing the program can be run with minimal risk. The results provide preliminary evidence equine therapy may be useful for Veterans with PTSD even without a mental health treatment component. (Complementary Therapies in Medicine, Dec. 16, 2022)
|
Pharmacy specialist involvement improves diabetes care
 Photo: ©Getty Images/LaylaBird (01/05/2023)
A VA North Florida/South Georgia study found Veterans were prescribed diabetes medication with cardiovascular benefits more often when clinical pharmacy specialists were involved in their diabetes care decisions. Cardiovascular disease commonly occurs with diabetes cases. While some newer diabetes medications may protect against heart failure, there are several other diabetes medications that might worsen cardiovascular disease. Researchers analyzed data on more than 8,000 VA patients with diabetes. Of the 2,000-plus Veterans who had their treatment co-managed by a clinical pharmacy specialist, about 19% were prescribed heart-beneficial medications, compared to only 3% of those without specialist involvement. Researchers concluded clinical pharmacy specialists can help optimize treatment for patients with diabetes. (Journal of Pharmacy Practice, Dec. 5, 2022)
|
Online screening tool helps connect Veterans to mental health care
 Photo: ©Getty Images/Delmaine Donson (01/05/2023)
Iowa City VA researchers showed that an online screening tool can help connect service members returning from deployment with mental health care. More than 400 Reserve and National Guard service members tried the Web-Ed online program, which includes mental health screenings, personalized education, and links to VA health care. Sixty-nine percent of women and 72% of men screened positive for at least one mental health condition. Almost half said they planned to seek further assessment from a health care provider as a direct result of Web-Ed. Most users said they would recommend Web-Ed to other Veterans and that they received useful information. Personalized, online screening has the potential to engage Veterans who have not sought mental health care, according to the researchers. (Military Medicine, Dec. 13, 2022)
|
Mindfulness could help Veterans with suicidal thoughts
 Photo: ©Getty Images/Isbjorn (12/21/2022)
Mindfulness training has the potential to help Veterans admitted to a facility for suicidal thoughts, according to a VA Salt Lake City study. Mindfulness refers to being aware of the present moment through meditation and mental exercises. In this pilot study, 20 Veterans admitted to a psychiatric unit for suicidal thoughts received either mindfulness training or treatment as usual. The training was feasible in an in-patient setting, with no adverse effects. Participants in the mindfulness group were better able to view their experiences with curiosity while disengaging from experience without emotional overreaction. Both groups experienced significant reductions in suicidal thoughts. There was no difference between groups in in-patient or emergency department admissions after treatment. The results show that teaching mindfulness could help Veterans with suicidal thoughts, according to the researchers, but larger studies are needed to determine its effectiveness. (Military Medicine, Oct. 8, 2022)
|
Special operation forces experience greater TBI symptoms
 Photo: ©Getty Images/zabelin (12/21/2022)
Special operations forces personnel reported greater traumatic brain injury (TBI) symptom severity compared to conventional forces, in a study by James A. Haley Veterans’ Hospital researchers and colleagues. Special operations forces are at increased risk of TBI compared with conventional forces. In a group of service members and Veterans receiving in-patient rehabilitation for TBI, special operations personnel had greater PTSD symptoms, but less alcohol and drug use, than conventional forces. These personnel also reported greater neurobehavioral symptoms, such as dizziness, vision problems, and slowed thinking. Addressing TBI symptoms in special operations forces may be especially important, concluded the researchers. (Military Medicine, Oct. 29, 2022)
|
Peer health coaching could help address health care needs of homeless Veterans
 Photo: ©Getty Images/Khanchit Khirisutchalual (12/21/2022)
Peer coaching can help address the health care needs of homeless Veterans, according to a VA study. Twenty homeless Veterans who frequently used acute health care were offered weekly health coaching sessions with a peer over 12 weeks. On average, participants attended a little over six sessions. Satisfaction with the program was high, and Veterans’ perceptions of their health improved after the sessions. Feedback from participants suggested that increasing the length of the intervention could improve goal setting and coordination with primary care. This pilot study shows that peer health coaching could improve homeless Veterans’ health and reduce frequent use of acute care, according to the researchers. (BMC Primary Care, Dec. 19, 2022)
|
Sleep apnea linked to worse cognitive function in people with traumatic brain injury
 Photo: ©Getty Images/tommaso79 (12/13/2022)
Obstructive sleep apnea may lead to worse cognitive performance in people recovering from traumatic brain injury, found a study by James A. Haley Veteran’s Hospital researchers. Obstructive sleep apnea is common in people with TBI. Those with the condition may stop breathing or have decreased airflow during sleep because the muscles supporting the throat temporarily relax. Sixty participants with TBI had their sleep analyzed. Nearly 77% of participants had obstructive sleep apnea. Participants with apnea showed worse processing speed, memory, and executive functioning than those without apnea. Compared to those with moderate-to-severe apnea, participants with mild apnea had worse working memory and executive function. The results support including obstructive sleep apnea diagnosis in routine clinical care for TBI, according to the researchers. (Sleep Medicine, December 2022)
|
Danger during deployment linked to gun ownership in women Veterans
 Photo: ©Getty Images/Halfpoint (12/13/2022)
Perceived threat during deployment is linked to firearm ownership in women Veterans, according to a VA Rocky Mountain Mental Illness Research, Education and Clinical Center for Suicide Prevention study. Firearms are the leading means of suicide among women Veterans. The researchers surveyed nearly 500 women Veterans about their deployment experience and gun ownership. Veterans who felt more exposed to danger during deployment were more likely to own a firearm, regardless of their beliefs about safety in their civilian lives. Other deployment experiences, including sexual harassment and assault, general harassment, and combat experiences, were not directly associated with firearm ownership. Perceived threat of harm and negative thoughts about the world after military service were also not directly linked to firearm ownership. Efforts to address firearm access and safety in women Veterans may benefit from assessing heightened sense of danger during deployment, the researchers concluded. (Journal of Psychiatric Research, Nov. 14, 2022)
|
Anxiety sensitivity influences PTSD treatment effectiveness
 Photo: ©Getty Images/Vladimir Vladimirov (12/13/2022)
Anxiety sensitivity influences the effectiveness of PTSD treatment, according to a VA study. Anxiety sensitivity refers to fear of anxiety-related sensations and beliefs that anxiety is dangerous. Researchers looked at outcomes for Veterans with PTSD being treated with prolonged exposure (a psychotherapy), medication, or both. At 24 weeks into treatment, Veterans with high anxiety sensitivity also had high PTSD severity. Anxiety sensitivity did not lead to dropout of any treatment type. Anxiety sensitivity also significantly decreased in all treatment groups during the treatment period. The results suggest that anxiety can reduce the effect of PTSD treatment, but PTSD treatment can also improve anxiety, according to the researchers. (Journal of Traumatic Stress, Nov. 30, 2022)
|
Opioid reduction practices improved in VA
 Photo: ©Getty Images/smartstock (12/12/2022)
Handling of opioid de-prescribing within VA has improved in recent years, according to a VA study. In 2013, VA implemented the Opioid Safety Initiative to enhance safe and appropriate opioid use. To study the program's effects, researchers compared data on VA patients who had their opioid prescriptions lowered or stopped in 2013 and 2017. Clinical pharmacists and pain management specialists were more involved in 2017. More patients in 2017 had their doses tapered, and the tapering plans were executed over a longer time period. Transitions to non-opioid pain therapy were also higher in 2017. The findings show that the Opioid Safety Initiative has led to better opioid management in VA, according to the researchers. (Journal of General Internal Medicine, December 2022)
|
Engaging family and friends has potential to improve diabetes management
 Photo: ©Getty Images/Fertnig (12/12/2022)
A health coaching intervention focusing on family and friend support led to improved self-efficacy in people with diabetes, found a VA Pittsburgh and VA Ann Arbor study. Researchers recruited participants with diabetes along with a supporter, such as a spouse. Participants received a health coaching session followed by 12 months of telephone coaching calls. Compared to pairs receiving only general diabetes information, pairs in the coaching program saw improvements in willingness and ability to take independent action to manage their health. The coached participants also improved in healthy eating and satisfaction with health system support. However, both groups had similar improvements in measures of diabetes control. While engaging family and friend support can help people improve their diabetes care, more intensive direct coaching may be needed to improve diabetes outcomes, according to the study. (JAMA Network Open, Nov. 1, 2022)
|
Social stressors and health among transgender Veterans
 Photo: ©Getty Images/Renata Angerami (12/12/2022)
Older transgender and gender diverse Veterans have higher odds than older cisgender Veterans of having social stressors and health conditions, but lower odds of substance use, found a study by VA Bedford researchers and colleagues. Cisgender people are those whose personal identity corresponds to the sex they were assigned at birth. The researchers looked at data on nearly 5,000 Veterans. They found that older transgender and gender diverse Veterans were less likely than cisgender Veterans to have alcohol use disorder, drug use disorder, tobacco use, and anxiety. Transgender and gender diverse Veterans were more likely to experience depression, Alzheimer’s disease, cancer, violence, social and family problems, lack of access to health care, and military sexual trauma. These Veterans were also more likely to experience multiple social stressors. Interventions are needed to reduce health disparities for older transgender and gender diverse Veterans, according to the researchers. (LGBT Health, Nov. 29, 2022)
|
Veterans with Parkinson’s at higher risk of suicide
 Photo: ©Getty Images/Barbasa (12/01/2022)
Veterans with Parkinson’s disease are at increased risk of suicide, found a VA Rocky Mountain study. Researchers looked at data on nearly 1.5 million Veterans who used VA health care over a 19-year period. They found that Veterans with Parkinson’s disease had about a 50% greater risk of suicide, compared to those without. Veterans with Parkinson’s also had higher rates of mood, anxiety, and psychotic disorders. For both groups, 79% of suicides involved firearms. There was no significant difference in suicide methods between groups. Additional screenings and interventions are needed to prevent suicide in Veterans with Parkinson’s disease, say the researchers. (Parkinsonism and Related Disorders, Nov. 4, 2022)
|
Veteran video-based health care use differs by type, demographics
 Photo: ©Getty Images/Courtney Hale (12/01/2022)
VA Palo Alto researchers identified which Veteran populations are routinely using video-based health care. Out of more than 5 million Veterans, about 27% had at least one video health visit. Rates of video-based health care differed based on type of care: 15% of Veterans had at least one primary care video visit, 11% had a mental health video visit, and 6% had a specialty care video visit. Veterans with a history of housing instability had the highest rates of video care, driven by high usage of mental health care. American Indian/Alaska Native Veterans and low-income Veterans had lower odds of video visits compared with other groups. Outreach to these groups is needed to address disparities in health care access, according to the researchers. (Health Services Research, Nov. 7, 2022)
|
Longer drive time linked to lower receipt of recommended health care
 Photo: ©Getty Images/peeterv (12/01/2022)
Patients with longer drive times are less likely to receive recommended health care services, according to a Minneapolis VA study. Researchers looked at data for Veterans receiving VA care for osteoporosis, chronic obstructive pulmonary disease (COPD), or ischemic heart disease. The longer a Veteran had to drive to reach a health care facility, the less likely they were to receive recommended care. Compared to Veterans with a drive time of 30 minutes or less, those whose drive time was 61 to 90 minutes were 10% less likely to receive screening for osteoporosis or COPD. Those with a drive time of 91 to 120 minutes were 20% less likely to receive cardiac rehabilitation. New strategies are needed to limit patient travel burden, say the researchers. (JAMA Network Open, Nov. 1, 2022)
|
COVID-19 reinfection increases risk of death and health problems
 Photo: ©Getty Images/whyframestudios (11/22/2022)
COVID-19 reinfection increases the risk of death and health problems, according to a VA St. Louis study. Researchers used VA’s health care database to compare health outcomes of nearly 444,000 Veterans who had COVID-19 once, nearly 41,000 who had it two or more times, and over 5 million who never had it. They found that those who had multiple COVID-19 infections were at higher risk of death and hospitalization than those who only had COVID-19 once. They were also at higher risk for a variety of health problems, including lung and heart problems, diabetes, and mental health disorders. The risk was highest when people were first sick, but many still had elevated risk six months later. Risk of death and health problems increased with the number of infections. The results show that strategies are needed to prevent COVID-19 reinfection to protect against additional health risks, say the researchers. (Nature Medicine, Nov. 10, 2022)
|
Genetic risks of opioid use disorder identified
 Image: ©Getty Images/mesut zengin (11/22/2022)
Researchers with VA’s Million Veteran Program identified new genetic traits linked to opioid use disorder. The researchers analyzed the genomes on nearly 426,000 MVP participants. They identified 14 areas of the human genome where variations are linked to the risk of opioid use disorder. Twelve of these areas had not previously been linked to the disorder. The study also showed that opioid use disorder shares genetic traits with many other conditions, including psychiatric disorders and other substance use disorders. The findings add to the understanding of the biological basis of opioid use disorder and provide further evidence that it is a brain disease, according to the researchers. (Nature Neuroscience, October 2022)
|
Assessment tool can help weigh risks of lung cancer surgery
 Photo: ©Getty Images/utah778 (11/22/2022)
VA St. Louis researchers and colleagues developed a tool to accurately predict a patient’s risk of death after lung cancer surgery. Surgery is the preferred treatment for early-stage non-small cell lung cancer. But for high-risk patients, the dangers may outweigh the benefits. Researchers developed a risk prediction score that takes into account factors such as age, body mass index, health history, and cancer characteristics. They tested the new tool using data from nearly 10,000 Veterans who underwent lung cancer surgery between 2006 and 2016. The risk score was able to accurately predict which patients were likely to die within 90 days of surgery. The tool could help surgeons and patients assess risk and decide between surgery and other cancer treatments, say the researchers. (Annals of Surgery, Oct. 17, 2022)
|
Paxlovid lowers risk of Long COVID
 Photo: ©Getty Images/portishead1 (11/09/2022)
The antiviral medication Paxlovid lowers the risk of developing Long COVID, according to a VA St. Louis study. The study reviewed the records of more than 56,000 Veterans with a positive COVID-19 test. Those given Paxlovid within five days of infection—a medication that can reduce the risk of severe COVID-19 and hospitalization—had a 25% decreased risk of developing 10 of 12 different Long COVID conditions. Paxlovid was associated with a decreased risk of long COVID for both a first COVID-19 infection and a reinfection, and also for individuals who were unvaccinated, vaccinated, or boosted. Paxlovid could be an important asset to address the serious issue of Long COVID, say the researchers. The study was released as a pre-print in the interest of public health. (medRxiv, Nov. 5, 2022)
|
Younger and female LGBTQ+ Veterans less likely to use VA health care
 Photo: ©Getty Images/PeopleImages (11/09/2022)
Younger and female LGBTQ+ Veterans may be less likely to use VA health care than cisgender, heterosexual Veterans, found a VA study. Researchers analyzed data on more than 20,000 Veterans who completed a survey on health care use. Overall, both LGBTQ+ and non-LGBTQ+ Veterans used VA or military care as their primary health care at about the same rates. LGBTQ+ Veterans age 34 or younger were significantly less likely than young non-LGBTQ+ Veterans to use VA or military health care, 25% versus 44%. Only about 13% of female LGBTQ+ Veterans used VA or military health care, compared to 29% of non-LGBTQ+ female Veterans. Future studies should examine the potential reasons for these disparities, say the researchers. (Health Services Research, Nov. 4, 2022)
|
PTSD, depression linked to accelerated brain aging
 Photo: ©Getty Images/AlexSava (11/09/2022)
Psychiatric disorders may be linked to accelerated cellular aging in the brain, according to a VA Boston study. Psychiatric and traumatic stress have been associated with biological aging of cells that outpaces chronological aging. Researchers used RNA sequencing to look at the gene expression in brain tissue from the VA National PTSD Brain Bank. They found that tissue in a region of the brain called the ventromedial prefrontal cortex from patients with PTSD or depression had more signs of advanced cellular age compared with samples from people without psychiatric conditions. PTSD and depression were also linked to increased biomarkers related to inflammation and immune response. The results suggest that inflammation and immune system dysregulation could be responsible for accelerated brain aging caused by psychiatric disorders, say the researchers. (Depression and Anxiety, Oct. 25, 2022)
|
E-cigarettes may weaken muscle strength and healing
 Photo: ©Getty Images/6okean (11/03/2022)
E-cigarette use may weaken muscle strength and healing, according to a study by VA San Diego researchers and colleagues. E-cigarettes use a heated aerosol mixture to deliver nicotine. Smoking E-cigarettes, also called vaping, has been linked to harmful effects such as lung injury and inflammation. To study how vaping affects muscle function, researchers exposed mice to nicotine-containing aerosol. Those exposed to the vapor had reduced leg muscle force and running speed. They also only recovered 80% of muscle strength after an overuse injury. Exposure to the chemicals used to dissolve nicotine in vapes, polyethylene glycol and vegetable glycerin, decreased running speed and prevented full recovery from injury even when no nicotine was included. The results suggest that both nicotine and the chemicals used in E-cigarettes are harmful to muscle function, say the researchers. (American Journal of Physiology, Oct. 17, 2022)
|
Mandatory vaccination of health care workers lowers flu risk
 Photo: ©Getty Images/SDI Productions (11/03/2022)
Mandatory vaccination lowers flu infection in health care workers, found a study by VA researchers and colleagues. The study compared flu rates at four VA health care system outpatient sites—which do not require employees to get a flu shot—with three non-VA health system facilities with mandatory flu vaccination. About 63% of employees at the VA facilities were vaccinated, compared with 93% at the other sites. Analysis showed that flu infections would have been reduced by 52% at the VA sites if they had the same level of vaccination as the non-VA sites. However, flu vaccination was associated with an increased risk of other respiratory viral infections. Mandatory flu vaccination of health care workers could lower risk of the flu, say the researchers, but the increase of other infections needs further research. (Infection Control and Hospital Epidemiology, September 2022)
|
Sleep problems from traumatic brain injury lead to lower life participation
 Photo: ©Getty Images/Viacheslav Peretiatko (11/03/2022)
Sleep problems related to mild traumatic brain injury lead to lower social and community participation, found a VA Rocky Mountain study. Out of nearly 9,000 Veteran participants with mild TBI, 87% had sleep problems. Sleep problems were linked with greater social and community participation restrictions. Two TBI symptoms, anxiety and forgetfulness, largely affected this association. Sleep problems were also linked with lowered productivity due to headaches and forgetfulness. The findings suggest that sleep treatment should play a prominent role in rehabilitation for Veterans with mild TBI, say the researchers. (Frontiers in Rehabilitation Sciences, October 12, 2022)
|
Bacteria transplantation could treat alcohol use disorder
 Photo: ©Getty Images/Savushkin (10/27/2022)
Gut microbe transplant could reduce alcohol consumption and help treat alcohol use disorder, suggests a study by a team including Richmond VA researchers. Previous research suggests that fecal transplant to introduce helpful bacteria to the digestive tract can reduce alcohol cravings in people with alcohol use disorder. The researchers introduced stool from a human trial into mice. Those colonized with helpful bacteria showed less interest in alcohol than those given a sterile control substance. Fecal transplants from humans with more types of gut microbes were linked to lower alcohol intake in mice. Those mice showed changes in immune response, inflammation, and other changes in the intestine. The findings suggest that targeting gut bacteria could lead to treatments for alcohol use disorder, say the researchers. (Nature Communications, Oct. 19, 2022)
|
Clinician views on medication reconciliation
 Photo: ©Getty Images/fotostorm (10/27/2022)
VA researchers developed a questionnaire to assess medication reconciliation programs in VA. Medication reconciliation can detect prescription discrepancies and help avoid negative drug events. However, organizations often struggle to implement reconciliation programs. The researchers developed at 21-question survey and distributed it to nearly 9,000 clinicians at 142 VA sites. Most staff agreed that medication reconciliation could improve drug safety. However, 90% expressed concerns about changes to workflow. One-third of respondents said they prioritized other duties over medication reconciliation. Only 47% said they had enough resources to address problems. This questionnaire can help identify barriers to medication reconciliation programs and lead to safer prescribing to Veterans, say the researchers. (BMJ Quality Open, October 2022)
|
More intensive chronic pain treatment may be needed for Black Veterans with mental health disorders
 Photo: ©Getty Images/supersizer (10/27/2022)
Black Veterans with mental health disorders were more engaged in treatment than those without mental health disorders in a study on chronic pain, found an Atlanta VA study. However, Veterans with mental health disorders did not experience reductions in pain-related disability. Researchers looked at outcomes for Black Veterans who participated in a walking program designed to treat chronic pain. The program involved telephone coaching sessions to encourage walking. Participants with mental health disorders, such as PTSD and depression, were more likely to complete the coaching sessions. They also reported improvements in how they perceived their pain and its interference with their lives. However, six months later, the intervention was only associated with improved pain-related disability in patients without mental health disorders. The results suggest that Black Veterans with mental health disorders may require more intensive treatment for chronic pain, according to the researchers. (Journal of Pain, Sept. 23, 2022)
|
Hepatitis C medications linked to lower alcohol use
 Photo: ©Getty Images/FatCamera (10/17/2022)
Hepatitis C medications were linked to lower alcohol use in patients with alcohol use disorder and PTSD, in a study by White River Junction VA researchers. The study looked at alcohol use in more than 1,000 patients with co-occurring alcohol use disorder and PTSD. All patients were taking one of three direct-acting antivirals for hepatitis C infection. All three medication groups showed substantial reductions in alcohol use. Treatment with ledipasvir/sofosbuvir led to the highest frequency of clinically meaningful alcohol use improvement. The results suggest that further exploration of direct-acting antivirals in alcohol use disorder treatment is warranted, say the researchers. (Journal of Dual Diagnosis, Sept. 23, 2022)
|
Multiple factors affect social integration in Veterans recovering from homelessness
 Photo: ©Getty Images/jeremyiswild (10/17/2022)
VA Greater Los Angeles researchers and colleagues identified factors associated with recovery from homelessness among Veterans in permanent supportive housing. The Department of Housing and Urban Development-VA Supportive Housing program provides permanent housing, financial subsidies, and supportive services to Veterans experiencing homelessness. Previous studies have shown that full “recovery” from homelessness requires social integration. Among Veterans using the program, health-related quality of life, psychiatric symptoms, and case management frequency affected how well Veterans integrated into their communities. Most participants did not perceive HUD-VASH services as relevant to their social integration. More services that enhance social integration may help Veterans recover from homelessness, say the researchers. (Journal of Community Psychology, July 2022)
|
Veterans continue to find tinnitus management skills useful
 Photo: ©Getty Images/Aleksej Sarifulin (10/17/2022)
Veterans continue to use skills learned in tinnitus management workshops up to 10 years after learning them, according to a Bay Pines VA study. Tinnitus refers to ringing or other sounds heard when no external sound is present. It is the most common service-connected disability in Veterans. Researchers followed up with Veterans who completed VA’s progressive tinnitus management workshops in 2010 to 2014. Progressive tinnitus management teaches Veterans to manage tinnitus with therapeutic sound, relaxation, planning pleasant activities, and changing thoughts and feelings. The follow-up showed that more than half of respondents used all four self-managements skills 10 years later. About 69% said they were better able to control their reactions to tinnitus. Most said that the workshop experience was positive, and 89% said they would recommend the workshop to someone with bothersome tinnitus. The results suggest that skills learned in the workshop continue to be useful for Veterans with tinnitus, say the researchers. (American Journal of Audiology, September 2022)
|
COVID-19 increases risk of neurologic disorders
 Image: ©Getty Images/nopparit (10/06/2022)
COVID-19 increases the risk of long-term neurologic disorders, according to a VA St. Louis study. Researchers compared data on over 150,000 VA patients who contracted COVID-19 with more than 11 million people who did not. A year after recovering from COVID-19, individuals had a higher risk of a wide array of neurologic conditions, including stroke, memory disorders, nervous system disorders, episodic disorders like migraines and seizures, Guillain-Barré syndrome, and sensory disorders. Following COVID-19 infection, individuals had elevated risks and burdens even when they did not require hospitalization during their illness. The results highlight a need for health care system planning to address the potential long-term consequences of COVID-19, say the researchers. (Nature Medicine, Sept. 22, 2022)
|
Traumatic brain injury linked to less social support
 Photo: ©Getty Images/AsiaVision (10/06/2022)
Veterans who screen positive for traumatic brain injury (TBI) receive less social support than those who screen negative, according to a study by VA San Diego researchers. The study included nearly 10,000 Veterans participating in the Million Veteran Program. Those who screened positive for TBI reported significantly lower levels of social support compared with those who screened negative. Lower levels of social support were associated with more severe neurobehavioral and psychiatric symptoms and worse cognitive functioning. Psychiatric symptoms appeared to control the link between TBI status and social support. The results show the importance of considering social support when treating Veterans with TBI, say the researchers. (Social Science & Medicine, Sept. 16, 2022)
|
Fracture risk in older men
 Photo: ©Getty Images/angkhan (10/06/2022)
A study by Minneapolis VA researchers and colleagues identified the strongest risk factors for hip fractures in elderly men. The five-year study followed more than 3,000 men who were 80 years or older. Fall history, body mass index, and recent fractures were found to be strong risk factors for hip fracture. Age and having multiple health conditions were the strongest predictors of death in the study group. Age, body mass index, and fall history were associated with both hip fracture and death. Identifying men in later-life who would benefit from treatment to prevent fracture is challenging because of high death rates. The findings suggest that decisions about osteoporosis drug treatment should consider fracture risk versus overall life expectancy, according to the researchers. (Journal of Gerontology, Aug. 2, 2022)
|
New prediction model to estimate risk of COVID-19 death
 Photo: ©Getty Images/FG Trade (09/29/2022)
VA researchers developed a new prediction model to estimate the probability of death from COVID-19. The mathematical model, called PDeathDx, uses diagnostic codes from medical records to survey all of a patient's preexisting conditions to estimate the risk that COVID-19 poses. Starting with data from 1997, the researchers used diagnoses from the first time a patient sought care until 14 days before a positive COVID-19 test, then compared that to COVID outcomes for nearly 350,000 patients treated in VA. They found that the new model outperformed other conventional prediction models. The study also showed that certain underlying conditions—such as neurological diseases, dementia, and severe disability—are much more likely to result in severe COVID or death. The approach used here could be adapted to predict outcomes for other diseases and conditions, say the researchers. (Biological Methods & Protocols, Aug. 4, 2022)
|
Whole health care model could reduce suicide risk
 Photo: ©Getty Images/ljubaphoto (09/29/2022)
A whole health model shows promise to reduce suicide risk and need for mental health services for Veterans with psychiatric illnesses, found a study by VA Salt Lake City researchers. However, whole health services were found to be underutilized. Whole health is a health care model that focuses on health promotion and disease prevention rather than disease treatment only. VA is implementing this model in its health care system. Researchers looked at outcomes for over 7,000 Veterans with a mental health diagnosis. Whole health interventions included mindfulness training, health education, nutrition classes, and health coaching. Only 305 Veterans had at least one whole health appointment. Whole health participation was associated with decreased risk of suicide and reduced use of mental health services. The findings suggest that a whole health approach could benefit Veterans with mental illness, but more efforts are needed to increase patient engagement, say the researchers. (Complementary Therapies in Medicine, Sept. 9, 2022)
|
Using social media to recruit loved ones to Veteran suicide prevention training
 Photo: ©Getty Images/Tero Vesalainen (09/29/2022)
Social media could be a useful tool to recruit Veterans’ loved ones in suicide prevention training, found a VA Portland study. Researchers used Facebook sponsored ads to recruit Veterans’ friends and family for VA’s free suicide prevention training module. The team was able to meet two benchmarks: enrolling an average of 20 participants a week and less than 50% loss to follow-up at the end of the 6-month study. Focusing on family and friends, an urgent call to action to help a Veteran, prior exposure to suicide, emphasizing the benefit of the training, and using a university as messenger all helped recruit participants. Recruitment barriers included generic ads, referring to “research” in the text, and Facebook as the ad platform. The results show that this approach is feasible, say the researchers, and the next step is to measure the training effectiveness with a larger group. (Contemporary Clinical Trials Communication, Sept. 5, 2022)
|
Institutional betrayal linked to suicidal behavior
 Photo: ©Getty Images/Cunaplus_M.Faba (09/22/2022)
Institutional betrayal is linked to suicidal behavior and worse mental health in women who experienced military sexual trauma, according to a Rocky Mountain Regional VA Medical Center study. Institutional betrayal refers to harm caused by an institution (such as the military) to someone dependent on that institution. Researchers surveyed 229 women Veterans who screened positive for military sexual trauma. Those who felt a sense of institutional betrayal had increased odds of suicidal thoughts and attempts following their military service. They also had more severe depression and PTSD symptoms. Institutional betrayal was not linked to non-suicidal self-injury or substance misuse. The results underscore the need to address institutional betrayal among women who experience military sexual trauma, say the researchers. (Journal of Trauma & Dissociation, Sept. 7, 2022)
|
Health records inaccurate on drug overdoses
 Photo: ©Getty Images/megaflopp (09/22/2022)
Nonfatal drug overdoses are underreported in health records, found a study by Birmingham VA researchers and colleagues. Researchers compared self-reported overdoses over three years with diagnostic codes in the medical records of Veterans receiving care both in VA and in the community. Only about 28% of alcohol, 23% of sedative, 12% of opioid, and 6% of cocaine overdoses were recorded with diagnostic codes. Veterans with substance use disorder diagnoses were more likely to self-report overdoses. The findings support the need for alternative approaches to overdose surveillance in public health, according to the researchers. (American Journal on Addictions, Aug. 24, 2022)
|
Traumatic brain injury may increase risk of cardiovascular disease
 Image: ©Getty Images/peterschreiber.media (09/22/2022)
Veterans who have had a traumatic brain injury (TBI) had increased odds of developing cardiovascular disease, found a study by VA researchers and colleagues. The study analyzed data on more than 1.5 million Veterans, including over 300,000 with a history of TBI. Those with TBI history were more likely to develop cardiovascular disease. All levels of TBI increased the risk of stroke, coronary artery disease, and peripheral artery disease. Both mild and moderate to severe TBI were associated with increased risk of death due to cardiovascular disease. The results suggest that Veterans who have sustained a TBI may have increased burden of cardiovascular disease as they age, say the researchers. More study is needed to determine whether this increased risk can be modified. (JAMA Neurology, Sept. 6, 2022)
|
PTSD symptoms linked to suicide risk
 Photo: ©Getty Images/Suriyawut Suriya (09/14/2022)
Improving PTSD symptoms can reduce the risk of suicide, found a study by White River Junction VA researchers and colleagues. The study included data on more than 750,000 Veterans diagnosed with PTSD between 1999 and 2018. Researchers found that any level of PTSD symptoms was linked to double the rate of death by suicide one month after assessment, compared to those without PTSD symptoms. Worsening PTSD symptoms were associated with a 25% greater long-term suicide mortality rate. Veterans who achieve remission from PTSD had a much lower suicide rate than those who still had PTSD symptoms. The results show lowering PTSD symptoms can reduce suicide risk, say the researchers, but only if Veterans reach remission levels. (British Journal of Psychiatry, Aug. 23, 2022)
|
Intensive lifestyle intervention improves diabetes in older adults
 Photo: ©Getty Images/kitzcorner (09/14/2022)
A lifestyle intervention strategy can be highly effective for older adults with diabetes, according to a Michael E. DeBakey VA Medical Center study. One hundred older adults with diabetes were assigned either one year of intensive lifestyle intervention or healthy lifestyle control treatment. The lifestyle intervention involved a weight management program and exercise training, including weekly interactions with dietitians and trainers. The control treatment consisted of group educational sessions about a healthy diet. A1c, a measure of diabetes control, improved significantly more in the intervention group. This group also saw greater weight loss and better performance on physical performance tests. Participants in the lifestyle intervention group were also able to decrease their insulin doses. The results show that an intensively managed lifestyle intervention can help improve older diabetic patients’ health and quality of life, say the researchers. (Diabetes Care, Sept. 1, 2022)
|
Patient engagement video improves telehealth visits
 Photo: ©Getty Images/Yaroslav Olieinikov (09/14/2022)
A pre-visit video before a telehealth appointment can improve patient communication and outcomes, found a VA study. Use of video for medical appointments has increased drastically in recent years, especially during the COVID-19 pandemic. While telehealth can improve access to care, lack of in-person contact can affect patient engagement. Researchers had patients watch a pre-visit video promoting active communication before video appointments. Patients who watched the video rated their physicians’ communication and empathy higher than those who only received a pamphlet on the subject. They also were more engaged in their care and showed a stronger cooperative relationship with their doctors. The results show that training patients about engagement and active communication can improve the telehealth experience, according to the researchers. (PEC Innovation, Sept. 12, 2022)
|
Melatonin may lower risk of death from sepsis
 Photo: ©Getty Images/Tempura (09/12/2022)
Melatonin lowered the risk of death from sepsis, in a Columbia VA study. Sepsis is a potentially life-threatening condition in which chemicals released by the body to fight infection damage its own tissue. Prior research has suggested that melatonin—a hormone related to sleep regulation—could benefit sepsis patients. The researchers studied data on more than 9,000 patients admitted to the hospital with sepsis. Those given melatonin within the first day of hospitalization had a 38% reduced risk of 30-day, in-hospital mortality, compared with those not given melatonin. The findings suggest that melatonin may have important effects beyond sleep regulation and could be a useful treatment for sepsis, say the researchers. (Journal of Pineal Research, September 2022)
|
Use of complementary and integrative health for Gulf War illness
 Photo: ©Getty Images/ljubaphoto (09/12/2022)
Many Veterans with Gulf War illness use complementary and integrative health (CIH) treatments, found a VA study. CIH practices include non-mainstream care such as acupuncture, yoga, and chiropractic care. Researchers looked at health care data on more than 1,000 Gulf War-era Veterans. Over half had used at least one CIH approach in the last six months. Women Veterans, white Veterans, and Veterans with higher levels of education were the most likely to use CIH. Those with a Gulf War illness diagnosis and higher symptom severity were more likely to use CIH. Over three-quarters of Veterans who used CIH to treat Gulf War illness symptoms said it was helpful. About 72% indicated that they would use CIH approaches if they were available at VA. The results could inform decisions on expanding CIH treatments for Veterans, say the researchers. (Complementary Therapies in Clinical Practice, July 31, 2022)
|
Robot-assisted surgery increasing in VA
 Photo: ©Getty Images/sompong_tom (09/12/2022)
The use of robot-assisted surgery in VA has increased significantly, according to a VA study. Researchers looked at data on three common surgery types performed in VA. Out of more than 100,000 surgeries, nearly 5% used robotics during the five-year study period. The proportion of robotically assisted surgeries increased from 1.5% to 10.5% from 2015 to 2019. Hernia repair surgery had the greatest increase in robotic use. The Northeast, Midwest, and West Coast of the United States saw the largest increases in robotic use. The results suggest that VA continues to be at the forefront of medical research and innovation, according to the researchers, but the reasons for regional differences should be investigated. (Journal of Surgical Research, Aug. 11, 2022)
|
Sense of belonging increases Veteran engagement with VA care
 Photo: ©Getty Images/Drazen Zigic (08/24/2022)
VA Portland researchers identified factors that strengthen Veterans’ sense of belonging in the VA health care system. The study team interviewed 27 VA patients. They found that a sense of belonging promotes appointment attendance and patient engagement. The Veterans identified three factors that related to a sense of belonging. Feelings of camaraderie and commitment toward other Veterans improved the patient experience. Interactions with all staff influenced the engagement a patient felt toward a particular clinic and VA. And personalized communication and messaging can humanize VA and demonstrate its interest in engaging with Veterans. Continuing to strengthen patients’ sense of belonging can help increase appointment attendance and engagement in VA care, according to the researchers. (Medical Care, July 26, 2022)
|
Most young non-daily cigarette smokers continue to smoke
 Photo: ©Getty Images/Miljan Zivkovic (08/24/2022)
Most young adults who smoke cigarettes intermittently continue the habit and may need help quitting, according to a study by VA San Diego researchers and colleagues. Increasing evidence shows that non-daily cigarette smoking is common in early adulthood. Researchers assessed 579 non-daily smokers between the ages of 18 and 24 for three years. They found that 55% smoked intermittently throughout the study. About 43% consistently stopped smoking by the end of the study. Few from either group transitioned to daily smoking. Quitting smoking was associated with having fewer smoking friends, smoking less in social situations, experiencing lower positive reinforcement from smoking, and having a stronger intent to quit. The findings suggest that efforts to get young adults to quit smoking should focus on reducing expectations of positive effects and social motivations of smoking, say the researchers. (Nicotine & Tobacco Research, Aug. 5, 2022)
|
Prescription opioid use disorder treatment lowers death risk compared with methadone
 Photo: ©Getty Images/Tashatuvango (08/24/2022)
A prescription medication used to treat opioid use disorder may lower the risk of death compared with methadone, found a White River Junction VA study. Opioid agonist treatments (OATs) are medications that reduce opioid withdrawal and cravings. Methadone is usually given at a treatment facility as a daily liquid dose. Buprenorphine can be prescribed and does not require observed dosing like methadone. Researchers looked at outcomes for nearly 62,000 VA patients with opioid use disorder taking one of the two treatments. Buprenorphine was linked to a 20% lower risk of death from any cause compared to methadone, and a 40% lower risk of suicide. The rates of death from overdose were similar with the two treatments. The results support less restrictive buprenorphine prescribing to help patients with opioid use disorder, say the researchers. (Acta Psychiatra Scandinavia, July 15, 2022)
|
Drug may help treat lupus skin damage
 Photo: ©Getty Images/Jovanmandic (08/18/2022)
A team including a Corporal Michael J. Crescenze VA Medical Center researchers identified a drug that may help treat a form of lupus that involves the skin. Lupus is an autoimmune disease, in which the body’s immune system attacks its own tissue. One form, cutaneous lupus erythematosus, can cause irreversible skin damage. The researchers compared outcomes for patients with lupus treated with a drug called litifilimab and those given a placebo. Those treated with the drug showed improvements in skin disease severity, compared to the placebo group. While larger trials are needed, the results suggest that litifilimab may be a useful treatment for this type of lupus, say the researchers. (New England Journal of Medicine, July 28, 2022)
|
Firearm safety discussions rare in Veteran health care
 Photo: ©Getty Images/Creatas (08/18/2022)
Most Veterans who own firearms have not had firearm safety discussions with a health care provider, according to a study by Rocky Mountain Regional VA Medical Center researchers. Seventy percent of suicides among Veterans involve firearms. Because of this, suicide prevention guidelines recommend addressing firearm safety during medical care. The study surveyed Veterans who owned firearms on whether they have had this discussion. About 32% of Veterans surveyed used VA health care. Overall, only 9% reported a health care provider speaking to them about firearm safety. About 14% of those who used VA care and 7% of those who did not use VA said they discussed firearm safety. The findings suggest that additional efforts are needed to increase these safety discussions, say the researchers. (Suicide & Life-Threatening Behavior, Aug. 4, 2022)
|
HIV may increase risk of head and neck cancers
 Photo: ©Getty Images/Lars Neumann (08/18/2022)
Veterans with HIV/AIDS may have increased risk of head and neck cancers, found a study by Michael E. DeBakey VA Medical Center researchers and colleagues. The study looked at VA patient data from 1999 to 2016. It included more than 45,000 Veterans with HIV/AIDS and over 160,000 HIV-negative Veterans. Those with HIV/AIDS had nearly twice the risk of head and neck cancers. Veterans with HIV/AIDS were more likely to be human papilloma virus (HPV)-positive than HIV-negative Veterans. The results suggest that HIV may play a role in the development of head and neck cancers, including those caused by viruses such as HPV, according to the researchers. (Cancer, July 22, 2022)
|
COVID-19 boosters effective against Omicron and Delta variants
 Photo: ©Getty Images/andresr (08/09/2022)
COVID-19 vaccine boosters were highly effective against recent virus variants, found a study by VA White River Junction researchers and colleagues. The study included data on more than 110,000 Veterans, mostly older and male, who had a COVID test between November 2021 and January 2022. Protection against both the Omicron and Delta COVID-19 variants was better in those who also had a booster dose of an mRNA vaccine, compared with those who only had a two-dose vaccine. Boosters were 64% effective against Omicron infection, while initial vaccination was only 12% effective. For the Delta variant, vaccinations with a booster were 90% effective against infection, versus 54% for initial vaccination. For preventing hospitalization, booster doses were 89% effective during the Omicron period and 94% effective during the Delta period, compared with the two-dose vaccines, which were 63% effective against Omicron and 75% effective against Delta. For preventing death, vaccines combined with a booster dose were 94% effective against Omicron and 96% against the Delta variant. The results show that vaccine boosters increase the effectiveness of COVID-19 vaccination against infection, hospitalization, and death, according to the researchers. (BMJ Open, Aug. 3, 2022)
|
Using AI to predict suicide risk
 Photo: ©Getty Images/FG Trade (08/09/2022)
Analyzing electronic health records with artificial intelligence could help predict which Veterans are at risk for suicide, found a VA White River Junction study. Researchers applied natural language processing (NLP) to VA electronic health records from 2015 and 2016. NLP is a branch of artificial intelligence that teaches computers to understand the way that humans speak and write language. The NLP technique was applied to unstructured health records, which are clinician-written notes that do not include key words and diagnostic codes. The NLP computer model was accurate at predicting which Veterans in the sample population died by suicide. It correctly predicted 74% of suicide cases in the study sample. This approach has potential to improve the accuracy of suicide risk prediction, say the researchers. (Psychiatry Research, July 1, 2022)
|
Web tool could help reduce medication discrepancies
 Photo: ©Getty Images/DNY59 (08/09/2022)
A secure patient messaging system has potential to help reduce medication discrepancies, according to a study by VA Boston researchers and colleagues. Medication discrepancies, such as incorrect prescriptions dosages, can lead to adverse drug effects and patient harm. The researchers developed a web-based tool to help identify and fix medication discrepancies when patients transition from hospital to home. The team surveyed 20 Veterans who received care at a VA medical center about their experiences with the messaging system. Most patients found it was easy to use at home and liked the fact that they could review medications at their own pace. They added that it was helpful at clarifying medication directions and dosages, and for removing incorrectly listed medications from their electronic health records. Some Veterans struggled to use the portal due to technology-related barriers. Adoption of the secure messaging tool in clinical practice could reduce medication discrepancies, say the researchers. (JMIR Human Factors, Aug. 3, 2022)
|
Underlying risk factors may explain racial/ethnic differences in PTSD recovery
 Photo: ©Getty Images/Drazen Zigic (08/08/2022)
Underlying social risk factors may explain racial/ethnic differences in mental health recovery after a traumatic event, according to a study by VA Palo Alto researchers and colleagues. More than 1,300 patients were assessed for PTSD after a severe injury. Hispanic, Black, and multiracial participants had higher PTSD symptoms than white patients. Symptoms remained higher in Black and multiracial patients six months after hospitalization. PTSD symptoms improved faster in Hispanic than in white patients. Risk factors such as discrimination, financial stress, and past mental health problems accounted for most of the differences between groups. Addressing these risk factors could reduce disparities in PTSD recovery, say the researchers. (Psychological Medicine, July 29, 2022)
|
Arm prosthetic satisfaction survey adapted to capture women’s needs
 Photo: ©Getty Images/Georgijevic (08/08/2022)
VA Providence researchers and colleagues modified an upper-limb prosthetic satisfaction survey to make it more responsive to women. Women with an upper-arm amputation are more likely than men to stop using their prostheses. The researchers added items specifically tailored to women to a widely used survey on prosthetic use and satisfaction. The new survey questions addressed topics such as device size, appearance, and fit under clothes. The updated survey showed good reliability in a test of 468 participants with amputation. The researchers recommend that new comfort and appearance subscales be added to the assessment in clinical use to better address the concerns of women prosthetic users. (Archives of Physical Medicine and Rehabilitation, June 12, 2022)
|
Less diabetes medication not linked to worse outcomes for Veterans in nursing homes
 Photo: ©Getty Images/PIKSEL (08/08/2022)
Reducing diabetes medication in older Veterans residing in nursing homes did not lead to worse outcomes, in a study by VA Pittsburgh researchers. Guidelines advise against tight glycemic control in diabetic patients with advanced dementia or limited life expectancy. Researchers analyzed data on more than 2,000 older diabetic Veterans living in nursing homes. Of those, 27% had their diabetes medications de-intensified. Veterans taking less medication had similar rates of emergency room visits, hospitalization, and death as those taking higher doses. The results suggest that reducing diabetes treatment could be a way to lower medication burden and avoid overtreatment in this population, say the researchers. (Diabetes Care, July 7, 2022)
|
High antibiotic, opioid prescribing linked
 Photo: ©Getty Images/stevecoleimages (07/27/2022)
High antibiotic prescribing is associated with high opioid prescribing at health care facilities, according to a VA study. Over-prescribing of antibiotics can lead to drug-resistant infections. Opioid over-prescribing is linked to addiction and overdose. Researchers looked at VA electronic health records prescribing data for both medical providers and dentists. They found that providers that prescribed the most antibiotics were also the highest prescribers of opioids. For medical providers, older age, region of the country, lower VA facility complexity, and rurality were linked with higher opioid prescribing. In dentists, younger age, male gender, specific region of the country, and lower number of dentists at a facility were linked to higher opioid prescribing. The results suggest that efforts targeting both medication classes may improve prescribing practices, say the researchers. (Pharmacotherapy, July 22, 2022)
|
Vets with mental health conditions have less fragmented health care
 Photo: ©Getty Images/mixetto (07/27/2022)
Having a mental health condition was linked to less fragmented health care, in a study by VA Palo Alto researchers and colleagues. Health care fragmentation—seeing many different providers—can lead to worse health complications. Health care providers worry that mental health conditions could amplify this problem. The researchers looked at more than 125,000 older VA patients also enrolled in Medicare. Contrary to what the researchers expected, patients with mental health conditions had less fragmented non-mental health care than those without mental health conditions. Those with mental health conditions saw fewer providers and had their care concentrated more with their primary provider. The finding could suggest higher quality care but also could indicate underuse of medical care in these patients, explain the researchers. (Journal of General Internal Medicine, July 22, 2022)
|
Toxic exposure may be linked to infertility
 Photo: ©Getty Images/sasacvetkovic33 (07/27/2022)
Toxic exposure during military service may be linked to infertility, according to an Iowa City VA study. Researchers surveyed both male and female Veterans between the ages of 20 and 45. In both men and women, those who reported environmental, chemical, and hazardous exposures during military service had increased rates of infertility. Toxic exposures linked to infertility included petrochemicals and polychlorinated biphenyls, chemicals known to cause cancer and birth defects. Veterans reporting infertility also had a higher number of total exposures. While causation between toxic exposure and infertility cannot be proven, say the researchers, more research between a possible link is needed. (American Journal of Obstetrics and Gynecology, July 13, 2022)
|
Pre-surgery lung cancer care linked to better survival
 Photo: ©Getty Images/shironosov (07/12/2022)
Inadequate access to pre-operative care is linked to worse lung cancer outcomes, found a VA St. Louis study. Quality pre-surgery care measures included timely surgery, imaging, smoking management, and lung function testing. Researchers looked at care quality measures for nearly 10,000 VA patients undergoing surgery for non-small cell lung cancer. About 35% received all four quality measures. Those who received these measures were significantly less likely to die after surgery, compared to patients not receiving all measures. Black patients, those from poorer areas, and those who lived farther from the hospital were less likely to receive the four quality measures. The results show that VA should focus on providing more equitable pre-surgery care for Veterans with lung cancer, say the researchers. (Annals of Thoracic Surgery, June 17, 2022)
|
Bad cholesterol may be risk factor for Alzheimer’s
 Photo: ©Getty Images/angelp (07/12/2022)
High cholesterol may be involved in the development of Alzheimer’s disease, according to a study by an Atlanta VA researcher and colleagues. The gene APOE is a risk factor for Alzheimer’s and is also associated with high low-density lipoprotein (LDL) cholesterol, also called “bad” cholesterol. Researchers followed 559 participants who developed dementia for seven years. They found that LDL cholesterol levels were associated with all measures of Alzheimer’s progression. The findings suggest that LDL cholesterol is involved in Alzheimer’s independent of APOE. Cholesterol could be a modifiable risk factor for Alzheimer’s disease, they say. (Journal of Neurology, Neurosurgery, and Psychiatry, June 30, 2022)
|
Leg power, grip strength predict fall injury risk in older men
 Photo: ©Getty Images/Mladen Zivkovic (07/12/2022)
Lower leg power and grip strength can predict fall injury risk in older men, according to a study including a VA Palo Alto researcher. In a study of more than 5,000 older men, 40% had at least one fall injury over a nine-year period. Those with lower leg power, as measured by a leg press, had an increased risk of fall injury. Weaker hand grip strength was also linked to greater risk of fall injury. Both measures predicted future fall injury risk independent of physical performance on a walking speed test. Leg power may identify fall injury risk better than grip strength, according to the researchers, but grip strength may be easier to measure in a clinical setting. The results suggest muscle strength decline likely precedes functional impairments, they say. (Journals of Gerontology, Series A, June 5, 2022)
|
PTSD avoidance symptoms linked to alcohol cravings
 Photo: ©Getty Images/FotoDuets (07/07/2022)
PTSD avoidance symptoms and alcohol cravings may be linked, found a Coatesville VA Medical Center study. PTSD and alcohol or substance use disorders often occur together. Researchers interviewed 167 Veterans to see whether specific PTSD symptoms were linked to drug or alcohol misuse. Avoidance, in which patients distance themselves from things that could remind them of their trauma, was significantly linked with alcohol cravings. No specific PTSD symptoms were linked to stimulant drug cravings. Veterans with avoidance symptoms may experience alcohol cravings because they believe alcohol will ease thoughts, feelings, or reminders of trauma, according to the researchers. This relationship should be considered when treating co-occurring PTSD and alcohol use disorder, they say. (Journal of Dual Diagnosis, June 27, 2022)
|
Low-value health services common in VA
 Photo: ©Getty Images/Kubra Cavus (07/07/2022)
More than 1 in 10 Veterans enrolled in VA health care received a low-value health service, according to a study of 5.2 million Veterans. Researchers looked at health care services delivered at VA facilities or paid for through VA in a single fiscal year. They analyzed the data for low-value care, meaning services with harms or costs that outweigh the benefits. About 14% of Veterans received low-value services. This added up to a total cost of $205.8 million. The most frequent low-value service was prostate-specific antigen testing—a blood test to detect prostate cancer—for men 75 or older. The most expensive low-value services were spinal injections for back pain and stenting for stable heart disease. The results can help guide VA’s efforts to reduce delivery and spending on low-value care, say the researchers. (JAMA Internal Medicine, July 5, 2022)
|
Stressful life events increase risk of Veteran suicide
 Photo: ©Getty Images/Jay Yuno (07/07/2022)
Stressful life events are a major factor in suicide attempts for Veterans recently separated from the military, found a VA study. Researchers looked at data on Veterans surveyed during active duty and again after separating from the military. About 15% of those surveyed were deemed high-risk for suicide attempts. Those at high risk of suicide where significantly more likely to experience post-separation stressful life events. These events included housing instability, legal problems, financial strain, and relationship problems. The link between stressful life events and actual suicide attempts was much stronger in the high-risk group, compared with those at lower risk for suicide. It might be possible to prevent some Veteran suicides by targeting interventions for common stressful life events, according to the researchers. (Psychological Medicine, May 27, 2022)
|
Sickle cell trait linked to increase risk of COVID-19 death
 Image: ©Getty Images/EzumeImages (06/29/2022)
Sickle cell trait is linked to an increased risk of death from COVID-19, found a VA Million Veteran Program study. People with sickle cell trait have one sickle cell gene and one normal gene. Those with the trait usually do not have symptoms of sickle cell disease—a blood disorder primarily affecting people of African descent. Researchers studied MVP data of nearly 3,000 people with sickle cell trait, 13% of whom contracted COVID-19. They compared them to nearly 130,000 people without sickle cell trait, 10% of whom had COVID-19. Those with sickle cell trait had higher odds of death from COVID-19. The sickle cell group also had increased rates of acute kidney failure. About 21% of COVID-19 deaths were due to acute kidney failure for patients with sickle cell trait. The results strongly support including sickle cell trait as a risk factor for worse COVID-19 outcomes, say the researchers. (JAMA Internal Medicine, June 27, 2022)
|
Barriers to positive airway pressure use
 Photo: ©Getty Images/cherrybeans (06/29/2022)
San Francisco VA researchers identified physical and psychological barriers to positive airway pressure use. Positive airway pressure (PAP) is an effective treatment for sleep apnea, but many patients have trouble tolerating it. Researchers interviewed 30 Veterans who did not use their PAP machines every day. The Veterans described physical and psychological barriers to use at about the same rate. The most common physical barriers were mask leaks and dry throat and nose. Psychological barriers included anxiety, claustrophobia, and worsening insomnia. Health care providers most often offered solutions for physical barriers. Solutions for psychological barriers were rarely proposed. The researchers recommend that patients receive individualized assessment to address both physical and psychological barriers to PAP use. (Translational Behavioral Medicine, May 30, 2022)
|
Poor diabetes control linked to weakened bones
 Photo: ©Getty Images/arinarici (06/29/2022)
Poor glycemic control is linked to bone weakness in men with diabetes, according to a study by Michael E. DeBakey VA Medical Center researchers and colleagues. The study assessed bone quality and strength in 169 men. Those with A1C—a measure of sugar levels in the blood—above 7% had higher trabecular separation and lower trabecular number than those with lower A1C scores. Trabecular bone tissue acts like a network of support beams that give bones their structure. Participants with high A1C also had worse measures of bone strength. They further had significantly lower bone turnover markers. Bone turnover, in which the body resorbs old bone tissue and produces new bone, helps the body maintain bone strength and health. A1C above 7% appears to be a threshold for bone impairment in men with diabetes, according to the researchers. (Calcified Tissue International, June 4, 2022)
|
Few differences in safety of Moderna, Pfizer COVID-19 vaccines
 Photo: ©Getty Images/Kanawa_Studio (06/23/2022)
Both the Moderna and Pfizer COVID-19 vaccines have a low risk of adverse events, found a study by VA Boston researchers. The study looked at data on more than 400,000 Veterans who were vaccinated. Risks were low after 38 weeks for either vaccine. Veterans receiving the Moderna vaccine were slightly less likely to experience stroke, heart attack, blood clots, or kidney damage. However, the difference was less than two-tenths of one percent. The results show that either vaccine is safe and effective for individuals, say the researchers, but the differences may help inform future population-level vaccination efforts. (JAMA Internal Medicine, June 13, 2022)
|
Airborne virus linked to hospital COVID-19 spread
 Photo: ©Getty Images/miodrag ignjatovic (06/23/2022)
Hospital COVID-19 infection may result from airborne virus particles introduced by employees and patients in common hospital areas, according to a study by VA Boston researchers and colleagues. The researchers studied the genome sequence of viruses from infected nurses and patients during a hospital COVID-19 outbreak. They compared these to virus particles from air samples. They learned that viruses found in nurses and patients were genetically identical to virus particles in the air. The findings suggest that very small, aerosolized virus particles can lead to COVID-19 spread in hospitals, according to the researchers. Isolating infected health care providers and improving ventilation and masking could help decrease the spread, they say. (JAMA Network Open, June 8, 2022)
|
Adverse childhood experiences linked to heart disease risk factors
 Photo: ©Getty Images/sanjagrujic (06/23/2022)
Adverse childhood experiences are linked to heart disease risk factors, according to a study by VA San Diego researchers. They analyzed data from more than 36,000 survey participants. Those who experienced childhood household dysfunction, mistreatment, or more than one adversity type were more likely to smoke tobacco, be overweight or obese, and have depression—all risk factors for cardiovascular disease. Having multiple childhood adversities was linked to the most risk factors, including high cholesterol and lipid levels. The results suggest that heart disease prevention programs should target these related risk factors together, say the researchers. (Stress and Health, May 26, 2022)
|
New treatment for antibiotic-resistant urinary tract infections
 Photo: ©Getty Images/Manjurul (06/08/2022)
Michael E. DeBakey VA Medical Center researchers and colleagues developed a treatment to combat urinary tract infections. Urinary tract infections from catheters affect one million patients per year in the United States. High rates of drug resistance make treating these infections difficult. The researchers created a cocktail containing phages, viruses that infect bacteria, to combat E. coli bacteria. The cocktail decreased cell viability of E. coli biofilms (layers of bacteria) isolated from the urine of spinal cord injury patients by 80%. Using antibiotics with the phage cocktail prevented or decreased bacteria infections in the urine of patients using catheters. This cocktail has high potential to treat antibiotic-resistant, catheter-associated urinary tract infections, say the researchers. (Frontiers in Microbiology, May 10, 2022)
|
Palliative care reduces suicide risk
 Photo: ©Getty Images/Kayoko Hayashi (06/08/2022)
Palliative care can help prevent suicide in Veterans at high risk for death from other causes, according to a Corporal Michael J. Crescenz VA Medical Center study. Palliative care refers to care aiming to improve quality of life and reduce symptom burden in patients with complex and life-shortening conditions. Researchers looked at VA data on more than 580,000 patients who had a high risk of death within a year. A high percentage of Veterans who died by suicide were diagnosed with chronic pulmonary disease, as well as mental health and substance use conditions. One palliative care consultation in the 90 days before death decreased the odds of suicide by 71%. Two or more consultations lowered the risk of suicide by 78%. The results highlight the importance of palliative care in preventing suicide for patients with serious illness, say the researchers. (Journal of Pain and Symptom Management, April 28, 2022)
|
Non-heterosexual Veterans at higher risk of disordered eating
 Photo: ©Getty Images/Tero Vesalainen (06/08/2022)
Non-heterosexual Veterans are more likely than heterosexual Veterans to have disordered eating, found a study by VA Boston researchers. The study surveyed over 800 female and over 500 male post-9/11 Veterans. Disordered eating—such as bulimia and binge eating disorder—was prevalent across gender and sexual orientation. Women identifying as bisexual and men identifying as gay had higher rates of disordered eating, compared to heterosexual Veterans. Experiencing discrimination in the military was linked to disordered eating. More research is needed on the causes of this disparity and the role of discrimination in disordered eating, according to the researchers. (International Journal of Eating Disorders, April 2022)
|
Vaccines only modestly reduce long COVID risk in breakthrough infection patients
 Photo: ©Getty Images/Drazen Zigic (06/02/2022)
Vaccines only modestly reduce the risk of long COVID in patients with breakthrough infection, according to a large study by VA St. Louis researchers. Long COVID refers to a wide range of ongoing health conditions that some people experience after recovering from COVID-19. Researchers studied data on nearly 34,000 people who had breakthrough COVID-19 infections after being vaccinated. They compared this group to more than 13 million controls. People with breakthrough infection had lower rates of death and long COVID symptoms six months after infection, compared to those who had never been vaccinated. However, breakthrough patients had a significantly higher risk of death and health problems compared to patients who never contracted COVID-19. These patients experienced many different symptoms, including cardiovascular, clotting, kidney, and mental health problems. The results show an urgent need to develop additional layers of protection beyond vaccines to protect against the long-term consequences of COVID-19, say the researchers. (Nature Medicine, May 25, 2022)
|
Role of immune system dysregulation in PTSD
 Image: ©Getty Images/image_jungle (06/02/2022)
A growing body of research shows that immune system dysregulation is an important contributor to PTSD, according to a review by VA Connecticut researchers. Recent research suggests that biological processes of the immune system contribute to PTSD. Researchers conducted a literature search and found 77 studies on the immune system response in PTSD. Traumatic experiences appear to cause dysregulation in the immune system that leads to inflammation in the brain and nervous system. Changes to gene expression could lead to hormones being produced that cause an inflammatory response in the brain, which is linked to PTSD symptoms. However, this dysregulation can be both pro-inflammatory and anti-inflammatory, depending on the patient. This shows that PTSD is a complex disorder than has many potential sub-types, say the researchers. More research is needed on the role of the immune system in PTSD, they say. (Biomedicines, May 10, 2022)
|
Exercise therapy lowers adverse outcomes from chronic pain
 Photo: ©Getty Images/bernardbodo (06/02/2022)
Exercise therapy lowers adverse outcomes in Veterans with chronic pain, found a VA study. Exercise therapy includes physical procedures such as stretching, strength training, and gait training. Researchers looked at data for nearly 94,000 soldiers with chronic pain who enrolled in VA health care after leaving the army. Those who attended at least eight sessions of exercise therapy for their pain while in the military had significantly lower risk of alcohol and drug disorders, suicidal thoughts, and death compared to those not given exercise therapy. This trend was especially true for those prescribed opioids before starting exercise therapy. The results suggest that exercise therapy should be considered as a non-drug treatment for chronic pain, according to the researchers. (Military Medicine, March 21, 2022)
|
Guilt reduction therapy effective treatment for PTSD
 Photo: ©Getty Images/Drazen Zigic (05/25/2022)
Therapy aimed at addressing guilt is an effective way to reduce posttraumatic symptoms and distress, found a VA study. Guilt is common after a traumatic experience and can even persist after PTSD treatment. Researchers compared two psychotherapies for reducing guilt in Veterans with guilt related to traumatic events during deployment to Iraq or Afghanistan. Trauma-informed guilt reduction helps patients accurately appraise their role in the trauma and re-engage with their values. Supportive care therapy focuses on understanding and support, without necessarily directly addressing guilt. While both therapies decreased guilt, the decrease was greater with the guilt-specific treatment. The guilt reduction method also was more effective at reducing PTSD and depression symptoms. Patients receiving trauma-informed guilt reduction had a higher likelihood of PTSD treatment response, loss of PTSD diagnosis, and meaningful change in depression. The results show that targeting a prominent symptom like guilt can be an effective way to reduce PTSD and distress, say the researchers. (Depression and Anxiety, April 2022)
|
Computer simulations show muscle weakness caused by peripheral artery disease
 Image: ©Getty Images/Bigpra (05/25/2022)
VA Nebraska-Western Iowa researchers used computer simulations to understand the walking problems of patients with peripheral artery disease. In peripheral artery disease, narrowed blood vessels reduce blood flow to the limbs. Patients with the condition have reduced muscle strength in the legs, which can cause walking problems. Researchers recorded gait and force metrics for 12 patients with the condition and 10 healthy patients. They then created computer simulations to study walking differences. Patients with peripheral artery disease walked slower than controls, with less hip extension. Several groups of leg muscles delivered inadequate force during stepping, compared with controls. The findings could be used to develop rehabilitation targeting specific muscles to improve walking in patients with peripheral artery disease, according to the researchers. (Journal of Biomechanics, April 2022)
|
Opioid prescribing decreased for Veterans in community living centers
 Photo: ©Getty Images/miodrag ignjatovic (05/25/2022)
Opioid prescribing decreased in recent years for Veterans with dementia in community living centers, found a study by VA Finger Lakes researchers and colleagues. The study included data from three time periods: 2012–2013, 2014–2015, and 2017–2018. More than 12,000 older Veterans living in community living centers were included. Opioid administration decreased after the publication of opioid safety guidelines for Veterans with dementia. Opioid prescribing was 26% lower in the second time period, and 34% lower in the third period. High-dose and long-term opioid use decreased more than 40% from the first time period. Prescriptions of both opioids and benzodiazepines (a dangerous combination) were 11% lower in the second period and 34% lower in the third period. Veterans with dementia and serious mental illness were less likely to be given opioids than those without mental illness. The results suggest that new guidelines reduced opioid use in community living centers, according to the researchers. More study is needed on how these opioid reductions affected health outcomes, they say. (Journal of the American Geriatrics Society, April 9, 2022)
|
Genetic links between severe COVID-19 and other diseases
 Image: ©Getty Images/Dr_Microbe (05/19/2022)
A VA Million Veteran Program study identified genetic links between COVID-19 severity and certain serious medical conditions. Researchers analyzed genetic and health record data on more than 650,000 Veterans who volunteered for MVP. They compared gene variations previously found to be linked to severe COVID-19 risk with gene variants connected to other conditions. The analysis showed that gene variants linked to severe COVID-19 are also linked to medical conditions known to be COVID-19 risk factors. The strongest links were found for venous embolism and thrombosis, as well as type 2 diabetes and ischemic heart disease. The study also showed genetic links between severe COVID-19 and neutropenia—low white blood cell count—in Veterans of African and Hispanic ancestry. This link was not seen in Veterans of European ancestry. Conversely, gene variants associated with severe COVID-19 were associated with reduced risk of immune-related conditions such as lupus and rheumatoid arthritis. The findings shed light on genetic risk for COVID-19 and could lead to paths for new treatments, say the researchers. (PLOS Genetics, April 28, 2022)
|
Dog ownership linked to physical exercise in older adults
 Photo: ©Getty Images/alexi_tm (05/19/2022)
Dog ownership is linked to positive physical health behavior in older adults, found a study by VA researchers. The study assessed multiple health outcomes in adults 65 and older. Dog owners were more likely than those without pets to walk for exercise. They also reported better subjective health. Cat owners did not differ from non-pet owners in self-reported health or walking. The researchers did not find a relationship between pet ownership and depression symptoms. White participants were more likely than Black participants to own pets. Sex, race, and geographic location did not affect the findings. The results show that dog ownership may lead to healthy behavior, but should not be viewed as a simple solution for depression, say the researchers. (International Journal of Environmental Research and Public Health, May 6, 2022)
|
Factors linked to suicidal behavior remission
 Photo for illustrative purposes only. ©Getty Images/LittleBee80 (05/19/2022)
VA researchers and colleagues identified three factors linked to remission from suicidal thoughts and actions in Veterans. Researchers analyzed a broad range of social, demographic, and health data from a large survey of U.S. Veterans. They found that purpose in life, dispositional gratitude, and conscientiousness were linked to remission from suicidal thoughts and behaviors. Dispositional gratitude refers to a tendency to appreciate the positive aspects of life. Conscientiousness means being goal-oriented and attentive to details. All three factors were linked to remission even after accounting for other risk and protective variables. These three elements could be targets for interventions to help prevent Veteran suicides, according to the researchers. (Journal of Psychiatric Research, May 2022)
|
Alcohol use disorder prevalent among Veterans
 Photo: ©Getty Images/kieferpix (05/04/2022)
Alcohol use disorder is prevalent among Veterans, according to a study by VA San Diego researchers. The study included more than 4,000 Veterans. About 41% of participants reported signs of alcohol use disorder in their lifetime, with 11% having the condition within the last year. Veterans with alcohol use disorder had higher rates of psychiatric disorders and suicidal behavior, compared with those without the disorder. Rates of these conditions increased with higher alcohol use disorder severity. Alcohol use disorder was linked to being younger, male, white, unmarried, retired, and having adverse childhood experiences and traumas. The results underscore the need for comprehensive alcohol use screening for Veterans, say the researchers. (Drug and Alcohol Dependence, Feb. 1, 2022)
|
Genetic testing could protect against adverse drug interactions
 Photo: ©Getty Images/Feverpitched (05/04/2022)
Genetic testing could help avoid adverse drug interactions for patients taking multiple medications, found a study by VA Puget Sound researchers. In a pilot study, researchers tested the genomes of 53 Veterans to predict how they would respond to specific medications. All participants were taking multiple medications for psychiatric conditions. Their health care providers were given the results of the genetic tests. For 83% of participants, providers changed their original medication plan based on the genetic results. Over 12 weeks of treatment, patients saw improvements in depression and mental health quality of life. Adverse drug effects were unchanged or improved over time with genetic testing, compared with original medication plans. The results show that genetic testing could benefit patients taking multiple medications, say the researchers. (Journal of Clinical Pharmacology, Jan. 24, 2022)
|
Post-concussive symptoms linked to suicide risk
 Photo: ©Getty Images/Pornpak Khunatorn (05/04/2022)
Concussions may increase suicide risk in Veterans by limiting social participation, found a VA study. Mild traumatic brain injury, also called concussion, has been linked to increased risk of suicide. Researchers assessed 145 Veterans with concussion history. They found that more severe post-concussive symptoms were linked to less participation in socially or culturally meaningful activities. Greater participation was associated with lower odds of suicidal thoughts. The researchers concluded that post-concussive symptoms may heighten the risk of suicidal thoughts by limiting social participation. The results suggest that occupational therapy could help prevent Veteran suicide by encouraging Veterans to engage in social activity, say the researchers. (American Journal of Occupational Therapy, May 1, 2022)
|
Pain in non-amputated arm common in Veterans with arm amputation
 Photo for illustrative purposes only. ©Getty Images/zoranm (04/27/2022)
Pain in the non-amputated arm is common in Veterans who have had an arm amputated, found a study by Providence VA researchers. The study surveyed nearly 800 Veterans with an upper-limb amputation—almost 600 participants were surveyed again one year later. About 73% had pain in the intact arm at baseline, 72% had pain one year later, and about 60% had persistent pain. Veterans who had conditions affecting the non-amputated arm, neck pain, and residual-limb pain had higher odds of having pain in the non-amputated arm. Black race, back pain, and older age were all associated with greater arm pain intensity. Women had lower pain intensity than men. Participants who used a cosmetic prosthesis also had less intense pain than those who used a body-powered prosthesis. The findings suggest that over-reliance on the non-amputated limb leads to pain in people with an upper-limb amputation, conclude the researchers. (Journal of Prosthetics and Orthotics, April 12, 2022)
|
Older and underweight Veterans at higher risk of death from COVID-19
 Photo: ©Getty Images/stefanamer (04/27/2022)
Older and underweight Veterans had a higher risk of death from COVID-19, in a study by Salt Lake City VA researchers and colleagues. Researchers studied data on more than 400,000 Veterans who tested positive for COVID-19 in 2020 and 2021. Those 65 and older and those who were underweight were more likely to require mechanical ventilation and die in the hospital, compared with younger Veterans and those with normal weight. Veterans 85 and older had an almost five times greater rate of death. Asian and American Indian/Alaska Native Veterans also had higher risk of ventilation and death compared to white Veterans. Black Veterans had a 31% higher risk than white Veterans of hospitalization, but did not have a higher risk of death. Hospitalization, ventilation, and death rates decreased for all groups over time. The results show that age and weight are important variables to consider in COVID-19 risk, say the researchers. (Annals of Epidemiology, April 21, 2022)
|
Transgender Veterans more likely to be prescribed opioids
 Photo: ©Getty Images/smartstock (04/27/2022)
Transgender Veterans had higher odds than cisgender Veterans of being prescribed opioids in VA, but not higher odds of high-risk opioid doses, found a study by VA Pittsburgh researchers. Researchers looked at data on nearly 10,000 transgender and more than 29,000 cisgender (someone who’s gender identity and sex assigned at birth are the same) Veterans receiving care in VA. They found that transgender Veterans had a 20% higher risk of being prescribed outpatient opioids. However, odds of high-risk prescribing were the same for transgender and cisgender Veterans. High-risk prescribing includes high doses, more than one opioid prescription, or prescriptions for both opioids and benzodiazepines. Overall, transgender Veterans had more than twice the risk of opioid poisoning compared with cisgender Veterans. But the risk was the same when only those prescribed opioids were analyzed. More research is needed on why opioid prescribing differs in these groups, say the researchers. (American Journal of Preventive Medicine, April 5, 2022)
|
Using genetic tests to assess disease risk
 Image: ©Getty Images/peterschreiber.media (04/22/2022)
VA Boston researchers and colleagues developed processes to assess patients for genetic risk for several diseases. A polygenic risk score summarizes a person’s gene variations to assess their genetic risk for a disease. While scientists have created many of these scores, assessing individual patients and then applying the findings clinically is more difficult. The researchers developed a process to analyze the genomes of more than 36,000 patients. They then compared the findings to polygenic risk scores for coronary artery disease, diabetes, atrial fibrillation, colorectal cancer, prostate cancer, and breast cancer. This method showed good accuracy for predicting disease risk. The team also developed a report to help clinicians interpret the results and share risk information with their patients. The study shows that individualized laboratory tests for genetic disease risk are feasible and could help improve patient health, say the researchers. (Nature Medicine, April 18, 2022)
|
Standing wheelchair performs well in testing
 Photo by Billie Slater (04/22/2022)
A manual standing wheelchair designed by Minneapolis VA researchers performed well and can improve users’ mobility. Standing wheelchairs allow users to raise from a seated to a standing position, enabling them to interact with people and objects at eye level. The study team previously designed a wheelchair that a user can propel manually in both the seated and standing position. They refined the design based on user feedback, including the weight and width of the chair. The new design met safety standards in stability testing. During a 100-meter test, study participants were able to move the wheelchair at speeds similar to those typical of wheelchair use in the home while both seated and standing. In the standing position, participants achieved speeds about three times faster than walking speeds seen with exoskeletons designed to help paralyzed users stand and walk. With some engineering changes, one participant was able to reach standing-configuration speeds similar to a nondisabled person when walking. This shows that the standing wheelchair could allow users to keep pace with family and friends, say the researchers. The standing wheelchair shows potential to improve users’ quality of life and health, they add. (Disability and Rehabilitation. Assistive Technology, Feb. 23, 2022)
|
Veterans’ health worsens over time after leaving military
 Photo: ©Getty Images/SDI Productions (04/22/2022)
Veterans may experience worsening health over time after leaving the military, according to a VA study. Researchers surveyed nearly 4,000 Veterans within three months of leaving the military. Each Veteran completed five additional surveys at six-month intervals. Most aspects of Veterans’ health and broader well-being worsened over time. The most noteworthy declines were in mental health and community involvement. Declines in good health and well-being were most notable in women Veterans. The findings highlight the need to increase health prevention and early intervention efforts as Veterans transition out of the military, according to the researchers. Women Veterans’ unique adjustment concerns especially need to be addressed, they say. (Social Science and Medicine, February 2022)
|
Military sexual trauma linked to multiple health problems
 Photo: ©Getty Images/guvendemir (04/13/2022)
Military sexual trauma is linked to elevated health burden, according to a VA study. Researchers surveyed more than 4,000 Veterans. They found that 44% of female and 4% of male Veterans had experienced military sexual trauma. Women with military sexual trauma histories had five-times greater odds of having PTSD, compared with other women. They were twice as likely to engage in mental health treatment. They also scored lower on measures of psychosocial functioning and had more physical health symptoms. Men with a military sexual trauma history had three-fold higher odds of suicidal thoughts. They were two- to three-times more likely to have PTSD, depression, and generalized anxiety disorder compared to men without a history of military sexual trauma. These male Veterans also had two-times greater odds of being disabled. The results underscore the importance of increasing outreach to both male and female Veterans with military sexual trauma history, say the researchers. (Journal of Affective Disorders, March 15, 2022)
|
Seizure drug may help treat posttraumatic irritability
 Photo: ©Getty Images/PeopleImages (04/13/2022)
A seizure drug may be an effective treatment for posttraumatic irritability, found a VA study. Irritability after traumatic brain injury can become a chronic problem that interferes with daily function. The study tested the effects of divalproex sodium, an epilepsy medication, on patients with posttraumatic irritability and a history of alcohol use disorder. Participants taking the drug showed significant, sustained reduction of irritability, compared with controls. Alcohol use did not change as a result of treatment. No adverse side-effects occurred. Larger clinical trials are needed to explore this potential new treatment, say the researchers. (Journal of Neuropsychiatry and Clinical Neuroscience, March 11, 2022)
|
Mindfulness program could lower opioid misuse
 Photo: ©Getty Images/FG Trade (04/13/2022)
A mindfulness program led to a reduction in opioid misuse and chronic pain improvements, according to a study led by a VA Salt Lake City researcher. Participants included 250 patients on long-term opioid therapy for chronic pain who were misusing opioid medication. Half received eight weeks of training focusing on mindfulness and savoring positive experiences. The other half attended supportive group psychotherapy. Nine months after treatment, 45% of the mindfulness group and 24% of the control group were no longer misusing opioids. The mindfulness group reported lower pain severity than the other group during the nine-month follow-up, as well as lower emotional distress and opioid craving. The mindfulness group also reduced their opioid dose more than the control group. The results suggest that mindfulness could be an effective approach to address opioid misuse, according to the researchers. (JAMA Internal Medicine, April 1, 2022)
|
Post-surgery opioid use increases opioid use disorder and overdose risk
 Photo: ©Getty Images/BackyardProduction (04/07/2022)
Patients who develop persistent post-surgery opioid use are at increased risk of opioid use disorder and overdose, according to a VA Maine study. Persistent opioid use is common after surgery. Researchers looked at data on more than 300,000 VA patients who had surgery. Patients were followed for multiple years. Those who developed persistent opioid use after surgery were at 88% higher risk of opioid use disorder, compared with those without persistent use. The risk of an opioid overdose was 78% higher in patients with persistent post-surgery use. Clinicians need to be aware of the risks when prescribing opioids after surgery, according to the researchers. (Annals of Surgery, Jan. 25, 2022)
|
VA depression screening leads to treatment, but improvements needed
 Photo: ©Getty Images/Lucky7trader (04/07/2022)
Most VA patients who screened positive for depression received treatment but fewer received timely follow-up, found a VA Greater Los Angeles study. VA mandates annual depression screening in primary care. Researchers studied data on more than 600,000 VA patients who were screened during a four-year period. About 8% screened positive for depression. Of those, 77% completed at least minimal depression treatment. However, only 32% met guidelines for timely follow-up after the positive screen. Younger patients, Black patients, and those with other psychiatric diagnoses were most likely to receive timely follow-up. The results show that VA’s universal depression screening has improved treatment, but improvements are still needed, say the researchers. (JAMA Network Open, March 1, 2022)
|
Behavioral health provider burnout
 Photo: ©Getty Images/FatCamera (04/07/2022)
VA Ann Arbor researchers and colleagues identified factors linked to burnout in VA behavioral health providers. They analyzed four years of employee survey responses from nearly 60,000 VA psychiatrists, psychologists, and social workers. Between 31% and 38% reported feeling burnout. Reasonable workload, having appropriate resources, supervisor support, and opportunities to improve skills were linked to lower burnout. Feeling that their work improved Veterans’ lives and that care provided was well-coordinated were also linked to lower burnout. Staffing vacancies, clerical work, and collateral duties that reduced availability for patient care were all associated with feelings of burnout. Workload was the strongest predictor of burnout. The findings highlight the importance of having necessary resources and support in behavioral health care, say the researchers. (Health Services Research, March 1, 2022)
|
COVID-19 increases diabetes risk
 Photo: ©Getty Images/towfiqu ahamed (03/31/2022)
COVID-19 increases the risk of developing diabetes, found a VA St. Louis study. Researchers studied data on more than 180,000 VA patients who had recovered from COVID-19. They compared these patients to over 4 million people who did not contract COVID-19 and over 4 million controls from before the pandemic. Those who had COVID-19 were at a 40% higher risk of being newly diagnosed with diabetes at least 30 days after infection, compared with controls. Odds of being prescribed medication for glycemic control were also increased. Diabetes risk was increased even in patients with mild COVID-19. More severe COVID-19 symptoms were linked to greater risk of developing diabetes. The results show that diabetes should be considered a facet of long COVID, and that strategies to address rising diabetes cases are needed, say the researchers. (Lancet Diabetes and Endocrinology, March 21, 2022)
|
Stem cells could speed up wound healing
 Photo: ©Getty Images/Motortion (03/31/2022)
Stem cells from fat could help speed up wound healing, according to a James A. Haley Veteran’s Hospital study. Chronic inflammation can often lead to problems with wound healing in the skin. Researchers isolated particles called exosomes from human fat stem cells. They showed that RNA strands in these exosomes are central to promoting wound repair. The researchers then simulated low-grade inflammation in lab-grown cells. They found that the exosomes from fat cells regulated inflammation pathways when introduced to the cells. The results show that exosomes harvested from fat cells could speed up healing in slow-healing skin wounds, such as those related to diabetes or obesity, say the researchers. (Biology, March 11, 2022)
|
Racial disparities in menopause management
 Photo: ©Getty Images/digitalskillet (03/31/2022)
Racial disparities may exist in menopause symptom reporting and treatment, according to a San Francisco VA study. Researchers studied electronic health record data for more than 200,000 women receiving care in VA. They found that Black women Veterans had lower odds of documented menopause symptoms, compared with white women Veterans. Black women also had lower estrogen use than white women. Black and Hispanic/Latina women were less likely than white women to be prescribed systemic hormone therapy to treat menopause symptoms. Hispanic/Latina women had higher odds than white women of a vaginal estrogen prescription. The findings show lower menopause symptom reporting and treatment in minority Veterans despite previous research that suggests higher menopause symptom burden in Black women. This suggests that important disparities in menopause care may exist, say the researchers. (Menopause, March 7, 2022)
|
COVID-19 vaccines largely effective over long-term
 Photo: ©Getty Images/Courtney Hale (03/23/2022)
COVID-19 vaccines are effective at preventing the disease long-term, according to a review by VA Iowa City researchers and colleagues. Most studies on vaccine effectiveness have looked at outcomes within three months after vaccination. The researchers conducted a literature search for studies of long-term vaccine efficacy. They found 16 studies that included nearly 18 million patients who received either the Pfizer, Moderna, AstraZeneca, or Janssen vaccines. At least five months after vaccination, average vaccine effectiveness was 84%. Average protection against COVID-19 hospitalization was 89%. Vaccine effectiveness during the delta variant wave was 61%. The findings show that COVID-19 vaccines convey protection for months after vaccination, say the researchers. More studies are needed on the effectiveness of a third dose, mixing different vaccines, and against newly emerging variants, they say. (Antimicrobial Stewardship & Healthcare Epidemiology, Feb. 14, 2022)
|
Strengths, weaknesses of housing-first homelessness program
 Photo: ©Getty Images/Punnarong (03/23/2022)
VA Greater Los Angeles researchers identified strengths and weaknesses of a housing-first program to combat Veteran homelessness. The Department of Housing and Urban Development-VA Supportive Housing (HUD-VASH) program prioritizes quickly finding permanent housing for homeless people without sobriety or mental health treatment prerequisites. Researchers surveyed Veterans and HUD-VASH providers on how well the program has been implemented. Overall, those surveyed believed that the program benefits Veterans and is sustainable. Weaknesses include client-to-staff ratio, frequency of client-provider contact, and time to housing. Factors such as housing scarcity and staff turnover affect the program’s sustainability. Staff also identified changes in leadership and unmet resource needs as challenges. The findings show that housing-first initiatives can help homeless Veterans, say the researchers, but improvements could be made. (Health Services Research, March 3, 2022)
|
Suicide rate increasing in American Indian and Alaska Native Veterans
 Photo: ©Getty Images/grandriver (03/23/2022)
Suicide is an increasing problem among American Indian and Alaska Native Veterans, according to a VA study. Researchers analyzed VA data on this group from between 2002 and 2014. They found that suicide rates more than doubled over the study period. The youngest age group (age 18–39) had the highest suicide rate. Firearms were the most frequently used means of suicide. The findings are similar to those seen in the general American Indian/Alaska Native population. The results show a compelling need to strengthen VA suicide prevention efforts for American Indian and Alaska Native Veterans, say the researchers. (Medical Care, April 1, 2022)
|
Small shifts in VA colon cancer screening during pandemic
 Photo: ©Getty Images/Zaharia_Bogdan (03/16/2022)
VA facilities achieved only limited success in efforts to switch from colonoscopy to fecal testing to improve colon cancer screening during the COVID-19 pandemic, according to a VA Ann Arbor study. A VA directive encourages the use of chemical fecal testing in place of colonoscopy for colon cancer screening to address screening backlogs. These backlogs were exacerbated during the pandemic. Researchers looked at data on screenings from both before and during the pandemic. They found a 9% decrease in colonoscopy screening in VA from the pre-COVID period to during the pandemic. The average monthly volume of fecal tests increased by 8% during this time. The results suggest poor system-wide uptake of the shift in screening type, say the researchers. More efforts are needed to increase access to cancer screening through stool-based testing, they say. (Gastroenterology, Feb. 24, 2022)
|
Stigma makes Veterans less likely to disclose suicidal behavior
 Photo: ©Getty Images/Srdjanns74 (03/16/2022)
Worry about stigma may stop Veterans from disclosing suicidal thoughts and behaviors, according to a study by VA researchers and colleagues. Past research has shown that stigma—feelings of shame or disapproval—is linked to less help-seeking for mental health issues. The researchers surveyed 500 participants, half of whom were Veterans. Greater feelings of self-stigma and anticipated stigma related to suicide were linked to a lower likelihood of disclosing suicidal thoughts and actions. This relationship was not seen in non-Veterans. Whether a Veteran used VA health care did not affect the fear of being stigmatized. The findings suggest that Veterans’ worries about suicide stigma may be grounded in past experiences in the military, say the researchers. Efforts are needed to protect against negative associations with talking about suicide in Veterans. (Psychiatry Research, March 2022)
|
Diabetes drug could help treat flu
 Photo: ©Getty Images/South_agency (03/16/2022)
The diabetes drug metformin may lower the risk of death from the flu, found a Columbia VA study. Metformin is a medication used to control high blood sugar. Researchers compared data on diabetic patients taking and not taking metformin, along with non-diabetic patients. All patients had been diagnosed with the flu. Flu patients prescribed metformin had lower rates of death than those not on metformin. There was no statistical difference between non-diabetic patients and diabetic patients not taking metformin. The results suggest that more research is warranted on metformin as a flu treatment, say the researchers. (Pathogens, Feb. 19, 2022)
|
Integrated mental health care may improve physical health
 Photo: ©Getty Images/LifestyleVisuals (03/09/2022)
Integrating mental health care into primary care clinics may improve patients’ physical health, found a study of VA patients. VA integrated mental health into all primary care clinics beginning in 2008. Researchers studied outcomes of nearly 830,000 patients seen at these clinics. About 6% of patients were seen by mental health specialists during their primary care visits. Diabetic patients seen at clinics with greater mental health care use showed better glycemic control. Patients diagnosed with hypertension had moderately lower odds of elevated blood pressure at clinics with more mental health use. The results suggest that integrating mental health care into primary settings can improve not only mental health, but physical health as well, say the researchers. (Journal of General Internal Medicine, Feb. 9, 2022)
|
Self-directed care program helps older Veterans live independently
 Photo: ©Getty Images/Inside Creative House (03/09/2022)
Older Veterans using a self-directed care program had fewer avoidable health care events, especially in rural settings, according to a VA study. The Veteran-Directed Care (VDC) program allows Veterans to pick for themselves the services and support they need to remain independent in the community, paid for by VA. Among other options, it allows participants to hire family members and neighbors as paid caregivers. Researchers studied data on more than 37,000 Veterans using VA-paid home and long-term care services. Both rural and urban Veterans using VDC were less likely to be admitted to a nursing home, compared with those using other care services. Rural VDC enrollees had significantly fewer acute care admissions and emergency room visits than those using other services. The results show that VDC has the potential to help older Veterans remain in the community. This is especially true in rural areas where health care options are more limited, say the researchers. (Journal of the American Geriatrics Society, Jan. 13, 2022)
|
Alcohol and drug use severity affect PTSD differently
 Photo: ©Getty Images/JurgaR (03/09/2022)
VA Southeast Louisiana Health Care System researchers identified mechanisms through which drug and alcohol use affect PTSD symptoms. PTSD and substance use disorders frequently occur together in Veterans. The researchers found that PTSD symptom severity was related to alcohol use severity through anxiety sensitivity, the fear of anxiety-related sensations. Drug use influenced PTSD severity through distress intolerance. Distress intolerance is the perceived inability to tolerate negative emotional states. Alcohol use was not linked to distress intolerance, and drug use was not linked to anxiety sensitivity. The findings suggest new ways to approach co-occurring PTSD and substance use disorders, according to the researchers. (Addictive Behaviors, March 2022)
|
Electronic appointment reminders improve VA wait times
 Photo: ©Getty Images/PeopleImages (03/01/2022)
Electronic appointment reminders improved wait times for VA patients, according to a study led by a VA Puget Sound researcher. The study included data on VA medical appointments across 130 VA medical centers made between January and October 2018. An interactive mobile text messaging system called VEText was rolled out across VA in that year. The data set included 39 million appointments from 5 million patients. Average wait time was shortened by 6.5 days after VEText adoption. However, VEText was also associated with an increase of 8.5 days waiting for patients who canceled or no-showed their appointments. The results suggest that electronic reminders can be a useful tool to decrease wait times, but challenges still exist, say the researchers. (JAMA Network Open, Feb. 1, 2022)
|
Horse riding could help Veterans with addiction
 Photo for illustrative purposes only. ©Getty Images/AleksandarGeorgiev (03/01/2022)
A horse-riding program has potential as a therapy for patients with addictive disorders, found a VA Salt Lake City study. Some evidence suggests that equine therapy can reduce anxiety and depression and enhance quality of life. Researchers conducted a pilot program of recreational trail rides with 18 Veterans with addictive disorders, such as drug or alcohol misuse. After the program, participants showed decreases in anxiety, negative emotions, and cravings. They also experienced increased positive emotions. The rides were carried out with minimal safety risks, although trail riding comes with some inherent dangers. The results show that recreational trail riding is a feasible complementary treatment for patients with addiction, say the researchers. (Complementary Therapies in Medicine, Feb. 3, 2022)
|
Gene strands linked to cognitive decline identified
 Photo: ©Getty Images/luismmolina (03/01/2022)
A team including an Atlanta VA researcher identified RNA strands that are involved in cognitive decline. The team studied the postmortem brain microRNA of more than 500 volunteers who had been diagnosed with dementia. MicroRNA are small, non-coding strands of genetic molecules that regulate gene expression. The researchers identified two specific strands that were particularly associated with cognitive trajectory. Together, the presence of these two genetic strands explained 13% of the variation in rate of cognitive decline seen in patients. Their effect on cognitive decline was independent of other neurodegeneration factors. The results will help scientists understand the molecular processes behind dementia and could lead to new treatments, according to the researchers. (Translational Psychiatry, Feb. 1, 2022)
|
COVID-19 increases mental health risks
 Image: ©Getty Images/Design Cells (02/24/2022)
COVID-19 increases the risk of multiple mental health conditions, according to a study by St. Louis VA researchers. The researchers examined data from more than 150,000 VA patients who had recovered from COVID-19. They compared the data to VA data on 5.8 million people who did not get COVID-19 during the pandemic era and 5.9 million controls from before the pandemic. Patients who contracted COVID-19 had a 60% higher risk of mental health disorders one year after recovering. This includes higher risk for anxiety, depression, stress disorders, opioid use, substance use disorders, and sleep conditions, as well as cognitive problems such as “brain fog.” Risk was increased even in patients who had less severe COVID-19 and were not admitted to the hospital. But this risk was highest in patients with more severe COVID-19. The results show that tackling mental health disorders among COVID-19 survivors should be a priority, say the researchers. (BMJ, Feb. 16, 2022)
|
Biomarkers may predict depression in pregnancy
 Photo: ©Getty Images/morrowlight (02/24/2022)
VA researchers and colleagues identified biomarkers that could help predict depression during pregnancy. Depression during and after pregnancy affects up to 20% of pregnant women. Researchers analyzed blood samples and symptoms in 114 pregnant women during each trimester and after pregnancy. They found that levels of two proteins, interleukin-1beta and interleukin-6, were linked to depression severity both during and after pregnancy. Measuring a combination of these proteins, called cytokines, and molecules linked to the amino acid tryptophan during the second trimester yielded a greater than 99% accurate prediction of third-trimester depression. The findings could help predict depression in pregnant women and may also lead to new treatment options, according to the researchers. (Translational Psychiatry, Jan. 26, 2022)
|
Automated wheelchair system to travel over curbs
 Photo courtesy of HERL (02/24/2022)
Engineers with the VA Pittsburgh’s Human Engineering Research Laboratories designed a system to help automated wheelchairs recognize and negotiate curbs. Common electric wheelchairs cannot safely travel over barriers such as curbs. Robotic wheelchairs are designed to overcome this obstacle. But they require proper alignment before passing curbs, which can be difficult for users with physical or sensory impairments. The researchers combined their existing mobility enhancement robot (MEBot) with a spatial-recognition algorithm called Polylidar3D. The system allows the MEBot wheelchair to automatically approach curbs correctly. It was able to successfully recognize curbs at 14 out of 15 starting positions and correctly determine the height and distance that the MEBot would need to travel. This allowed the wheelchair to climb curbs safely. The new system could improve accessibility and safety for automated wheelchair users, say the researchers. (Sensors, Nov. 24, 2021)
|
COVID-19 increases cardiovascular risk
 Photo: ©Getty Images/bymuratdeniz (02/15/2022)
COVID-19 increases the risk of cardiovascular complications, found a study by VA St. Louis researchers. The study included data on more than 150,000 VA patients who contracted COVID-19, comparing them with more than 5 million controls who did not have COVID-19 and more than 5 million pre-pandemic patients. Patients who had recovered from COVID-19 were significantly more likely to have heart and vascular disease a year after infection. Overall, COVID-19 patients had a 4% higher rate of heart disease. Compared with controls, they had a 72% higher risk of coronary artery disease, 63% higher risk of heart attack, and 52% higher risk of stroke. The risk was evident regardless of age, race, sex, or other cardiovascular risk factors. Even those who had mild COVID-19 had higher cardiovascular risk, although the risk increased with disease severity. The findings show that post-COVD-19 care needs to include cardiovascular health, say the researchers. (Nature Medicine, Feb. 7, 2022)
|
Problem drinking patterns after traumatic brain injury
 Photo: ©Getty Images/ZzzVuk (02/15/2022)
Trends in problematic drinking after a traumatic brain injury differ based on severity of injury, according to a VA study. Young service members and Veterans are at risk for problematic alcohol use. Research suggests that TBI may increase this risk. The study followed 265 service members and Veterans younger than 40 who had sustained a TBI for a period of five years. Those with moderate-to-severe TBI reported reduced alcohol consumption in the first two years after injury, followed by an increase in alcohol use. Those with mild TBI showed an opposite trend. Many had a period of increased alcohol use after injury, before declining to baseline levels of drinking. The difference between groups may be due to more severely injured patients receiving more advice to limit alcohol consumption as part of their TBI care. The results suggest that the period of two to five years after a TBI may be a critical window for efforts to lower alcohol use, say the researchers. (Journal of Head Trauma Rehabilitation, Feb. 1, 2022)
|
Veterans with and without mental illness equally likely to get COVID-19 vaccine
 Photo: ©Getty Images/Courtney Hale (02/15/2022)
VA patients with and without serious mental illness were equally likely to get a COVID-19 vaccine, found a Greater Los Angeles VA study. Researchers looked at data from nearly 5 million VA patients. They compared vaccine rates during the period of December 2020 to June 2021. About 48% of Veterans with a serious mental health diagnosis received a COVID-19 vaccine during the time period. For Veterans without serious mental illness, the vaccination rate was 46%. The results show that VA outreach has led to equitable COVID-19 vaccine distribution, according to the researchers. (Psychiatric Services, Jan. 18, 2022)
|
Digital app could improve loneliness and quality of life
 Photo: ©Getty Images/SeventyFour (02/10/2022)
A mental health therapy app improved loneliness and quality of life, found a study by VA Palo Alto researchers. The Meru Health Program is a therapist-supported digital program aimed at decreasing depression and anxiety. It focuses on mindfulness and cognitive behavioral interventions. Researchers looked at outcomes for 50 older participants using the app. Program use led to increases in mental health quality of life and decreases in loneliness. These changes were largely due to increases in mindfulness, according to study analysis. The results show that therapist-supported digital interventions can be a useful tool for improving mental health, say the researchers. (Frontiers in Public Health, Dec. 9, 2021)
|
Possible new biomarker for antidepressant effectiveness
 Photo: ©Getty Images/solarseven (02/10/2022)
A team including a Jesse Brown VA Medical Center researcher identified a biomarker that may help predict how well patients with depression respond to antidepressants. The researchers studied blood samples of 49 subjects with major depressive disorder and 59 healthy controls. Subjects with depression had significantly lower activity of an enzyme called adenylyl cyclase. The protein Gsα is known to activate adenylyl cyclase. However, in patients with depression this protein is often concentrated inside lipid rafts, structures within cell membranes made of lipid molecules. The researchers compared blood samples of patients with depression after six weeks of antidepressant treatment. They found that those who responded best to antidepressants had higher activation of the enzyme than those who did not respond to treatment. Antidepressants may aid in the movement of Gsα outside of lipid rafts, where they would be more likely to activate adenylyl cyclase, according to the researchers. The results could lead to a simple blood test for these molecules to predict how well antidepressants will work, they say. (Molecular Psychiatry, Jan. 5, 2022)
|
Brain structure changes linked to impairment after stroke
 Photo: ©Getty Images/Image Source (02/10/2022)
Reduced gray matter volume is connected to impairments after stroke, according to a study by a worldwide consortium including VA. A majority of stroke survivors experience sensorimotor impairments such as difficulty with fine motor skills. Structures in the gray matter are important in the regulation of sensorimotor movements. The researchers studied brain scans of more than 800 patients with stroke. In the early days of stroke recovery, sensorimotor problems were linked to lower volume of the thalamus on the same side of the brain as the stroke damage. In chronic stroke (symptoms lasting at least 180 days), a lower volume of the brain structures putamen and accumbens and larger lateral ventricle size were linked to worse sensorimotor behavior. The results show how changes in brain structure after stroke may cause motor and sensory problems, say the researchers. (Brian Communications, Oct. 27, 2021)
|
Gene variants increase COVID-19 kidney risk in patients with African ancestry
 Image: ©Getty Images/BlackJack3D (02/01/2022)
Veterans of African ancestry with specific gene variants were at heightened risk of acute kidney injury from COVID-19, found a VA Million Veteran Program study. COVID-19 can cause significant risk of acute kidney injury. Previous research has shown that people of African ancestry with two copies of specific variants of the APOL1 gene have increased rates of kidney disease. Researchers looked at genetic data on 990 MVP participants of African ancestry who were hospitalized with COVID-19. They found that patients with two copies of the high-risk APOL1 variants had higher odds of acute kidney disease, higher kidney disease severity, and death, compared with patients with one or none of the gene variants. This risk existed even in patients with prior normal kidney function. The findings suggest that genetic risk assessment could help predict kidney risk from COVID-19 in patients with African ancestry, say the researchers. (JAMA Internal Medicine, Jan. 28, 2022)
|
Depression may be linked to genetic cause of Alzheimer’s
 Image: ©Getty Images/Gio_tto (02/01/2022)
Depression may have a causal role in Alzheimer’s disease, according to a study by an Atlanta VA researcher and colleagues. Depression is known to be associated with increased Alzheimer’s risk. Researchers performed a genome-wide association study of more than 800,000 people to examine the genetic link between depression and Alzheimer’s. Data suggest that the two conditions have a shared genetic basis. Further, depression appears to add to the development of Alzheimer’s, but Alzheimer’s does not contribute to depression. The researchers identified 46 RNA molecules and seven proteins previously known to be linked to depression that also contribute to cognitive decline, Alzheimer’s pathologies, and Alzheimer’s diagnosis. Additionally, higher depression genetic risk was associated with faster memory decline. The results suggest genetic targets for possible future Alzheimer’s therapies, say the researchers. (Biological Psychiatry, Dec. 16, 2021)
|
Sound waves could help treat musculoskeletal injury
 Photo: ©Getty Images/ljubaphoto (02/01/2022)
Sustained acoustic medicine has potential as a treatment for musculoskeletal injury, according to a VA review. Sustained acoustic medicine uses high-frequency ultrasound waves to stimulate circulation and cell growth. James A. Haley VA Hospital researchers performed a literature search of studies on this technique. They found 13 clinical studies on the topic. Patients in the studies were being treated for neck and back pain and injury, knee pain from osteoarthritis, or soft tissue injury. Acoustic treatment was shown to improve patient function and reduce pain. It was linked to heating that aided tissue recovery. Because it is non-invasive and non-narcotic, sustained acoustic medicine could be a good treatment option for musculoskeletal pain when patients do not respond to physical therapy, say the researchers. (BMC Sports Science, Medicine & Rehabilitation, Dec. 18, 2021)
|
Telehealth may be best method to deliver PTSD therapy
 Photo: ©Getty Images/insta_photos (01/25/2022)
Telehealth therapy is an efficient and effective way to treat PTSD, according to a study by South Texas VA researchers and colleagues. Active-duty service members and Veterans with PTSD underwent 12 sessions of cognitive processing therapy, a psychotherapy. Therapy was delivered one of three ways: face-to-face with the therapist in-office; through a computer video link; or in the patient’s home, with the therapist traveling to the home. All three methods resulted in significant PTSD symptom reductions. In-home and telehealth symptom reductions were about twice as large as those for in-office treatment. In-home treatment had the lowest dropout rate, but the differences were not statistically significant. While in-home treatment led to the strongest PTSD improvements and lowest dropout, it was also the least accepted treatment by patients. In-home treatment also required double the amount of therapist time and had unexpected complications for both patients and therapists. The results provide strong support for the use of telehealth for PTSD treatment, say the researchers. (BMC Psychiatry, Jan. 17, 2022)
|
Moral injury increases Veterans’ suicide risk
 Photo: ©Getty Images/zabelin (01/25/2022)
Moral injury during military service increases suicide risk in both men and women, according to a VA study. Moral injury is defined as perpetrating, failing to prevent, or bearing witness to acts that go against deeply held moral beliefs. Researchers surveyed more than 14,000 Veterans. They found that men who experienced moral injury were 50% more likely to attempt suicide during their service and twice as likely to do so after leaving the military, compared with those without moral injury. Men who felt betrayed were nearly twice as likely than those without these feelings to attempt suicide during service, but no more likely after service. Women who experienced betrayal were over 50% more likely to attempt suicide both during and after service. Perpetrating a morally injurious act did not increase the suicide risk of women Veterans. The findings indicate that moral injury assessment should take gender difference into account, say the researchers. (Psychological Medicine, Jan. 17, 2022)
|
Oxytocin may improve opioid use disorder treatment adherence
 Photo: ©Getty Images/Malikov Aleksandr (01/25/2022)
Using oxytocin nasal spray may improve patients’ adherence to opioid treatment programs, found a study by VA researchers. Use of stimulants such as cocaine or methamphetamine in people with opioid use disorder (OUD) has increased drastically in recent years. Stimulant users have lower treatment retention and poorer outcomes than those with OUD only. In the study, Veterans receiving medication treatment for OUD (such as methadone) also received twice-daily intranasal oxytocin for six weeks. Oxytocin is a hormone linked to social bonding. Some research suggests that it could have anti-addiction effects. Oxytocin did not decrease patients’ stimulant use or cravings. However, those receiving oxytocin attended significantly more daily opioid medication visits. The results suggest that oxytocin could improve engagement and social connection, leading to better adherence to OUD treatment, according to the researchers. (Frontiers in Psychiatry, Jan. 17, 2022)
|
Study identifies gene variant that may protect against severe COVID-19
 Image: ©Getty Images/Gilnature (01/19/2022)
An international study using VA Million Veteran Program data identified a specific gene variant that may protect against severe COVID-19 infection. The team, including a VA Boston researcher, studied the genome of nearly 3,000 patients of African ancestry with COVID-19 and more than 130,000 controls of African ancestry. They found that individuals with a specific variant on the gene OAS1 had a decreased chance of developing severe COVID-19. Previous studies of people of European ancestry identified the region on the genome containing OAS1 as related to COVID-19 risk. By examining this region in those with African ancestry, the researchers were able both to show that people of different ancestry shared this protection and to home in on the specific gene variant. People with this gene variant produce a longer form of a specific protein, which is more effective at breaking down the virus that causes COVID-19 than other forms of the protein. The finding could help develop new drugs against COVID-19, according to the researchers. The study also shows the importance of including ethnically diverse populations in genetic studies, they say. (Nature Genetics, Jan. 13, 2022)
|
VA patients may receive better diabetes care than non-VA patients
 Photo: ©Getty Images/evgenyb (01/19/2022)
Diabetic patients receiving VA care had better blood pressure and cholesterol management than those receiving non-VA care, found a study by VA researchers and colleagues. Of more than 5,000 patients, VA and non-VA patients had similar diabetes outcomes. However, VA patients had more diabetes risk factors, including high blood pressure and cholesterol, older age, and cardiovascular disease. VA patients were more likely to be on blood pressure- and cholesterol-lowering medications, leading to better cholesterol numbers than those seen in non-VA patients. The results suggest that VA patients received better diabetes care despite having more diabetes complications, say the researchers. (Diabetes Research and Clinical Practice, Dec. 28, 2021)
|
Women Veterans less likely than men to be prescribed statins
 Photo: ©Getty Images/rogerashford (01/19/2022)
Women are less likely than men to receive statin therapy for cardiovascular care, according to a Ralph H. Johnson VA Medical Center study. Statins, drugs that lower cholesterol, are often prescribed to patients with cardiovascular disease and diabetes. Researchers looked at data on more than 700,000 VA patients with diabetes. They found that women Veterans had 14% lower odds of being prescribed statins, compared with men. Lower access to health care and higher mental health diagnoses seem to explain this disparity. Women were 10% less likely than men to be on high-intensity statins. After the researchers adjusted for health care access and mental health burden, women actually had higher odds of high-intensity statin use. The study highlights a persistent health disparity between men and women Veterans, say the researchers. (Women’s Health Issues, Dec. 20, 2021)
|
Group cohesion an important part of suicide prevention group therapy
 Photo for illustrative purposes only. ©Getty Images/SDI Productions (01/12/2022)
Establishing group cohesion is an important part of group therapy for Veteran suicide prevention, according to a study by Robley Rex VA Medical Center researchers. They performed a three-year follow-up of Veterans who received group therapy after discharge from inpatient psychiatric care following a suicidal crisis. No suicides occurred during the study period. Higher group cohesion was linked to a lower likelihood of psychiatric hospitalization and higher engagement in mental health services. Group cohesion refers to forming a collaborative, accepting relationship with the therapy group. Factors that led to group cohesion included shared experiences and having similar service backgrounds, as well as building intimacy and trust. The results show that group therapy could be a useful long-term treatment for suicidal behavior, say the researchers. (Psychological Services, Dec. 30, 2021)
|
Less racial disparity in VA than non-VA care for bladder cancer
 Photo for illustrative purposes only. ©Getty Images/SeventyFour (01/12/2022)
Lower racial disparities in bladder cancer outcomes were seen in VA versus outside care, in a study by VA San Diego researchers. African American patients with bladder cancer tend to have worse outcomes than white patients, likely due to difference in health care access. The study included more than 36,000 VA patients and more than 120,000 non-VA patients with bladder cancer. African Americans were more likely than Whites to have muscle-invasive disease (a more serious form of bladder cancer) and cancer metastasis, when cancer spreads to other parts of the body, in both groups. But this racial difference was smaller in VA patients. In non-VA patients, African Americans were more likely than Whites to die from bladder cancer or other causes. Mortality rates between races were similar in VA patients. The findings show that receiving care in an equal-access system such as VA lowers cancer care disparities, according to the researchers. (Journal of the National Cancer Institute, Dec. 16, 2021)
|
Lower risk of death from surgery in VA hospitals than outside facilities
 Photo: ©Getty Images/Morsa Images (01/12/2022)
Patients who have surgery at VA facilities had a lower risk of death than those receiving non-VA surgery, found a VA study. Researchers looked at data on nearly 4 million surgeries performed between 2015 and 2018. Surgeries from eight different non-cardiac specialties were examined. Compared with private sector care, VA care was associated with a lower risk of death during surgery and recovery. VA surgeries also had lower failure to rescue, defined as inability to prevent a patient’s deterioration and death after a complication arises. The results suggest that VA hospitals may be better equipped to care for the unique surgery needs of Veterans, say the researchers. Veterans are often more frail and have more medical conditions than the general population. (JAMA Surgery, Dec. 29, 2021)
|
Potential new treatment for cocaine use disorder
 Photo: ©Getty Images/GeniusKp (12/27/2021)
A team including a Providence VA researcher identified a potential new treatment for cocaine use disorder. Researchers studied gene expression in the brain tissue of people with cocaine use disorder who died from cocaine-related causes. They identified several gene expression patterns associated with the disorder. Ibrutinib, a drug used to treat certain cancers, appears to interact with the biological pathways associated with cocaine use disorder. Using a fruit fly model, the researchers found that ibrutinib reduced cocaine-induced startle response and seizures. The findings suggest that ibrutinib could be a useful treatment for cocaine use disorder, say the researchers. (Translational Psychiatry, Dec. 8, 2021)
|
Crowded psychiatric units may increase suicide risk
 Photo: ©Getty Images/sturti (12/27/2021)
Inpatient psychiatric unit overcrowding may increase suicide risk, found a study of VA patients. Researchers looked at data from 111 VA medical centers with psychiatric units from 2011 to 2016, a period in which Veteran suicides increased. They found that inpatient psychiatric unit occupancy above 95% was associated with a 10% increase in Veteran suicide risk in the region. The total number of beds in a psychiatric unit did not affect suicide risk. The researchers suggest that mental health care providers may make different decisions on whether to admit patients for suicidal thoughts or other mental health diagnoses based on psychiatric bed availability. Ensuring psychiatric units have enough beds could be an important part of preventing Veteran suicide, they say. (BMJ Quality & Safety, Aug. 16, 2021)
|
Phone app may help treat insomnia
 Photo: ©Getty Images/PeopleImages (12/27/2021)
A mobile app can help treat insomnia in Veterans, found a VA Bedford study. CBT-i Coach is a smartphone program designed to deliver cognitive behavioral therapy to treat insomnia. Cognitive behavioral therapy is psychological treatment focused on changing patterns of thinking related to stress and trauma. Veterans with chronic insomnia using the app reported significant improvements in sleep quality and insomnia symptoms. Benefits were similar in those with and without PTSD or sleep apnea. Adding a physical activity regimen to the app treatment did not affect outcomes. The results show that app-directed self-management can be a useful tool for Veterans with insomnia. (JMIR Formative Research, Dec. 9, 2021)
|
Risk factors for Veteran suicide
 Photo for illustrative purposes only. ©Getty Images/Nes (12/27/2021)
A seven-year study by VA researchers identified risk factors for suicide in Veterans. The researchers followed more than 2,000 Veterans for seven years to see how their baseline characteristics affected suicide risk. The strongest suicide risk factors were loneliness, low dispositional gratitude (the ability to appreciate positive aspects of life), thoughts of self-harm, and new traumas. Having more than one risk factor increased suicide risk. Veterans with all four risk factors had a 55% higher risk of a suicide attempt. The results suggest that suicide prediction models should consider how risk factors combine, say the researchers. (Suicide and Life-Threatening Behavior, Dec. 6, 2021)
|
COVID-19 antibodies decline after six months in nursing home residents
 Photo: ©Getty Images/Geber86 (12/27/2021)
Antibodies from the COVID-19 vaccine declined significantly in nursing home residents six months after vaccination, found a Cleveland VA study. Researchers tested the blood of 130 nursing home residents and 95 health care workers two weeks and six months after they received the Pfizer mRNA vaccine. At two weeks, nursing home residents had only one-quarter of the antibodies as health care workers. The difference was likely due to age and health-related risk factors. All subjects who did not contract COVID-19 after vaccination had drastically lower antibody levels after six months. Of nursing home residents who never caught COVID-19, 69% had antibody levels below the limit of detection after six months. Residents with COVID-19 infection before vaccination had slightly higher antibody levels, but antibody levels still dropped by at least 81%. The results highlight the need for vaccine boosters, especially in older populations, say the researchers. (Clinical Infectious Diseases, Nov. 19, 2021)
|
Drug may help prevent cardiovascular complications of kidney disease
 Photo: ©Getty Images/PeopleImages (12/27/2021)
The drug finerenone may improve cardiovascular outcomes in patients with diabetes and chronic kidney disease, found a study that included a Richard L. Roudebush VA Medical Center researcher. Finerenone (sold as Kerendia) has been shown to improve outcomes in patients with advanced kidney disease. But its effects on those with less advanced kidney disease are unknown. More than 7,000 patients with chronic kidney disease and type 2 diabetes were given either finerenone or placebo. Researchers followed patients for more than three years. The finerenone group had lower rates of death from cardiovascular causes, heart attack, stroke, and hospitalization for heart failure, compared with the placebo group. Those taking finerenone also had lower frequency of kidney failure, decreased kidney function, and kidney-related death. The results suggest that finerenone may be an attractive therapeutic option to prevent cardiovascular complications of kidney disease, say the researchers. (New England Journal of Medicine, Dec. 9, 2021)
|
Psychotherapy an effective treatment for anger
 Photo: ©Getty Images/Andranik Hakobyan (12/15/2021)
The psychotherapy cognitive behavioral intervention (CBI) is an effective treatment for anger problems in Veterans, found a VA study. Problems with anger and aggression are common in post-9/11 Veterans. Researchers compared the effectiveness of CBI versus supportive intervention for anger in 92 Veterans. CBI focuses on recognizing and changing how a patient thinks and reacts to anger and traumatic thoughts. Supportive intervention focuses on support, hope, and motivation. Patients receiving CBI has significantly more improvement in anger severity, social and interpersonal functioning, and quality of life. The treatment was effective regardless of whether the patient had PTSD. The results show that CBI can be an effective treatment for post-deployment anger for patients both with and without PTSD, say the researchers. (Depression and Anxiety, Dec. 8, 2021)
|
Genetic mutations linked to esophageal cancer identified in African American patients
 Photo for illustrative purposes only. ©Getty Images/FG Trade (12/15/2021)
Washington, DC VA researchers identified genome mutations that could explain the aggressiveness of esophageal cancer in African Americans. Esophageal cancer—cancer of the tube that runs from the throat to the stomach—has a low survival rate because of a lack of diagnostic markers for early detection. In the United States, 75% of patients diagnosed with esophageal squamous cell carcinoma are of African descent. Researchers analyzed the genomes of 10 tumors from African American patients, compared with health control tissue. This was the first such genetic study in African American patients. They identified several gene mutations that could help explain why esophageal cancer is so aggressive in this population. The findings could lead to new diagnostic and treatment techniques, according to the researchers. (Scientific Reports, July 20, 2021)
|
Lithium can stabilize circadian rhythm in bipolar disorder
 Photo: ©Getty Images/yanyong (12/15/2021)
Lithium treatment is associated with reduced circadian rhythm disruption in patients with bipolar disorder, found a study by VA San Diego researchers and colleagues. Bipolar disorder often involves depression and disrupted circadian rhythms. A circadian rhythm is a natural, internal process that regulates the sleep-wake cycle and repeats about every 24 hours. Lithium is an effective treatment for bipolar disorder, but only 30% to 40% of patients respond. It is unclear how important lithium’s effect on circadian rhythm is to the treatment’s effectiveness. Researchers measured sleep patterns in 386 patients with bipolar disorder. They found that patients who had never taken lithium had the most circadian disruption. Patients who responded to 12 weeks of lithium treatment showed significant improvements in depression symptoms that disturb sleep patterns. The results suggest that stabilizing circadian rhythms may be an important feature of lithium treatment for bipolar disorder, say the researchers. (Bipolar Disorder, Nov. 26, 2021)
|
Diabetes drug metformin may lower liver cancer risk in diabetic patients
 Image: ©Getty Images/magicmine (12/03/2021)
Metformin use and glycemic control were linked to reduced risk of liver cancer in patients with diabetes and nonalcoholic fatty liver disease, found a Michael E. DeBakey VA Medical Center study. Nonalcoholic fatty liver disease patients who also have diabetes have a high risk of developing liver cancer. Researchers looked at data from nearly 86,000 VA patients with both conditions. Use of the diabetes drug metformin was linked to a 20% lower risk of liver disease compared to patients not taking the drug. Adequate control of blood sugar levels was linked to a 31% lower risk of cancer. Taking insulin alone did not affect cancer risk. Insulin combined with other oral medications was linked with a 1.6-fold higher risk of liver cancer. The results support the idea that metformin may help prevent liver cancer in these patients, say the researchers. (Hepatology, Nov. 15, 2021)
|
Combination antibiotics may effectively treat drug-resistant bacteria
 Photo: ©Getty Images/Ridofranz (12/03/2021)
Combination antibiotics may be more effective than older medication at treating antibiotic-resistant infections, according to a review by Hines VA researchers and colleagues. Antibiotic-resistant bacteria, such as carbapenem-resistant Enterobacterales and Pseudomonas aeruginosa, are serious health care concerns. Combination antibiotics pair older drugs with a drug called beta-lactamase inhibitor. The researchers reviewed scientific studies to see whether these new antibiotics are more effective than older drugs at treating the two infections. They found that combination antibiotics produced similar clinical results as older drugs. The new drugs appear to be more effective at controlling bacteria levels. The results support recommendations that combination antibiotics be used to overcome antibiotic resistance, say the researchers. (Antimicrobial Stewardship & Healthcare Epidemiology, Nov. 25, 2021)
|
Asthma drug may reduce lung cancer risk
 Photo: ©Getty Images/mustafagull (12/03/2021)
Asthma medication may reduce the risk of lung cancer, found a study by Columbia VA researchers. Drugs called leukotriene inhibitors are used to treat asthma. Some research suggest that they may also suppress tumor growth. Researchers studied data on more than 550,000 VA patients with asthma. Patients taking a leukotriene inhibitor had a 22% reduced risk of lung cancer, compared with patients not on the drug. The researchers caution that other factors may be at play because treatment was not randomized. The findings suggest that leukotriene inhibitors have potential as lung cancer prevention, say the researchers. (Pulmonary Pharmacology and Therapeutics, Oct. 15, 2021)
|
Lithium does not appear to improve suicide risk
 Photo: ©Getty Images/Chris Marshall (11/24/2021)
Adding lithium to medication regimens does not help prevent suicide-related events in patients with mood disorders, found a VA study. Prior studies have suggested that lithium may prevent suicide in patients with bipolar disorder or depression. Researchers added lithium to the treatment of VA patients with bipolar disorder or depression who had survived a recent suicide-related event, such as a suicide attempt or a hospital admission to prevent suicide. The trial was stopped for futility after 519 Veterans were enrolled. No difference between lithium and placebo treatment was found. Both the lithium and placebo groups had similar rates of suicidal behavior. The findings suggest that adding lithium has no effect on suicidal behavior for patients with mood disorders, say the researchers. (JAMA Psychiatry, Nov. 17, 2021)
|
Telemedicine could help reduce emergency department overcrowding
 Photo: ©Getty Images/Marje (11/24/2021)
Tele-urgent care could safely decrease emergency department overcrowding, according to a San Francisco VA study. Emergency department use for non-emergency issues often leads to overcrowding and decreased quality of care. Researchers tested a telehealth program for urgent care to address this issue. Out of 2,510 patients who used tele-urgent care, 21% were referred to in-person emergency care. Among those not referred to in-person care, 11% ended up visiting an emergency department within 72 hours. Only one in five in this group required hospitalization. The results show that a virtual platform may offer an effective and safe way to assess patients and decrease emergency department burden, say the researchers. (Journal of Telemedicine and Telecare, June 21, 2021)
|
Smartphone app aims to help prevent Veteran suicide
 Photo: ©Getty Images/PeopleImages (11/24/2021)
Researchers from the Providence VA developed a smartphone app to help prevent suicide. The Mobile Application for the Prevention of Suicide (MAPS) uses assessment in the moment to identify suicide risk and deliver real-time treatment strategies. The app is personalized to each patient. Eight Veterans hospitalized for suicidal behavior tried MAPS for two weeks. They reported high levels of satisfaction. All eight Veterans opted to continue using the app after the trial period ended. MAPS could be a useful addition to treatment and may help better track suicide risk and provide assistance for high-risk Veterans, according to the researchers. (Military Psychology, Oct. 28, 2021)
|
Daily fasting could improve metabolic health, suggests mouse study
 Photo: ©Getty Images/dra_schwartz (11/17/2021)
Fasting is an important aspect of a calorie-restricted diet, suggests a study by William S. Middleton Memorial Veterans Hospital researchers. Calorie restriction has been shown to promote healthy aging in mouse models. But in such models, feeding usually happens once per day, altering normal feeding behavior. Researchers studied multiple feeding patterns in mice to see how periods of fasting affect calorie restriction benefits. They found that prolonged fasting is necessary for key metabolic and molecular benefits of calorie restriction to take effect. A calorie-restricted diet improved glucose tolerance, body composition, and age-related frailty, but only in mice that fasted for extended period between meals. The results suggest that when a person eats, not just how much they eat, is important to health and diet, according to the researchers. Daily prolonged fasting could have real benefits for metabolic and aging health in humans, they say. (Nature Metabolism, October 2021)
|
Homelessness, justice involvement linked to mental health difficulties
 Photo: ©Getty Images/LordHenriVoton (11/17/2021)
Homelessness and justice involvement are linked to greater mental health difficulties, according to a VA Rocky Mountain MIRECC study. Researchers looked at data from a 2018 survey of more than 15,000 post-9/11 Veterans. They found that homelessness and a history of involvement with the criminal justice system were both linked to more severe PTSD, depression, and substance use symptoms, compared with other Veterans. Those who experienced homelessness or justice involvement also had increased rates of suicidal thoughts and attempts. Veterans with a history of both homelessness and justice involvement had the most severe mental health symptoms and suicide risk of the study group. The findings show that increased access to mental health services is needed in these Veteran populations, say the researchers. (Journal of Psychiatric Research, Nov. 3, 2021)
|
Solar activity may be linked to high blood pressure in elderly men
 Image: ©Getty Images/dzika_mrowka (11/17/2021)
Sunspots may be linked to higher blood pressure in older men, found a study including VA Boston researchers. The researchers studied blood pressure readings for 675 elderly men between 2000 and 2017. Participants were born between 1884 and 1945. They found that periods with high magnetic field activity from the sun corresponded with higher diastolic and systolic blood pressure patterns. The pattern was most evident when the number of sunspots and disturbance to Earth’s magnetic field were high 16 days before blood pressure reading. The link between solar radiation and blood pressure was independent of pollution or ambient radioactivity levels. Previous research has shown that changes in magnetic field linked to sunspots and solar wind can affect autonomic nervous system activity. The results could have implications for long-term management of blood pressure, and also may help scientists interpret data from long studies, according to the researchers. (Journal of the American Heart Association, Nov. 2, 2021)
|
COVID-19 vaccine effectiveness wanes, but remains high against death
 Photo: ©Getty Images/Inside Creative House (11/10/2021)
Vaccine protection against COVID-19 declined during 2021, but protection against death after infection remained high, according to a study by VA San Francisco researchers. The study looked at COVID-19 infection rates and deaths for more than 780,000 VA patients between February and October 2021. Effectiveness against infection for the three vaccines being given in the United States—created by Pfizer, Moderna, and Janssen—fell from an average of 88% to 48% as the Delta variant of the virus emerged. Although breakthrough infections increased, the vaccines proved to be highly protective against death from COVID-19. Protection against death from COVID-19 remained above 73% for all three vaccines in patients younger than 65, and above 70% for older patients. The findings support efforts to increase vaccination, booster campaigns, and additional layers of protection against infection, say the researchers. (Science, Nov. 4, 2021)
|
E-cigarettes may increase inflammation, disease risk
 Photo: ©Getty Images/danchooalex (11/10/2021)
E-cigarettes may increase inflammation and weaken immune response, according to a VA San Diego study. Researchers measured the levels of several biomarkers in the saliva, sputum, and blood of e-cigarette users and non-smoking controls. E-cigarette smokers had higher levels of proteins that indicate inflammation. Smokers also had lower levels of proteins that signal the immune response to help fight off infections. The immune response was also blunted in smokers when challenged by a bacteria. This suggests a decreased ability to respond to infection. The findings raise concerns that smoking e-cigarettes may make people more vulnerable to infectious disease, say the researchers. (American Journal of Physiology, Oct. 27, 2021)
|
PTSD medication disparities between rural and urban VA patients mostly eliminated
 Photo: ©Getty Images/SDI Productions (11/10/2021)
Disparities in PTSD treatment between rural and urban VA patients have improved in the last decade, found an Iowa City VA study. Researchers looked at VA prescribing data from 2009 and 2019. They found that recommended PTSD medications were prescribed significantly less often in rural clinics than in larger medical centers in 2009. By 2019, recommended prescribing was about equal in rural and urban settings. In 2009, prescribing of medications not recommended for PTSD patients was higher among rural than urban residents. The rates were largely equal by 2019. The results show that rural discrepancies in PTSD prescribing in VA had largely been corrected by 2019, according to the researchers. (Journal of Rural Health, Nov. 9, 2021)
|
Tau protein linked to traumatic brain injury, processing problems
 Image: ©Getty Images/selvanegra (11/02/2021)
High levels of the protein tau are linked with a history of traumatic brain injury and reduced processing speed in Vietnam-era Veterans, found a study by VA San Diego researchers. The team checked the levels of several biomarkers in the cerebrospinal fluid of 102 Veterans, half of whom had history of TBI. The TBI group had significantly higher levels of both p-tau and t-tau, two forms of a protein often found in the brain and spinal cord. Researchers did not find differences in levels of amyloid beta, a peptide associated with Alzheimer’s disease. Those with TBI history and high tau levels had reduced performance on a measure of cognitive processing. The findings suggest that tau accumulation may be a mechanism of dementia risk for Veterans with TBI, according to the researchers. (Alzheimer’s and Dementia, Oct. 14, 2021)
|
Pregnancy-related anxiety linked to postpartum depression
 Photo: ©Getty Images/AsiaVision (11/02/2021)
Pregnancy-related anxiety was linked to postpartum depression and parent-child bonding difficulties, in a study of pregnant Veterans. Twenty-eight pregnant Veterans completed questionnaires during and after pregnancy. Results showed that pregnancy-related anxiety was a stronger predictor of postpartum depression than depression during pregnancy. Postpartum depression was in turn associated with parenting stress. More depressed mothers were more likely to have greater difficulties bonding with their child and experienced more feelings of rejection, anger, anxiety, and stress. The results suggest that treating anxiety during pregnancy could help prevent postpartum depression and subsequent parenting difficulties, say the researchers. (Maternal Child Health Journal, Oct. 9, 2021)
|
Transcranial magnetic stimulation can improve depression, PTSD
 Image: ©Getty Images/image_jungle (11/02/2021)
Transcranial magnetic stimulation (TMS) was shown to reduce depression and PTSD symptoms, in the largest study to date of the treatment in Veterans. TMS noninvasively uses magnetic fields to affect the electrical signals in the brain. Researchers studied its effectiveness in 770 Veterans with major depressive disorder. Of those, 68% also had PTSD. TMS led to clinically meaningful symptom reductions for both conditions. Of patients who received an adequate dose of TMS, 41% saw depression symptom improvements, with a remission rate of 20%. For patients with PTSD, 65% had meaningful symptom reduction, and 46% no longer met the criteria for PTSD. The results support the effectiveness and safety of TMS for treating both depression and PTSD, say the researchers. (Journal of Affective Disorders, Oct. 20, 2021)
|
Low-value prostate cancer screening common in VA
 Photo: ©Getty Images/BeholdingEye (10/26/2021)
Low-value cancer screenings in VA were low for some cancers, but high for prostate cancer, found a study by VA Puget Sound researchers. Clinical practice guidelines recommend stopping cancer screenings when risks exceed benefits. Researchers looked at data on almost 6 million VA patients. For men of average risk, 19% underwent prostate cancer screening and 5% underwent colorectal cancer screening. For women of average risk, 5% underwent breast cancer screening and 14% underwent cervical cancer screening. Low-value screening was defined as screening outside of recommended age ranges or mortality risks. It was rare for breast, cervical, and prostate cancers. However, more than one-third of prostate cancer screens were low-value. Patient race and ethnicity, sociodemographic factors, and health burdens were linked to the likelihood of receiving low-value tests. Individualized recommendations for cancer screenings could help limit low-value screenings, say the researchers. (JAMA Network Open, Oct. 1, 2021)
|
Mild traumatic brain injury linked to prolonged health problems
 Photo for illustrative purposes only. ©Getty Images/Ridofranz (10/26/2021)
Deployment-related mild traumatic brain injury was associated with multiple persistent post-concussive symptoms, in a VA study. Researchers interviewed 613 Veterans and service members who served in Afghanistan and Iraq. They found that mild TBI was linked to headaches, sleep disturbance, and difficulty making decisions an average of 10 years after injury. Deployment-related TBI was also associated with nausea/upset stomach and numbness or tingling. These symptoms were seen in deployment-related TBI but not normally in TBI patients. The results show that mild TBIs sustained during deployment have enduring negative health effects, according to the researchers. (Brain Injury, Sept. 20, 2021)
|
Statin use may increase diabetes progression
 Photo: ©Getty Images/vitapix (10/26/2021)
Statin use is linked to worsening diabetes progression, according to a study led by a VA North Texas researcher. Statins are drugs intended to lower cholesterol. Researchers compared data on over 80,000 VA patients with diabetes who took statins and a matched group not on statins. They found that diabetes worsened in 56% of patients taking statins, compared with 48% of those not on the drug. Patients taking statins were more likely to have begun insulin treatment, have high blood sugar, have diabetes complications, and take an increased number of prescriptions. Results show that the risks and benefits of statin use need to be carefully weighed in diabetes patients, say the researchers. (JAMA Internal Medicine, Oct. 4, 2021)
|
Biological pathways of suicide risk identified
 Image: ©Getty Images/kirstypargeter (10/21/2021)
VA Million Veteran Program researchers identified several biological factors related to suicide risk. Researchers conducted a genome-wide association study comparing Veterans with a history of suicide attempts with those without suicidal behavior. They found 30 biologic pathways associated with an increased risk of suicide attempts. Those pathways included differences in the signaling of oxytocin, a hormone involved in social bonding. Multiple stress pathways, including cortisol secretion and blood pressure regulation, were also found to be related to suicide risk. Subject groups also showed differences related to circadian rhythm. Identifying biological factors related to suicide risk could help identify new treatments, according to the researchers. (American Society of Human Genetics, Oct. 18, 2021)
|
Statin use disparities
 Photo: ©Getty Images/rogerashford (10/21/2021)
Disparities exist between which patients continue to take statins when experiencing side effects, according to a study by Michael E. DeBakey VA Medical Center researchers and colleagues. Statins are drugs that lower cholesterol. Side effects—such as headache, muscle pain, digestive problems, and poor sleep—are the leading cause of statin discontinuation. Researchers studied data on more than 1 million patients with atherosclerotic cardiovascular disease. Females, white patients, and those with high blood pressure or ischemic heart disease were at increased risk of statin side effects. Those receiving care at a teaching facility had lower risk. Among patients experiencing side effects, those with diabetes or ischemic heart disease and those with more cardiology visits were more likely to remain on statins. Being female was linked with lower odds of remaining on statins. The results suggest areas for improvement in optimizing statin use, say the researchers. (Journal of Clinical Lipidology, Oct. 2, 2021)
|
Many VA health care enrollees purchase outside insurance
 Photo: ©Getty Images/Andrei Sauko (10/21/2021)
Many enrollees of VA health care also acquire health insurance outside VA, found an Edward Hines, Jr. VA Hospital study. Researchers surveyed almost 4,000 Veterans enrolled in VA health care. Of those, 32% also had non-VA insurance. The most common reasons for having outside insurance were wanting coverage for emergency situations or family members. The largest barrier to outside insurance coverage was affordability. The results show the importance of meeting all of VA enrollees’ health care needs within VA and community care financed through VA, according to the researchers. (Medical Care Research and Review, Oct. 8, 2021)
|
Military sexual trauma independently increased suicide risk
 Photo: ©Getty Images/globalmoments (10/21/2021)
Military sexual trauma is a risk factor for suicide in Veterans without mental health diagnoses, found a study by VA Connecticut researchers. While sexual trauma is associated with suicidal ideation—thinking about suicide—less is known about this relationship when other mental health concerns, such as depression or PTSD, are not involved. Researchers examined more than 41,000 Veterans without a mental health diagnosis. They found that 28% of women and 3% of men reported military sexual trauma. Fifteen percent of women and 17% of men experienced suicidal ideation. Military sexual trauma was linked to a higher risk of suicidal ideation in both men and women. The findings suggest that instances of military sexual trauma should prompt suicide screening, say the researchers. (Psychiatric Research, September 2021)
|
Legal involvement increases risk of opioid overdose death
 Photo: ©Getty Images/South_agency (10/21/2021)
Legal system involvement was linked to increased risk of opioid overdose and death, in a study of VA patients. Researchers looked at data of more than 5 million Veterans who used VA health care. Of those, around 32,000 had legal system involvement, meaning they spent time in prison or jail. Veterans with legal involvement were significantly more likely to die from an opioid overdose, compared with those without legal involvement. The results show that opioid overdose prevention and naloxone distribution should target legally involved Veterans, say the researchers. (American Journal of Preventive Medicine, Sept. 11, 2021)
|
Poor diet quality in older Veterans with PTSD
 Photo: ©Getty Images/Mukhina1 (10/21/2021)
Older Veterans with PTSD may have poor quality of diet, found a pilot study by Durham VA researchers. Older Veterans with PTSD are at an increased risk of obesity and cardiovascular disease. Researchers examined the eating habits of 54 older Veterans participating in a supervised exercise trial. They found that consumption of added sugar exceeded dietary recommendations. Consumption of healthy foods such as whole grains, fruits and vegetables, and calcium fell short of recommendations. Participating in the exercise program did not affect diet quality. Interventions that target both diet and exercise are needed to address obesity and cardiovascular disease in Veterans with PTSD, conclude the researchers. (Translational Behavioral Medicine, Sept. 6, 2021)
|
Severe obesity a risk factor for death from COVID-19
 Photo: ©Getty Images/spukkato (10/06/2021)
Severe obesity increases the risk of death from COVID-19, according to a study of VA patients. Researchers looked at outcomes for more than 16,000 VA patients hospitalized with COVID-19 between March and November of 2020. Of those, 12% died in the hospital. Severe obesity, defined as a body mass index above 40 kg/m2, increased the risk of death by 43%. Obesity (BMI between 30 and 40) and sleep apnea did not increase the risk of death from COVID-19. According to the Centers for Disease Control and Prevention, a BMI between 18.5 and 24.9 is considered a healthy weight. Severe obesity should be considered an underlying medical condition when prioritizing treatment and predicting severe COVID-19 risk, conclude the researchers. (International Conference on Pharmacoepidemiology & Therapeutic Risk Management, Aug. 23, 2021)
|
Disability compensation may affect PTSD treatment response
 Photo: ©Getty Images/PeopleImages (10/06/2021)
Disability compensation status may affect how well Veterans respond to PTSD treatment, found a study by Battle Creek VA Medical Center researchers and colleagues. The researchers reviewed the charts of 105 Veterans undergoing cognitive processing therapy, a PTSD psychotherapy. Those seeking compensation from the Veterans Benefits Administration saw less symptom improvement. About 67% of non-compensation seeking Veterans saw clinically significant improvements. Only 40% of those who were seeking VBA benefits saw PTSD improvement. Some researchers and clinicians have suggested that Veterans may be concerned with losing their disability status if they show symptom improvement. Others fear that some Veterans may participate in mental health treatment to establish a basis for a PTSD claim, only to drop out after their claim is adjudicated. More research is needed on whether the benefits process unintentionally discourages PTSD improvement, say the researchers. (Psychiatric Quarterly, Sept. 17, 2021)
|
Transcranial magnetic stimulation safe for patients with alcohol use disorder
 Photo: ©Getty Images/gorodenkoff (10/06/2021)
Transcranial magnetic stimulation is safe for patients with alcohol use disorder (AUD), according to a Providence VA study. In transcranial magnetic stimulation, a magnetic field is applied to the skull to influence brain impulses. One form of this treatment, intermittent theta burst stimulation (iTBS), has potential as a treatment for PTSD and depression. However, there are some safety concerns about the treatment in patients with AUD. Researchers studied 50 Veterans with PTSD receiving iTBS, 17 of whom had AUD. iTBS was shown to be safe for AUD patients. These patients also had greater improvements in depression symptoms, compared to patients without AUD. AUD did not impact PTSD symptom change. The results suggest that AUD should not be excluded from receiving iTBS treatment, say the researchers. (Journal of Affective Disorders, Oct. 1, 2021)
|
Heart rate variability as a biomarker of PTSD treatment response
 Photo: ©Getty Images/Kativ (09/29/2021)
Heart rate variability could be a useful predictor of how patients with PTSD will respond to transcranial magnetic stimulation, according to a study by VA Providence researchers. PTSD is linked to problems with autonomic functions, such as elevated heart rate and reduced heart rate variability. Intermittent theta-burst stimulation (iTBS) is a form of transcranial magnetic stimulation, in which a magnetic field is applied to the head to affect brain signals. Researchers examined how well Veterans with PTSD responded to this treatment. Those with less dysfunction had greater PTSD symptom improvements from iTBS. Measuring abnormalities such as heart rate variability could be a useful way to gauge how patients will react to iTBS, say the researchers. (Neuromodulation, Sept. 27, 2021)
|
Cough medicine may reduce flu hospitalizations
 Photo: ©Getty Images/Photodisc (09/29/2021)
The drug dextromethorphan may reduce hospitalization from the flu, found a Columbia VA study. Dextromethorphan is an over-the-counter cough suppressant. It is sold as Robitussin, Delsym, and several other brands. Researchers looked at data on more than 18,000 Veterans with confirmed flu cases, nearly 3,000 of whom were given dextromethorphan. Those treated with the drug had a 34% reduced risk of being hospitalized. The chances of being hospitalized for a respiratory problem were even lower for treated patients, compared with patients not given the drug. The results suggest that dextromethorphan could be repurposed as a treatment for the flu, say the researchers. (Pharmacotherapy, Aug. 24, 2021)
|
Gender-based health care disparities
 Photo: ©Getty Images/FatCamera (09/29/2021)
A study by Michael E. DeBakey VA Medical Center researchers and colleagues examined how gender affects cost-related health care disparities. The researchers looked at data from a CDC survey of more than 1.7 million people. They found that women were more likely than men to delay health care, be unable to see a doctor because of cost, and have cost-related medication non-adherence. Women were less likely to not have health coverage or a primary care physician. These disparities were most pronounced in women younger than 45 and Black women. Identifying such health care barriers is crucial to ensuring equitable health care access for all, according to the researchers. (Preventive Medicine, Sept. 3, 2021)
|
Primary care employment support helps Veterans with psychiatric disorders
 Photo: ©Getty Images/ablokhin (09/22/2021)
Offering employment support in primary care helps Veterans with psychiatric disorders find meaningful employment, found a Tuscaloosa VA Medical Center study. Individual placement and support (IPS) is a program that helps Veterans with disabilities find personally matched work. But many find it stigmatizing to receive this service through mental health care. Some Veterans fear that they will not be able to find employment if their psychiatric needs are disclosed. Researchers studied the effectiveness of IPS integrated with VA primary care. Nearly twice as many IPS participants achieved steady work, compared with controls receiving standard vocational rehabilitation. IPS participants worked significantly more weeks and earned more income from competitive jobs. The results show that integrating IPS with primary care is feasible and effective, say the researchers. (Psychiatric Services, Sept. 15, 2021)
|
Gulf War chemical exposure could cause cell dysfunction
 Image: ©Getty Images/wir0man (09/22/2021)
A combination of toxins can cause cell dysfunction related to Gulf War illness, according to a study by VA New Jersey researchers. Previous studies have suggested that GWI is related to exposure to various toxins during service. Researchers exposed human cells in the lab to three chemicals: a pesticide, an insect repellant, and a nerve gas antitoxin. Service members were commonly exposed to these chemicals during the Gulf War. Exposure to all three together caused mitochondrial dysfunction in the cells. Problems with cell function could cause GWI symptoms such as fatigue, forgetfulness, and muscle pain, according to the researchers. Combined exposure to all three toxins should be examined as a possible cause of GWI, they say. (Journal of Biochemical and Molecular Toxicology, Sept. 15, 2021)
|
Differentiating between Veterans who think about and attempt suicide
 Photo: ©Getty Images/AntonioGuillem (09/22/2021)
A study of more than 4,000 Veterans identified demographic differences between those who only have suicidal thoughts and those who attempt suicide. Out of the sample, 26% thought about suicide at some point in their lives. Four percent attempted suicide. Several factors distinguished Veterans with a history of a suicide attempt from those with suicidal thoughts only. Factors linked to suicide attempts were younger age, nonsuicidal self-injury, adverse childhood experiences, alcohol use disorder, lower household income, and physical disability. These factors should be considered when assessing Veterans for suicide risk, say the researchers. (General Hospital Psychiatry, September-October 2021)
|
Review: No link between cinnamon and lower cardiovascular risk
 Photo: ©Getty Images/Marat Musabirov (09/16/2021)
Consuming cinnamon does not appear to reduce cardiovascular risk, according to a review by Michael E. DeBakey VA Medical Center researchers. Cinnamon is used as a traditional medicine for a variety of conditions by many cultures. Researchers performed a literature review of published studies on the effects of cinnamon on cardiovascular risk. They identified 23 studies. The existing research shows no differences in hemoglobin A1c levels or both types of cholesterol for patients who did or did not consume cinnamon. The results suggest that cinnamon has no effect on these measures of cardiovascular risk, say the researchers. (American Journal of Medicine, Aug. 16, 2021)
|
High altitude may negatively affect brain chemistry
 Photo: ©Getty Images/Aaron Hawkins (09/16/2021)
Living at a higher altitude could negatively affect brain chemistry, found a study by VA Salt Lake City researchers and colleagues. Epidemiological studies have suggested that living at high altitude may be a risk factor for mood disorders, substance abuse, and suicide. The researchers used brain imaging to compare metabolite levels in the brains of patients living in Utah, Massachusetts, and South Carolina. Metabolites are molecules that the brain needs to function properly. Patients in Utah, which is at a higher elevation, had lower levels of several brain metabolites, compared with patients in the two other locations closer to sea level. Larger studies are needed to examine how altitude affects brain chemistry and mental health conditions, according to the researchers. (Psychiatry Research: Neuroimaging, Aug. 30, 2021)
|
PTSD and traumatic brain injury alter brain connectivity
 Photo: ©Getty Images/koya79 (09/16/2021)
Patients with PTSD and blast-related mild traumatic brain injury showed significant alterations to neural connections in the brain, in a Salisbury VA and Wake Forest School of Medicine study. Researchers used imaging to map the network of connections in patients’ brains. Patients with both PTSD and mild TBI shared structural characteristics in the brain that were not present in patients with PTSD only. The findings demonstrate that TBI and PTSD interact to create distinct neurological damage in the brain. The evidence strongly supports mild TBI as a risk factor for PTSD, according to the researchers. The connection patterns identified could aid in diagnosing both conditions, they say. (Journal of Neurotrauma, Aug. 26, 2021)
|
COVID-19 pandemic has not increased suicide risk in Veterans
 Photo: ©iStock/Cortney Hale (08/30/2021)
The COVID-19 pandemic has not increased suicidal behavior among Veterans, according to a VA National Center for PTSD study. Many scholars warned that hardships and isolation caused by the pandemic could create a “perfect storm” of suicide risk among vulnerable populations. Researchers surveyed more than 3,000 Veterans in November 2019, and again in November 2020. They found that rates of suicidal thoughts actually decreased by nearly a third during the pandemic, from 10.6% of Veterans surveyed to 7.8%. The number of suicide attempts did not increase during the study period. However, Veterans who contracted COVID-19 were more than twice as likely to report suicidal thoughts than they were before infection. The results suggest that the resiliency of Veterans and increased social support may be protective against suicide risk during a health crisis, according to the researchers. More research is needed into how the physical and social effects of COVID-19 infection may affect suicide, they say. (JAMA Psychiatry, Aug. 25, 2021)
|
PTSD treatment improves sleep
 ©iStock/Wavebreakmedia Photo for illustrative purposes only. (08/30/2021)
PTSD treatments improve sleep difficulties, according to a review that included a VA Greater Los Angeles researcher. Patients with PTSD often have difficulties with sleep. Researchers reviewed 89 studies on various PTSD treatments. They found that treatments that improved PTSD symptoms also improved sleep. Different types of treatment all led to better sleep. Interventions that specifically targeted sleep were more effective at improving sleep outcomes than other PTSD treatments. The results show that treatments that target sleep improvement may be helpful for patients with PTSD, say the researchers. (Sleep Medicine, Aug. 19, 2021)
|
Testosterone treatment not associated with cardiovascular events
 Image: ©iStock/Evgeny Gromov (08/30/2021)
Testosterone treatment in not associated with increased risk of cardiovascular events, found a study by VA Puget Sound researchers and colleagues. Concerns have been raised that treating men with testosterone could lead to cardiovascular events such as heart attack and stroke. The researchers studied more than 200,000 male Veterans with low testosterone levels. They found that testosterone treatment was not linked to increased cardiovascular events in patients without cardiovascular disease. In patients with cardiovascular disease, testosterone treatment was linked to lower risk. The results provide some reassurance that testosterone treatment does not pose a significant risk for cardiovascular events, say the researchers. (Journal of the American Heart Association, Aug. 21, 2021)
|
New tool to predict suicide risk
 Photo: ©iStock/PeopleImages (08/26/2021)
Durham VA researchers and colleagues created an accurate tool for predicting future suicide attempts. The researchers gathered data from a nationwide study and two smaller Veteran studies, for a total of over 35,000 participants. They developed a tool, the Durham Risk Score, based on psychiatric, social, economic, and health risk factors. The score proved to be a strong predictor of future suicide attempts. It performed well among multiple subgroups, including people of different ethnicities, Veterans, low-income people, and LGBTQ people. The results suggest that the Durham Risk Score represents a significant advancement in suicide risk prediction, say the researchers. (PLoS Medicine, Aug. 5, 2021)
|
Smoking, alcohol use tied to lower mortality risk in COVID-19 patients
 Photo: ©iStock/Dusan Ilic (08/26/2021)
Risk factors for death differ in COVID-19 infected and uninfected patients, found a Durham VA and Duke University study. Researchers compared mortality rates between Veterans with and without COVID-19 who had similar risk factors. They looked at outcomes of more than 340,000 male Veterans tested for COVID-19 between March and September 2020. Of those, 7% tested positive. Older age and obesity both increased the chance of death in patients with COVID-19 beyond the risk in similar patients not infected. Surprisingly, COVID-19 patients who smoked or had alcohol use disorder had lower mortality risk than patients who did not smoke or had alcohol use disorder. Both smoking and alcohol use disorder increased mortality risk in patients without COVID-19. More study is needed on why normally harmful behaviors might be associated with better mortality outcomes in COVID-19 patients, say the researchers. (International Journal of Environmental Research and Public Health, Aug. 11, 2021)
|
Treating vitamin D deficiencies could lower risk of heart attack, death
 Photo: ©iStock/yulka3ice (08/26/2021)
Treatment of vitamin D deficiencies may help prevent heart attacks and death, according to a study by Kansas City VA and University of Kansas Medical Center researchers. The study included more than 20,000 VA patients with low vitamin D levels. Patients given vitamin D to correct the deficiency had significantly lower chance of death from any cause, compared with those not given vitamin D. Patients whose vitamin D levels were maintained above a certain level were less likely to have a heart attack, compared with patients treated with a lower level of vitamin D. The findings suggest that correcting vitamin D deficiency could improve patients’ health outcomes, say the researchers. (Journal of the Endocrine Society, July 15, 2021)
|
Racial gaps in PTSD treatment outcomes
 Photo: ©iStock/Prostock-Studio (08/18/2021)
A VA study found that Black Veterans saw less improvement than white Veterans from PTSD treatment. Researchers looked at outcomes for 2,870 Veterans in a residential rehabilitation treatment program. Compared with white Veterans, Black Veterans had lower PTSD symptom reduction during treatment. They also had greater depression symptom recurrence four months after discharge. Importantly, both Black and white Veterans had PTSD symptom improvements during treatment. More study is needed to understand the causes of these differences in mental health treatment outcomes, say the researchers. (Psychiatric Services, Aug. 9, 2021)
|
Convalescent plasma treatment did not affect COVID-19 mortality
 Image: ©iStock/Floriana (08/18/2021)
Convalescent plasma treatment did not reduce mortality in patients with non-severe COVID-19, in a study of VA patients. Convalescent plasma is a treatment using the blood from a person who has recovered from COVID-19. Scientists hypothesized that transferring antibodies to the new patients could improve recovery. Out of nearly 5,000 VA patients admitted for non-severe COVID-19 between May and November of 2020, about 8% received convalescent plasma. Thirty-day mortality for the convalescent plasma patients was 6.5%, compared with 6.2% in other patients. The results show no meaningful differences between patients treated or not treated with convalescent plasma for non-severe COVID-19, according to the researchers. (Journal of Infectious Disease, June 21, 2021)
|
Toxic exposure increases Gulf War illness likelihood in women Veterans
 Photo: ©iStock/Brasil2 (08/18/2021)
Women Gulf War Veterans exposed to toxins were significantly more likely to have Gulf War illness than those without toxic exposures, found a study by VA Boston researchers. They surveyed 202 women Veterans who deployed during the Gulf War. Self-reported exposure to pesticides, oil well fires, and anti-nerve gas medication increased the likelihood of meeting Gulf War illness criteria. Results also suggest that women exposed to particular toxic substances may benefit from more targeted treatment strategies, according to the researchers. (Life Sciences, Sept. 1, 2021)
|
Chronic pain may disrupt nervous system, lead to walking problems
 Photo: ©iStock/Piyapong Thongcharoen (08/10/2021)
Chronic pain may impact the body’s nervous system responses and disrupt a person’s walking, found a study including a Malcom Randall VA Medical Center researcher. Researchers measured sympathetic reactivity—how the body responds to danger or complex tasks such as walking on uneven terrain—by measuring skin conductivity. They found that participants with chronic pain had lower sympathetic reactivity when walking over obstacles, compared with participants without pain. They also found that blunted sympathetic reactivity was linked to disruptions in the brain’s autonomic network structure, the part of the brain responsible for involuntary actions such as heartbeat and breathing. The results suggest that chronic pain may negatively impact the body’s autonomic responses, which could lead to walking problems and falls, say the researchers. (Chronic Stress, July 7, 2021)
|
Gulf War illness symptoms persist 25 years later
 Photo: ©iStock/robertcicchetti (08/10/2021)
A survey of Gulf War Veterans by Durham VA researchers found evidence of sustained, multis-symptom illness decades after deployment. Researchers surveyed more than 1,000 Veterans of the Gulf War era for Gulf War illness symptoms. Using the Centers for Disease Control and Prevention (CDC) definition of Gulf War illness, 84% of Veterans surveyed had the condition. Under the Kansas criteria, a different measure of the condition, 40% had the condition. Veterans who were deployed had higher odds of having symptoms related to Gulf War illness, compared with non-deployed Veterans. Symptom differences between deployed and non-deployed Veterans have diminished since initial reports. This suggests that definitions of Gulf War illness need to be updated to take into account age-related conditions, say the researchers. (Life Science, Aug. 1, 2021)
|
TBI and PTSD affect coping skills and self-efficacy differently
 ©iStock/molchanovdmitry (08/10/2021)
Traumatic brain injury and PTSD change Veterans’ coping skills and self-efficacy, according to a study by VA San Diego researchers. Analysis of a group of Iraq and Afghanistan-era Veterans revealed that those with both mild TBI and PTSD had lower self-efficacy than Veterans with TBI only or neither condition. Self-efficacy refers to confidence in one’s ability to achieve goals. Veterans with PTSD but not TBI used less action-focused coping than those with only TBI or neither condition. The results suggest that treatments for TBI and PTSD should consider the interplay of the two conditions, say the researchers. (Journal of Clinical Psychology, May 15, 2021)
|
Equal access to VA COVID-19 testing among racial groups
 Photo: ©iStock/ljubaphoto (08/04/2021)
Minority Veterans have had equal or greater access as White Veterans to COVID-19 testing from VA during the pandemic, found a VA Greater Los Angeles study. Researchers looked at data on the nearly 1 million Veterans who sought care through VA for COVID-19 symptoms or exposure in 2020. Early in the pandemic, Hispanic, Black, and other non-White minorities were more likely than White patients to receive COVID-19 tests. As the pandemic continued, testing was similar in VA among all racial and ethnic groups. As periodic testing shortages continue, it is important to ensure that groups with increased COVID-19 exposure risk continue to have equal access to testing, say the researchers. (Preventive Medicine Reports, July 22, 2021)
|
Gulf War toxic exposure may be linked to damaging gene expression changes
 Photo: ©iStock/koto_feja (08/04/2021)
Toxic exposure during the Gulf War may alter gene expression in the hippocampus, which could cause memory problems, found a VA New Jersey study. The hippocampus is a part of the brain involved in spatial memory. Researchers simulated Gulf War toxic exposure in mice using three chemicals: two insecticides and an anti-sarin prophylactic. The chemical exposure resulted in inflammation and other changes in gene expression in the hippocampus. Genes involved in neuron health were downregulated after chemical exposure. The results suggest that exposure to these toxic substances could cause chronic neurodegeneration. The findings could help explain how Gulf War illness develops, according to the researchers. (Life Sciences, July 20, 2021)
|
Knee replacement surgery at VA facilities leads to fewer complications than community surgeries
 Photo: ©iStock/kckate16 (08/04/2021)
Veterans receiving knee replacement surgery at VA facilities generally have fewer complications than those who receive VA-purchased surgery in the community, found a VA study. In addition to delivering health care directly, VA is increasingly purchasing health care for Veterans in the community. Researchers compared post-surgery complications between Veterans who had knee replacement surgery at VA and in the community. Overall, complication rates were significantly lower for VA-performed surgeries. However, there were five locations where VA-purchased care outperformed VA-delivered care. However, there were five locations where VA-purchased care outperformed VA-delivered care. In an email, lead researcher Dr. Alex Sox-Harris emphasized that the findings at those sites should not be “misinterpreted to mean those five facilities provided suboptimal care. We did not look at that directly. What we can say is that those five facilities managed to purchase care of even better quality than they delivered.” The results highlight the importance of monitoring quality of care both at VA facilities and where Veterans receive outside care, say the researchers. (Health Affairs, August 2021)
|
Shorter antibiotic treatments effective at treating UTIs in men
 Photo: ©iStock/Ridofranz (07/28/2021)
A shorter course of antibiotics can effectively treat urinary tract infections in men, according to a study by Minneapolis VA and Michael E. DeBakey VA Medical Center researchers. Standard treatment for UTIs is antibiotics for 7 to 14 days. In a study of more than 300 men, taking antibiotics for seven days was as effective as a 14-day course at resolving symptoms. Being on antibiotics for a shorter period of time is easier on patients who may experience side effects, say the researchers. Shortening the course of antibiotic treatment is also important for preserving the overall effectiveness of antibiotics. (JAMA, July 27, 2021)
|
Program could prevent suicide after psychiatric hospitalization
 Photo: ©iStock/PeopleImages (07/28/2021)
A brief intervention could help prevent suicide after psychiatric hospitalization, found a White River Junction VA study. Risk for suicide is high after psychiatric hospitalization. The World Health Organization’s Brief Intervention and Contact (BIC) program has shown some success at preventing suicide for these patients. Researchers tested the effectiveness of the BIC adapted for VA patients. The VA BIC program consists of six sessions within three months of discharge. Sessions include education about suicide prevention resources and conversations about motivation and social support. They found that, one month after discharge, the intervention led to meaningful reductions in suicidal thoughts. VA BIC also led to improvements in social connectedness, feelings of hopelessness, and engagement. The results show that the VA BIC program may be useful for preventing Veteran suicide during a vulnerable time, according to the researchers. (Psychiatric Services, May 12, 2021)
|
Factors associated with homelessness
 Photo: ©iStock/MattGush (07/28/2021)
Birmingham VA researchers and colleagues identified both individual and community risk factors for homelessness in Veterans. They surveyed more than 5,000 Veterans. Of those, 9% had at least seven nights unsheltered over a six-month period. Veterans experiencing homelessness were more likely to report criminal justice history, poor social support, medical and drug problems, financial hardships, and being unmarried. The communities they lived in had poorer shelter access and warmer temperatures. Having more than one of these risk factors increased the chances of homelessness significantly. The results show the need to consider both individual and community factors when addressing Veteran homelessness, say the researchers. (American Journal of Preventive Medicine, July 15, 2021)
|
Nasal swab COVID-19 test less sensitive, easier than sinus swab
 Photo: ©iStock/Giuseppe Lombardo (07/21/2021)
Nasal swabs are less sensitive than deeper sinus swabs at detecting the virus that causes COVID-19 but are still highly accurate, found a study by a VA researcher. The “gold standard” for detecting SARS-CoV-2 is a nasopharyngeal swab, which takes a sample from the back of the sinuses through the nose. Researchers reviewed studies of how effective this type of COVID-19 test was compared with nasal swabs taken from the nostrils. They found that nasal swabs were 82% to 88% effective at detecting the virus, compared with 98% for nasopharyngeal swabs. However, nasal swabs are quicker to perform and require less protective equipment. The lower sensitivity of nasal swabs is balanced by the ability to screen more patients and the easier procedure, conclude the researchers. (PLoS One, July 20, 2021)
|
Remdesivir linked to longer hospital stays for COVID-19 patients
 Photo: ©iStock/Hispanolistic (07/21/2021)
Remdesivir treatment was associated with longer hospital stays for COVID-19 patients, in a study by Iowa City VA researchers. Previous studies suggested that the drug remdesivir can reduce recovery time for COVID-19 patients. Researchers looked at data on nearly 6,000 Veterans treated for COVID-19 at VA medical centers. Of those, 40% received remdesivir. Patients given remdesivir had longer median hospital stays than patients not treated with the drug. Remdesivir did not appear to reduce patients’ 30-day risk of death. Because the treatment lasts several days, remdesivir may increase the need for hospital beds for COVID-19 patients while not improving survival, say the researchers. (JAMA Network Open, July 1, 2021)
|
Eating disorder symptoms linked to trouble at work
 Photo: ©iStock/Daisy-Daisy (07/21/2021)
An eating disorder can lead to worse functioning at work in women Veterans, according to a VA Boston study. Researchers surveyed 198 female Veterans. They found that high eating disorder symptoms were linked to worse occupational functioning, a measure of how well an employee performs at a job. Eating disorder symptoms were not linked to employment status. The link between having an eating disorder and having trouble at work was largely mediated by depression symptoms. The results suggest that depression may be an important treatment target for women with eating disorders and work problems, say the researchers. (Eating Behaviors, June 21, 2021)
|
Telehealth increases specialty pain care use
 Photo: ©iStock/Nattakorn Maneerat (07/14/2021)
Telehealth led to an increase in specialty pain services use among VA patients with chronic care, found a study by VA Puget Sound researchers. The study examined health care use by more than 33,000 Veterans over a five-year period. Specialty pain care use increased from 11% to 16% after a telehealth program was introduced. This increase occurred in both urban and rural patients, although the increase was smaller for rural patients. Among rural patients using specialty pain care, 12% used telehealth, compared with only 3% of urban patients. The results suggest that telehealth may increase patients’ access to specialty pain services, say the researchers. (Pain Medicine, June 18, 2021)
|
Brief intimate partner violence counseling program shows promise
 Photo: ©iStock/Jose Girarte (07/14/2021)
A counseling program for women who experience intimate partner violence proved potentially helpful, in a VA pilot study. Recovering from IPV through Strengths and Empowerment (RISE) is an empowerment and skills-focused treatment. It involves motivational interviewing in up to six sessions. Fifteen women Veterans who experienced intimate partner violence within the past year participated in a pilot of the program. Results suggest RISE improves psychosocial well-being. Both participants and clinicians gave positive feedback on the program, with the participants giving high retention and satisfaction ratings. The results show that RISE could be effective for women who experience intimate partner violence, say the researchers. (Psychological Services, June 2021)
|
Transportation a barrier to colon cancer care
 Photo: ©iStock/humonia (07/14/2021)
Transportation is a barrier to colorectal cancer care, according to a study by VA researchers and colleagues. Researchers mailed surveys to 115 Veterans with colorectal cancer. Of those, 18% reported transportation barriers that made attending appointments difficult. The distance a patient lived from a VA facility was not linked to transportation barriers. The greatest contributor to transportation barriers was a chaotic lifestyle. Identifying Veterans with chaotic lifestyles for interventions such as organizational skills training could improve colorectal cancer outcomes, say the researchers. (BMC Health Services Research, April 13, 2021)
|
Race more important than rural-urban residency in suicide risk
 Photo: ©iStock/pixdeluxe (07/06/2021)
Race significantly affects the relationship between rural residence and suicide risk, according to a VA White River Junction study. Researchers looked at data on nearly 11 million VA patients over a 15-year period. They found that patients who live in rural areas have a significantly higher risk of suicide, compared with more urban residents. However, this connection disappeared when race was considered. Rural living significantly increased suicide risk for Hispanic patients, but not for Black or White patients. White VA patients had the highest suicide rates of any group, regardless of where they lived. The results show that race must be considered when studying the effects of location of suicide risk, say the researchers. (Journal of Rural Health, June 15, 2021)
|
Public transportation, high Veteran population increase VA health care use
 Photo: ©iStock/Bim (07/06/2021)
Public transportation and the size of Veteran populations influence how likely formerly homeless Veterans are to use VA health care, found a VA study. Researchers looked at data on 711 Veterans in VA’s permanent supportive housing program. They found that Veterans in neighborhoods with a high percentage of Veteran residents were more likely to use emergency departments, compared to those in other areas. In areas with high public transportation use, Veterans had increased likelihood of emergency department and primary care visits. Neighborhoods with more property vacancies had increased outpatient mental health visits. The results highlight the importance of public transportation availability and social engagement with other Veterans in getting homeless Veterans to use VA health care, according to the researchers. (Psychological Services, June 3, 2021)
|
A1c variability linked to increased risk of death in diabetes patients
 Photo: ©iStock/jarun011 (07/06/2021)
Maintaining hemoglobin A1c at steady levels lowers risk of death in older patients with diabetes, found a VA Boston study. Hemoglobin A1c is a type of blood cell that is linked to sugar. Measuring A1c levels is a common test of how well diabetes is being managed. Researchers studied how variations in A1c levels affected outcomes in more than 400,000 older Veterans with diabetes. Patients whose A1c levels were less often within the targeted range set by each individual’s doctors had a higher risk of death, compared with patients whose A1c levels were more stable. More variable A1c levels were also associated with greater cardiovascular disease risk. The results show that reducing A1c variability is important for lowering mortality and cardiovascular risk in diabetic patients, say the researchers. (Diabetes Care, June 14, 2021)
|
Social and behavioral risk factors did not increase COVID-19 mortality risk in Veterans
 Photo: ©iStock/sasirin pamai (06/29/2021)
Social and behavioral risk factors were not associated with death from COVID-19 in VA patients, in a study of more than 27,000 Veterans. Researchers looked at data on Veterans with a positive COVID-19 test between March and September of 2020. They found that Veterans with risk factors traditionally associated with barriers to care had no higher risk of dying from COVID-19 than patients without those risk factors. Social risk factors included housing problems and financial hardship. Behavioral risk factors included tobacco, alcohol, and drug use. The results show that an integrated health system such as VA can transcend social vulnerabilities that often lead to health care disparities, according to the researchers. (JAMA Network Open, June 9, 2021)
|
Psychiatric issues increase risk of multiple suicide attempts
 Photo: ©iStock/ligonpix (06/29/2021)
Veterans who attempt suicide had greater psychiatric issues than those with only one suicide attempt, according to a VA study. Half of military Veterans who attempt suicide report more than one attempt. Researchers looked at data on more than 4,000 Veterans who attempted suicide. They found that Veterans with multiple attempts had higher rates of lifetime depression, non-suicidal self-injury, and substance use disorder, compared with those who made only one attempt. Veterans with multiple suicide attempts were also less likely to be married or living with a partner. The results highlight the importance of examining risk factors for single and multiple suicide attempts separately, say the researchers. (Journal of Psychiatric Research, June 7, 2021)
|
High-performance brain-to-text communication
 Photo: ©iStock/baona (06/29/2021)
A team including a Providence VA researcher developed a brain-computer interface that allowed a paralyzed user to quickly type just by thinking. Brain-computer interfaces allow people who have lost the ability to move or speak to interact directly with computers by reading brain signals. Most brain-computer interfaces for typing have focused on moving and clicking a computer cursor. The researchers developed a system in which a paralyzed participant thought about writing by hand. The computer analyzed patterns in the participant’s motor cortex and converted them to text. The participant achieved typing speeds of 90 characters per minute. Raw typing accuracy was 94%, with 99% accuracy using an autocorrect program. This type of brain-computer interface could enable faster communication than point-and-click typing, say the researchers. (Nature, May 12, 2021)
|
Predictors of response to PTSD treatment
 Photo for illustrative purposes only. ©iStock/Courtney Hale (06/23/2021)
Time since trauma is an important predictor of how well patients respond to PTSD treatment, found a VA study. Patients were given a combination of prolonged exposure psychotherapy and the drug sertraline (sold as Zoloft). Those with a longer time since their trauma exposure had the greatest PTSD symptom improvement 24 weeks after treatment. Higher baseline pain severity predicted smaller symptom improvement. Hispanic patients also showed greater improvement than non-Hispanics. Alcohol use did not impede the effectiveness of treatment. The findings suggest that patients who might not seek help for years following trauma can still benefit from PTSD treatment, say the researchers. (Journal of Clinical Psychiatry, June 15, 2021)
|
Phone intervention can relieve PTSD caregiver burden
 Photo: ©iStock/KatarzynaBialasiewicz (06/23/2021)
A behavioral intervention program can help relieve burden for caregivers of Veterans with PTSD, found a Memphis VA study. Loved ones caring for Veterans with PTSD often face stress that may seem overwhelming. The REACH VA intervention aims to help caregivers cope and manage PTSD-related concerns. It includes four one-hour sessions delivered by phone. In a group of 161 caregivers, the program significantly improved burden, depression, anxiety, frustrations, general stress, time providing care, troubling behavior, and safety risk. REACH can help reduce caregivers’ psychological distress and can improve their ability to care for Veterans with PTSD, concluded the researchers. (Military Behavioral Health, May 27, 2021)
|
Discussing firearms storage safety in primary care
 Photo: ©iStock/NoDerog (06/23/2021)
Veterans are open to discussing firearms storage safety in primary care as long as it is done in a Veteran-centric manner, according to a study by VA Portland researchers. Two-thirds of Veteran suicides involve a firearm. Researchers surveyed 68 Veterans about their views on discussing firearms during health care visits. The Veterans generally accepted discussing firearms in primary care. However, most did not support direct questions about gun ownership because of fears of having firearm access taken away or limited. Participants suggested using personalized, caring, and conversational approaches to the discussions rather than scripted checklists. They said that Veterans should be engaged in a non-judgmental manner that respects a Veteran’s knowledge of firearms. Participants also suggested that care teams provide information on legal consequences of disclosing gun ownership. The results show that discussing firearms storage safety could help with suicide prevention efforts when done correctly, say the researchers. (Journal of General Internal Medicine, June 2021)
|
Trauma-sensitive yoga effective treatment for PTSD
 Photo: ©iStock/fizkes (06/16/2021)
Trauma-sensitive yoga may be an effective treatment for PTSD in women Veterans who experienced military sexual trauma, found an Atlanta VA study. Women Veterans with PTSD participated in either a yoga program or cognitive processing therapy, a psychotherapy. The yoga program involved 10 weekly 60-minute group sessions. Trauma-sensitive yoga focuses on establishing safety, individual choice, and being in the present moment, along with the physical movements. Both groups saw clinically meaningful improvements in PTSD symptoms after treatment. While improvement rates were similar, 60% of the women in the yoga group completed their treatment. Only 35% in the cognitive processing therapy group completed treatment. The results show that yoga could be an effective alternative to trauma-focused therapy, say the researchers. (Journal of Alternative and Complementary Medicine, March 2021)
|
Chronic pain linked to cognitive processing problems in Gulf War Veterans
 Photo: ©iStock/ljubaphoto (06/16/2021)
Pain interferes with cognitive processing in Gulf War Veterans, according to a William S. Middleton Memorial Veterans Hospital study. Both disrupted thinking and chronic musculoskeletal pain are common in Gulf War Veterans. Researchers performed magnetic resonance imaging on Veterans with chronic pain while running through cognitive tests. Imaging showed that Veterans with chronic musculoskeletal pain required more neural resources to sustain cognitive performance during pain stimuli, compared with controls without chronic pain. The results suggest that Veterans with chronic pain linked to Gulf War illness may have abnormal pain processing, according to the researchers. (Life Sciences, May 26, 2021)
|
Soldiers with chronic pain likely to use VA health care
 Photo: ©iStock/gsheldon (06/16/2021)
The majority of soldiers with chronic pain were likely to use VA health care after separating from the military, found a study by VA researchers. The study looked at data on nearly 140,000 soldiers who served between 2008 and 2014. Of those who met the criteria for chronic pain, 79% began using VA health care after leaving the military. Veterans who used VA health care as a non-enrollee prior to military separation were more likely to use VA after separation. Separating for disability, having mental health conditions, and being of Black or Hispanic ethnicity all predicted VA health care use. Of all the soldiers who enrolled in VA health care, about 50% had chronic pain. The findings show that careful coordination of pain management between the military health service and VA is needed to optimize care, say the researchers. (BMC Health Services Research, May 24, 2021)
|
Alzheimer’s screening tool highly effective in Mexican American patients
 Photo for illustrative purposes only. ©iStock/ajr_images (06/08/2021)
A blood-based screening tool can help detect Alzheimer’s disease and may increase Mexican Americans’ access to clinical research, found a study including VA researchers. Mexican Americans have been poorly represented in Alzheimer’s disease research. As part of the Health & Aging Brain among Latino Elders (HABLE) study, researchers studied data on 1,600 patients. About half were Mexican American, and the other half were non-Hispanic whites. Profiling the protein content of patients’ blood was highly accurate in detecting mild cognitive impairment and dementia. Blood protein profiles varied significantly between ethnic groups and disease state. The findings could help bridge the gap between community-based and clinical settings and recruit more Hispanic patients into Alzheimer’s disease research, say the researchers. (Alzheimer’s and Dementia, May 31, 2021)
|
Diabetes linked to worse COVID-19 outcomes
 Photo: ©iStock/vitapix (06/08/2021)
Diabetes is linked to worse outcomes from COVID-19 infection, according to a VA Puget Sound study. Researchers looked at outcomes form nearly 36,000 VA patients who tested positive for COVID-19. Patients with diabetes had greater odds of hospitalization, intensive care unit admission, and death than patients without diabetes. Prior use of the diabetes medication sulfonylurea was linked to increased odds of hospitalization. Prior insulin use was linked to increased odds of both hospitalization and death. Statin use was associated with lower chance of death, and angiotensin receptor blockers (ARBs) were associated with lower odds of hospitalization. The results show that diabetes can increase the danger posed by COVID-19. (BMJ Open Diabetes Research and Care, June 2021)
|
Some VA therapists more effective than others at treating PTSD
 Photo: ©iStock/FatCamera (06/08/2021)
Some therapists are more effective than others at keeping patients engaged in PTSD treatment, found a study by VA researchers. The study looked at data on nearly 3,000 therapists providing the psychotherapies cognitive processing therapy (CPT) or prolonged exposure (PE) to more than 18,000 VA patients with PTSD. Results showed that dropout rates varied by 11% for CPT and 6% for PE between different therapists. Whether or not patients received an adequate psychotherapy dose varied by as much as 9% for both therapies based on therapist. The VA facility where a patient received care accounted for only a 1% to 3% variance in dropout and adequate dose rates. The results show that therapist skill and work environment are important to the success of PTSD treatment, say the researchers. (Journal of Traumatic Stress, May 28, 2021)
|
COVID-19 vaccines largely effective in inflammatory bowel disease patients taking immunosuppressants
 Photo: ©iStock/Juanmonino (06/03/2021)
Vaccination against COVID-19 proved mostly effective in patients with inflammatory bowel disease, found a Michael J Crescenz VA Medical Center study. Clinical trials of COVID-19 vaccines mostly excluded patients taking immunosuppressive medication, which keep the immune system in check. The researchers studied outcomes for nearly 15,000 patients taking medication for inflammatory bowel disease. Full vaccination—meaning patients were at least a week past the second vaccine dose—showed 80% effectiveness against COVID-19. Unvaccinated patients in this population had a much higher rate of COVID-19 infection than vaccinated patients. Partial vaccination did not significantly reduce the hazard of infection. The results could help increase patient and provider willingness to vaccinate immunosuppressed patients, say the researchers. (Gastroenterology, May 25, 2021)
|
Depression and other conditions often co-occur
 Photo: ©iStock/Srdjanns74 (06/03/2021)
Veterans with depression often have other psychiatric conditions, according to a study by VA researchers and colleagues. Researchers surveyed nearly 3,000 Veterans receiving treatment for depression in VA. They found that almost all patients screened positive for at least one other mental health condition. About half had four or more conditions. The most common conditions were generalized anxiety disorder, PTSD, and panic/phobia. Results showed that depression severity plays a large role in impairment caused by other mental health conditions. The findings suggest that addressing depression could help improve symptoms of other mental health conditions, say the researchers. (Journal of Affective Disorders, April 27, 2021)
|
Affordable Care Act reduced catastrophic health costs for young Veterans
 Photo: ©iStock/hudiemm (06/03/2021)
The Affordable Care Act reduced catastrophic health expenditure among young Veterans, found a study by VA Greater Los Angeles researchers. While some Veterans receive health care through VA, many get their health coverage outside the system. Researchers looked at health care costs for more than 13,000 Veterans receiving health care outside VA before and after the Affordable Care Act was passed. Catastrophic health expenditure was defined as health care costs of more than 10% of the yearly family income. They found that the Act was linked to a 26% decrease in the likelihood of a catastrophic health expenditure in Veterans aged 18 to 64. Veterans 65 and older did not see a similar reduction in catastrophic health care costs. The results highlight gaps in Veterans’ financial protection based on age, say the researchers. (Journal of General Internal Medicine, May 6, 2021)
|
Most adult COVID-19 patients develop antibodies
 Image: ©iStock/wildpixel (05/27/2021)
Most adults with COVID-19 develop antibodies that stay in the body after infection, according to a review by VA Portland researchers. The researchers surveyed studies published on COVID-19 in 2020. They found that most adults had detectable levels of antibodies after infection with the SARS-CoV-2 virus. Levels of IgM, short-term antibodies that protect from initial infection, peak at about 20 days after infection and then decline. IgG—longer-term antibodies—levels peak about 25 days after symptom onset and remain detectable for at least 120 days. Some evidence suggests that older age, greater COVID-19 severity, and presence of symptoms may be linked to higher antibody levels. Some adults do not develop antibodies for unclear reasons. (Annals of Internal Medicine, March 16, 2021)
|
PTSD treatment more effective in patients with specific brain traits
 Image: ©iStock/johan63 (05/27/2021)
VA San Diego researchers identified brain network traits that could predict which patients will see an improvement of PTSD symptoms from psychotherapy. The researchers took magnetic resonance imaging (MRI) scans of the brains of 53 patients with both PTSD and alcohol use disorder. They found that a subgroup of patients with specific brain connectivity traits were more likely than others to benefit from prolonged exposure therapy. They did not find any brain connectivity patterns related to alcohol consumption. The results could lead to treatments that target brain connectivity to boost treatment effectiveness, say the researchers. (Psychological Medicine, April 30, 2021)
|
Veterans more likely to use community care in rural areas
 Photo: ©iStock/JamesBrey (05/27/2021)
How rural the area is and the closeness of VA facilities affected how frequently Veterans used community health care, found a VA Boston study. In 2014, the Veterans Choice Act made it possible for some VA patients to receive health care in the community instead of from VA facilities. Researchers looked at data from over 3,000 counties across the country. Rural counties saw the greatest increase in community care use. Counties with a VA facility were less likely to see community care increases. The results suggest that community care may enhance primary care access for Veterans in areas farther away from VA facilities, according to the researchers. (Medical Care, June 1, 2021)
|
Brain connectivity disruption may explain poor social connection in PTSD patients
 Image: ©iStock/Naeblys (05/20/2021)
Poor social connection in people with PTSD may be related to abnormalities in brain structure, found a White River Junction VA study. Researchers looked at 31 participants with PTSD and 21 controls with trauma exposure but no PTSD. The PTSD group reported smaller social networks and greater loneliness. The researchers used magnetic resonance imaging (MRI) while participants performed a memory task involving social relationships. Imaging of the PTSD group during the memory task showed hyperactivation of the default network, the connection between different parts of the brain. MRI also revealed less functional connectivity between specific brain systems in the PTSD group. The results suggest that poor social connection in people with PTSD could be caused by disrupted brain connectivity, according to the researchers. (Depression and Anxiety, Feb. 23, 2021)
|
Cognitive behavioral therapy beneficial for dementia patients
 Photo: ©iStock/Enes Evren (05/20/2021)
Cognitive behavioral therapy could improve mood and insomnia in people with dementia, found a review by Michael E. DeBakey VA Medical Center researchers and colleagues. Cognitive behavioral therapy aims to improve mental distress by helping a person modify and control their thought processes. Researchers reviewed the available evidence on this approach for people with mild cognitive impairment and dementia. Multiple studies showed that cognitive behavioral therapy can improve anxiety, depression, and quality of life in these patients. Some evidence also suggests that the therapy can reduce insomnia and improve sleep quality. The results show a need for more study on cognitive behavioral therapy in dementia patients, especially with regard to insomnia, say the researchers. (Alzheimer’s Disease and Associated Disorders, April 28, 2021)
|
High blood pressure could cause peripheral artery disease
 Photo: ©iStock/Ivan-balvan (05/20/2021)
Higher blood pressure is likely to cause peripheral artery disease, according to a study by VA researchers and colleagues. In peripheral artery disease, narrowed arteries reduce blood flow to the limbs. Researchers looked at genome-wide study data on blood pressure and cardiovascular disease. They found that higher pulse pressure and mean arterial pressure directly increase the risk of peripheral artery disease. Use of blood pressure medications such as beta-blockers and diuretics was linked to lower risk of peripheral artery disease. This suggests that medications that lower blood pressure protect against the disease. More research is needed to clarify how exactly blood pressure influences peripheral artery disease, say the researchers. (Arteriosclerosis, Thrombosis, and Vascular Biology, April 15, 2021)
|
Comparing different forms of transcranial magnetic stimulation
 Photo: ©iStock/Henrik5000 (05/11/2021)
One form of transcranial magnetic stimulation may be better than another method at treating PTSD and depression, found a Providence VA study. In TMS, magnetic pulses are applied to the outside of the head to influence the electrical signals in the brain. It has been shown to help with both PTSD and major depressive disorder. The researchers compared two types of TMS, 5 Hz TMS and intermittent theta burst stimulation (iTMS), in 10 Veterans each with PTSD and depression. The treatments are similar but use different frequencies and duration. Both methods were safe and reduced PTSD and depression symptoms. However, Veterans who received iTMS reported poorer outcomes. Separate studies of iTMS showed similar outcomes to 5 Hz TMS when the iTMS exposure time was longer. The results could help clinicians choose the best form of TMS for their patients, say the researchers. (Journal of Traumatic Stress, May 11, 2021)
|
Gene therapy could prevent learning and memory loss from Alzheimer’s disease
 Photo: ©iStock/Evgenyi_Eg (05/11/2021)
VA San Diego researchers and colleagues used gene therapy to prevent learning and memory loss in a mouse model of Alzheimer’s disease. The researchers introduced a compound called AAV-SynCav1—a protein that can potentially activate mechanisms to prevent structural damage in the brain—into the hippocampus brain region of mice with deficits similar to Alzheimer’s. The hippocampus is one of the first parts of the brain affected by Alzheimer’s. At nine and 11 months after treatment, hippocampus-related learning and memory were preserved. Important membrane structures and receptors also remained intact in the treated mice, while control mice had damage. The results show the treatment has potential to restore brain plasticity and improve function in humans with Alzheimer’s, according to the researchers. (Molecular Therapy, March 29, 2021)
|
Cannabis use disorder linked to aggression
 Photo: ©iStock/Olga Novikova (05/11/2021)
Cannabis use disorder and aggression appear to be linked, according to a Durham VA study. Cannabis use disorder refers to addiction to the substance and negative social impacts of excessive use. Evidence suggests that some Veterans attempt to self-medicate with cannabis for conditions such as PTSD. The researchers studied cannabis use and psychological factors for more than 3,000 Iraq/Afghanistan-era Veterans. They found that cannabis use disorder was associated with increased odds of difficulty managing anger, aggressive impulses, and problems controlling violence. The study could not determine whether cannabis use disorder causes aggression, or whether people with more aggressive tendencies were more likely to develop the disorder. The results show a need to assess violent tendencies along with cannabis use disorder, say the researchers. (Journal of Psychiatric Research, April 22, 2021)
|
Combined PTSD, substance use disorder lead to worse social well-being
 Photo: ©iStock/PeopleImages (04/27/2021)
Veterans with both PTSD and substance use disorder face significant social problems, found a Durham VA study. Researchers analyzed data on social functioning for more than 1,000 Veterans. Those with both PTSD and SUD were particularly likely to experience homelessness, violent behavior, and suicidal behavior. Veterans with both conditions were more likely to report worse social well-being, compared to those with only PTSD, only SUD, or neither disorder. Veterans with both conditions were also more likely to have worse job and financial well-being. The findings suggest that multiple aspects of well-being should be assessed together in Veterans with PTSD and SUD, according to the researchers. (Psychological Trauma, March 4, 2021)
|
Cognitive and motor performance linked in stroke recovery
 Image: ©iStock/peterschreiber.media (04/27/2021)
Cognitive function affects physical motor performance after stroke, according to a study by Providence VA researchers and colleagues. The study assessed how 50 patients recovering from stroke did on two arm movement tasks. Patients performed worse on the more cognitively demanding task, especially immediately after their strokes. Poorer performance on the more complex test was linked to broad injury beyond the parts of the brain involved with movement, while performance on the simpler task was mostly linked to injury of the brain regions related to motor function. The results show that motor ability and cognitive function must be considered together when treating stroke patients, say the researchers. (Neurology, April 15, 2021)
|
Transportation an important barrier to colorectal cancer care
 Photo: ©iStock/Kichigin (04/27/2021)
Transportation is an important barrier to colorectal cancer care, found a study by Durham VA researchers. Researchers surveyed 115 Veterans with colorectal cancer. Of those, 18% said they had transportation barriers that made accessing care difficult. Their distance from a VA facility was not strongly linked to transportation difficulty. Rather, a chaotic lifestyle was the largest cause of transportation barriers. Chaotic lifestyle mainly means that patients have an unpredictable schedule. Identifying Veterans with chaotic lifestyles could allow for timely intervention to improve their cancer care, say the researchers. (BMC Health Services Research, April 13, 2021)
|
COVID-19 ‘long-haulers’ face increased risk of death and many other health problems
 Photo: ©iStock/MilosStankovic (04/26/2021)
A large VA study showed that people who have had COVID-19 are at heightened risk of both death and many other health problems. In the largest post-acute COVID-19 study to date, VA Saint Louis Health Care System researchers characterized many potential long-term consequences of COVID-19. The researchers looked at outcomes on more than 73,000 VA patients who survived COVID-19 and close to 5 million who did not contract the disease. The COVID-19 group had a higher risk of dying six months after diagnosis. People who have recovered from COVID-19 also are at increased risk of health problems affecting virtually every organ system in the body, not just the lungs. About 8% to 10% of people affected by COVID-19 will likely have long-term effects, according to the researchers. (Nature, April 22, 2021)
|
Inflammation linked to Alzheimer’s disease risk
 Photo: ©iStock/digicomphoto (04/21/2021)
Inflammation in the brain is linked to greater Alzheimer’s disease risk, found a VA San Diego study. Researchers analyzed the cerebrospinal fluid and performed cognitive testing on 81 cognitively normal older adults and 137 with mild cognitive impairment. In the cognitive impairment group, those with biomarkers for vascular inflammation also had increased levels of tau proteins, which have been linked to Alzheimer’s. Higher levels of tau protein were associated with poorer memory performance in the cognitive impairment group only. However, in the cognitively normal group, participants with lower pulse pressure who had greater inflammation showed signs of lower burden of amyloid-beta, an amino acid also linked to Alzheimer’s. The findings suggest that pulse pressure and inflammation have a complex effect on markers of Alzheimer’s disease, say the researchers. (Journal of Alzheimer’s Disease, March 4, 2021)
|
Non-suicidal self-injury linked to suicide attempts
 Photo: ©iStock/ligonpix (04/21/2021)
Non-suicidal self-injury disorder is strongly linked to suicide attempts among Veterans, found a study by Durham VA researchers and colleagues. The study looked at more than 100 Veterans with at least one mental health disorder. Forty-eight percent had a diagnosis of non-suicidal self-injury disorder. Suicide attempts were reported in 28% of the participants. Those with non-suicidal self-injury disorder were nearly five times more likely to have a suicide attempt than those without. The results show that understanding the link between self-injury and suicide could improve prevention, say the researchers. (Journal of Affective Disorders, March 15, 2021)
|
Older adults show low physical activity in and out of nursing facilities
 Photo: ©iStock/Dean Mitchell (04/21/2021)
Older adults in skilled nursing facilities showed low physical activity both during and after their stays, according to a study led by an Eastern Colorado VA researcher. The study followed patients during the last few days of their stay at a skilled nursing facility and a few days after discharge. Participants spent a median of 12% of their time in the facility and 17% at home standing upright. The number of steps taken per day was very low and did not increase much when patients returned home. Patients thought that they were more physically active than they actually were. The results highlight the need to encourage physical activity both in and out of skilled nursing facilities, say the researchers. (Disability and Rehabilitation, April 9, 2021)
|
Higher risk of suicidal thoughts in American Indian, Alaska Native Veterans
 Photo: ©iStock/grandriver (04/14/2021)
American Indian and Alaska Native (AI/AN) Veterans have more than twice the risk of suicidal thoughts compared to white Veterans, found a VA Salt Lake City study. Researchers looked at data from two large national surveys. In the Behavioral Risk Factor Surveillance System, 9.1% of AI/AN Veterans reported suicidal thoughts, compared with 3.5% of white Veterans. In the National Survey on Drug Use and Health, 8.9% of AI/AN Veterans reported suicidal thoughts, compared with 3.7% of white Veterans. Suicide prevention efforts in collaboration with these communities are needed, conclude the researchers. (Military Psychology, April 8, 2021)
|
Veterans open to firearms safety discussions in primary care to prevent suicides
 Photo: ©iStock/KarenMower (04/14/2021)
Veterans are open to discussing firearms safety in primary care, according to a study by VA Portland researchers and colleagues. More than half of Veterans who die by suicide visit their primary care provider a month before their death. The researchers surveyed 27 Veterans with depression and PTSD. All participants received health care through VA. The majority felt that discussing firearms safety was acceptable and needed, even if discussions were uncomfortable. They cited the urgent need to prevent Veteran suicide for this feeling. The Veterans identified the need for providers to be transparent in their reasons for asking about firearms and to respect Veterans’ unique relationships with firearms. The findings show that a Veteran-focused approach to firearms safety could help address Veteran suicide, say the researchers. (Journal of the American Board of Family Medicine, March–April 2021)
|
PTSD symptoms linked to unhealthy diet
 Photo: ©iStock/wildpixel (04/14/2021)
Veterans with PTSD symptoms often have a more unhealthy diet than those without PTSD, found a VA National Center for PTSD study. Researchers assessed more than 800 Veterans twice during a three-year period. They found that trauma exposure directly predicted diet quality. Participants with greater PTSD symptoms at baseline were more likely to have a poor diet, compared to those without PTSD symptoms. The findings suggest that consuming unhealthy food was driven by emotional suppression. The researchers did not find any link between PTSD symptoms and amount of exercise. The results could help treat medical comorbidities in patients with PTSD, say the researchers. (European Journal of Psychotraumatology, March 2021)
|
Feelings of anger often lead to self-injury
 Photo: ©iStock/ananaline (04/06/2021)
Feelings of anger and hostility often lead to self-injury, found a study by Durham VA researchers. Forty Veterans diagnosed with nonsuicidal self-injury disorder completed an electronic diary for 28 days. During the time period, 9% of participants reported self-injury, and 19% said they had the urge to self-injure. The most common type of self-injury was punching walls or objects. Momentary feelings of anger or hostility were linked to subsequent self-injury urges. The reverse was not true: self-injury did not lead to feelings of anger. The results highlight the need to assess and treat patients who self-injure for anger issues, say the researchers. (Journal of Psychiatric Research, March 2021)
|
Stem cell therapy offers potential treatment for ischemia
 Image: ©iStock/luismmolina (04/06/2021)
Stem cells may be an effective treatment for life-threatening ischemia, according to a mouse study led by a VA Connecticut researcher. Ischemia is when an organ does not get enough blood, which can cause serious organ problems. Researchers treated ischemic mice with smooth muscle cells derived from pluripotent stem cells that had been grown in a lab. Pluripotent stem cells are base cells that can be reprogramed to form into different types of body cells. Treated mice had improved functional outcomes and blood flow, compared with controls. They also showed signs of improved wound healing. The results show that stem-cell therapy has potential to effectively treat ischemia in humans, say the researchers. (Cells, April 2, 2021)
|
Peer-led program leads to better Veteran engagement and well-being
 Photo: ©iStock/Georgijevic (04/06/2021)
A peer-led program resulted in greater Veteran health care engagement and well-being, found a study by VA Bedford researchers and colleagues. Forty-eight Veterans took part in a group-led VA program called Taking Charge of My Life and Health. The nine-week program used peer support to improve patient engagement and health by teaching whole health concepts and strategies. Participants had a significant decrease in perceived stress. They also showed significant improvements in mental health and quality of life. Patients were more engaged with their health care after the program. The findings suggest that using peers to guide patients in exploring their values and goals can improve their health and engagement, say the researchers. (Journal of Alternative and Complementary Medicine, March 2021)
|
Black patients face credibility bias
 Photo for illustrative purposes only. ©iStock/monkeybusinessimages (03/31/2021)
Black patients may face systemic bias in physicians’ perceptions of their credibility, according to a study that included a VA Portland researcher. The researchers identified three linguistic features that may indicate disbelief in medical notes: putting patient statements in quotation marks, using judgment words such as “claims” or “insists,” and reporting patients’ symptoms and experiences as hearsay. They then used machine learning to look for these features in more than 9,000 medical notes. Notes written about Black patients were more likely to contain all three signs of disbelief, compared with notes on white patients. Notes about female patients were more likely than male patient notes to contain quotes. The results suggest that Black patients are less likely to be believed when they describe their symptoms or experiences, say the researchers. (Journal of General Internal Medicine, March 22, 2021)
|
Challenges of providing telehealth care
 Photo: ©iStock/nensuria (03/31/2021)
A study of VA nurse practitioners and patients identified challenges of using telehealth for care. Nurses identified several logistical problems that made providing care over video more difficult. They noted the complexity of scheduling appointments, local barriers to care, and difficulty of remotely managing acutely ill patients. The nurses surveyed also said that it is harder to gather sensory data during remote visits. Video makes it harder to build provider-patient relationships, as well. Patients were aware of the limitations on physical exams but not the logistical challenges. Training videos and mentoring on best practices could improve the telehealth experience, according to the researchers. (Journal of Nurse Practitioners, March 20, 2021)
|
Process behind kidney stone formation
 Image: ©iStock/wildpixel (03/31/2021)
Researchers with the VA Calcium Signaling Laboratory explored how a disease called acidosis can lead to the formation of kidney stones. A region of the kidney called the proximal tubule helps control the acid-base balance in the blood. Acidosis is when acids are not properly removed from the blood into the urine by the proximal tubule. In addition to causing problems with the blood, acidosis causes the urine to become more alkaline. The researchers used a mouse model of this condition to study how this shift may lead to kidney stones. They found that the shift in urine pH causes a build-up of calcium ions, which may form into stones. Dysregulation of the proximal tubule can also cause cell damage, which further leads to stone formation when damaged cellular fragments bind with calcium crystals. The results improve the understanding of the biological processes behind kidney stones, say the researchers. (International Journal of Molecular Sciences, March 17, 2021)
|
Mild traumatic brain injury and PTSD frequently occur together
 Photo: ©iStock/SDI Productions (03/23/2021)
Mild traumatic brain injury and PTSD are strongly linked in Veterans, according to a VA study. Researchers assessed more than 1,500 former and current military personnel with a history of combat exposure. Eighty-two percent had a history of mild TBI. Of those, 41% also screened positive for PTSD. Only 24% of participants without a history of TBI had PTSD. Mild TBI was a good predictor of more severe neurological symptoms related to PTSD. The results suggest that TBI and PTSD should be evaluated and treated together in Veterans and service members who experienced combat, say the researchers. (Journal of Head Trauma Rehabilitation, Feb. 22, 2021)
|
Morphine could improve heart function in diabetic patients
 Photo: ©iStock/Hailshadow (03/23/2021)
Morphine could help restore heart function damaged by diabetes, found a study by VA San Diego researchers. Diabetes can increase the risk of serious heart problems, largely through increased obesity risk. Opioids are known to aid in cardiac stress tolerance, but diabetes disrupts how the body responds to opioids. The researchers tested a five-day, high-dose morphine treatment in a mouse model of type 2 diabetes. The treatment improved blood pressure stability, reversed cardiac depression, and improved heart function. It also restored impaired molecular heart processes. The findings suggest that short-term, high-dose morphine could help diabetic patients recover from acute cardiovascular events, say the researchers. (FASEB J, March 2021)
|
Addiction possibly linked to brain asymmetry
 Photo: ©iStock/CasarsaGuru (03/23/2021)
Addiction may be linked to brain asymmetry, found a large international study that included a VA San Diego researcher. The researchers analyzed brain scans of nearly 1,800 patients who were dependent on alcohol, nicotine, cocaine, methamphetamine, or cannabis. They compared them to scans of almost 1,000 patients without substance dependence. The results showed that addiction was significantly linked to asymmetry of the nucleus accumbens, a region in the lower middle of the brain. The right side of the nucleus accumbens was smaller in patients with substance dependence. This effect was largest in patients with alcohol and nicotine dependence. More research is needed on whether substance use causes the brain asymmetry, or whether the asymmetry increases the risk of addiction, according to the researchers. (Addiction Biology, Jan. 28, 2021)
|
Increasing physical distance in schools not linked to fewer COVID-19 cases
 Photo: ©iStock/izusek (03/17/2021)
Maintaining three feet versus six feet of physical distance between students did not affect COVID-19 case rates, found a study by VA Boston researchers and colleagues. Researchers looked at COVID-19 infection data for nearly 540,000 students and more than 99,000 staff attending in-person schools in the Massachusetts public school system. They found that the infection rate was similar in districts with policies requiring three feet of physical distance, compared with districts requiring six feet. Increasing physical distance may not be necessary to prevent COVID-19 cases in schools, concluded the researchers, provided that universal mask mandates and other precautions are implemented. (Clinical Infectious Diseases, March 10, 2021)
|
Moral injury increases Veteran suicide risk
 Photo: ©iStock/Drazen Zigic (03/17/2021)
Morally injurious experiences are linked to increased risk of suicidal behavior, found a VA study of more than 1,000 Veterans. Moral injury experienced during deployment includes perpetrating, failing to prevent, witnessing, or learning about acts that transgress deeply held moral beliefs. Of the Veterans surveyed, 36% had at least one morally injurious experience. Reports of transgressions by others and feelings of betrayal were more common than personal transgressions. These experiences were linked with a higher risk of suicidal thoughts, making a suicide plan, and suicide attempts. While the effect of moral injury on suicidal behavior was significant, PTSD and depression had greater effects on suicide risk. The results show that more work to evaluate and address moral injury in Veterans is needed, say the researchers. (Depression and Anxiety, March 5, 2021)
|
Rural Veterans may have less access to lung cancer screenings
 Photo: ©iStock/mustafagull (03/17/2021)
Access to lung cancer screening varies widely based on location in the Veterans Health Administration, found a study by VA Bedford researchers. The researchers looked at data on screening exams at VA facilities and partner sites over a six-year period. They found that screening numbers varied by more than 30-fold across different regions. Screenings were particularly low in more rural locations. Nine of the 12 states with the highest proportions of rural Veterans had three or fewer lung cancer screening facilities. The findings indicate that VA needs to make efforts to provide more equitable access to lung cancer screening, according to the researchers. (Chest, Feb. 19, 2021)
|
Meditation program may reduce nursing burnout
 Photo: ©iStock/insta_photos (03/09/2021)
An online mantram meditation program could help nurses with stress management and lead to improved patient care, according to a Edward Hines, Jr. VA Hospital study. Nurses often experience high levels of stress and burnout, which has been exacerbated by the COVID-19 pandemic. Registered nurses working in VA acute care units participated in an online mantram repetition program to learn stress coping skills. The program involved repeating a spiritually meaningful word or phrase, called a mantram, to slow down one’s thoughts and refocus. Nurses who participated in the program reported increased mindfulness, spiritual well-being, and presence while with patients. They also experienced less burnout. Patients being treated by participating nurses noticed greater levels of presence from nurses and were highly satisfied with their care. The results suggest that portable stress reduction techniques can help alleviate nursing burnout, say the researchers. (Nursing Outlook, Feb. 8, 2021)
|
Traumatic brain injury increases sleep disorder risk
 Photo: ©iStock/amenic181 (03/09/2021)
Veterans with traumatic brain injury have an increased risk of developing sleep disorders, found a study by San Francisco VA researchers. The study included data from nearly 200,000 Veterans over a 14-year period. Veterans who had a TBI were 41% more likely to develop a sleep disorder, compared with Veterans with no TBI history. The association between sleep disorders and TBI was most common in mild TBIs, or concussions. Sleep disorders seen in this population included sleep apnea, insomnia, excessive sleepiness during the day, and sleep-related movement disorders. The findings show that better prevention and long-term management for sleep are needed for Veterans with TBI, say the researchers. (Neurology, March 3, 2021)
|
MRI could help detect early Alzheimer’s
 Photo: ©iStock/utah778 (03/09/2021)
Magnetic resonance imaging (MRI) of the locus coeruleus brain region could aid in early detection of Alzheimer’s disease, according to a study of Vietnam-era male Veterans. The locus coeruleus is a structure in the brainstem involved in the sleep-wake cycle and in cognitive function. It is known to undergo extensive degeneration during Alzheimer’s progression. Researchers assessed cognitive function and MRI scans in nearly 500 older Veterans. They found that reduced locus coeruleus integrity was linked to sleep dysfunction, poorer memory, and greater odds of mild cognitive impairment. The results suggest that assessing locus coeruleus structural integrity with MRI could be used as an early measure of Alzheimer’s risk, according to the researchers. (Alzheimer’s and Dementia, Feb. 13, 2021)
|
Height loss linked to higher hip fracture risk in older men
 Photo: ©iStock/RealPeopleGroup (03/03/2021)
Height loss in elderly men is associated with a higher risk of hip fracture, found a study by Minneapolis VA researchers and colleagues. Losing height is common in older adults as age-related changes in the bones, muscles, and joints occur. The researchers studied a sample of nearly 3,500 older men. They found that men who had lost at least three centimeters in height over a period of seven years had nearly double the risk of a hip fracture, compared with those who lost less than a centimeter in height. Men who lost at least three centimeters had an 11.6% chance of a hip fracture. Those losing less than a centimeter had a 2.7% chance of hip fracture. The risk of other bone fractures was also higher in men who had lost height. The results suggest that height loss should be considered when assessing fracture risk, say the researchers. (Journal of Bone and Mineral Research, Feb. 22, 2021)
|
Simulating feeling in amputated feet
 Photo: ©iStock/xavierarnau (03/03/2021)
Researchers with the VA Advanced Platform Technology Center were able to simulate foot sensations in patients with lower-limb amputations using electrodes. People with lower-limb amputation often experience postural instability because of missing sensory information from the foot. Researchers simulated sensation in patients missing a foot due to amputation during standing using implanted electrodes. They compared the patients’ reactions to how they reacted to vibrations felt in the intact foot. Participants adjusted their posture in much the same way in both situations. This told the researchers that the participants perceived the electrical stimulation as if it were coming from the missing foot. The results could lead to using electrical stimulation to provide sensory feedback when walking with a leg prosthesis and improve gait stability, according to the researchers. (Frontiers in Neuroscience, Feb. 18, 2021)
|
Kidney transplant patients have lower risk of death when receiving VA care
 Image: ©iStock/peterschreiber.media (03/03/2021)
Risk of death after a kidney transplant was significantly lower in patients whose post-surgery care was through VA, compared to those cared for outside VA, found a study by VA Pittsburgh researchers. The study focused on data from over 6,000 Veterans enrolled in both VA health care and Medicare. Of those, 16% had a kidney transplant at a VA hospital. Out of all kidney transplant patients, 12% received their post-transplant care from VA only, while 34% received care only at non-VA hospitals through Medicare. The remaining 54% used both VA and non-VA care. Patients who used only non-VA post-transplant care were more than twice as likely to die within five years of their surgery, compared with patients who used VA only. Compared with VA-only patients, patients who used both VA and Medicare were 1.5 times more likely to die within five years. The results show the need to monitor patient outcomes for Veterans receiving care outside VA, say the researchers. (Clinical Journal of the American Society of Nephrology, Feb. 18, 2021)
|
Quitting smoking linked to less pain
 Photo: ©iStock/Sezeryadigar (02/23/2021)
Quitting smoking was linked to significantly lower pain levels, in a VA study. Researchers studied data on nearly 2,000 Veterans who smoked an average of 15 cigarettes a day and had chronic pain. Participants were involved in a program of proactive outreach to help them quit smoking. At six and 12 months after the program, researchers asked participants whether they had smoked in the last seven days. Participants at all pain levels who had stopped smoking had significantly less pain at the six-month check-in. After 12 months, participants with severe pain had lower pain. The results show that abstinence from smoking may lower pain levels, according to the researchers. (Pain Medicine, Jan. 27, 2021)
|
Transgender Veterans at high risk of suicide
 Photo: ©iStock/AlxeyPnferov (02/23/2021)
Transgender Veterans are at an elevated risk of suicide, found a study of more than 32,000 Veterans. Researchers assessed VA data from a 17-year period. They found that transgender patients had more than twice the risk of suicide, compared with cisgender patients—those whose gender identity matches their sex assigned at birth. This difference was especially pronounced among younger (18-39 years) and older (65 and older) patients. Overall, transgender patients had slightly lower risk of death from any cause, compared with cisgender patients. The results highlight an urgent need for more efforts to prevent suicide among transgender patients, say the researchers. (LGBT Health, Feb. 5, 2021)
|
Secure messaging changes how Veterans access health care
 Photo: ©iStock/katleho Seisa (02/23/2021)
Secure messaging decreased in-person health care visits and increased telephone visits, according to a study of VA health care use. Secure messaging allows patients and health care providers to send messages back and forth online while protecting patient information. Researchers looked at how use of secure messaging on VA’s MyHealtheVet patient portal affected health care usage in 2016. In-person health care visits decreased by 16% for secure messaging users and 10% for users who did not use secure messaging. Telephone visits increased by 11% for secure messaging users and 7% for non-users. The results show that secure messaging could improve clinic appointment availability, say the researchers. They also point out that secure messaging will likely increase providers’ time commitments for not-traditional forms of access. (Journal of General Internal Medicine, Feb. 2, 2021)
|
Anticoagulants could lower COVID-19 mortality risk
 Photo: ©iStock/kovop58 (02/16/2021)
Anticoagulation medication could lower the risk of death from COVID-19, according to a study by VA researcher and colleagues. The study looked at data on more than 4,000 patients hospitalized with COVID-19. Most of the patients were given medication to prevent blood clots. Results show that patients given the medication had a 27% lower risk of dying from COVID-19 within 30 days of hospitalization, compared with patients not receiving anticoagulants. Anticoagulant use was not associated with serious bleeding events. The findings provide strong evidence for the use of anticoagulants as an initial treatment for COVID-19, say the researchers. (BMJ, Feb. 11, 2021)
|
Recovery needs after suicide attempt vary by gender
 Photo: ©iStock/Marjan_Apostolovic (02/16/2021)
Men and women have different needs when recovering from a suicide attempt, found a study by VA Portland researchers and colleagues. Researchers interviewed 25 female and 25 male Veterans who had attempted suicide but survived. When talking about their recovery needs, women focused on developing connections with others and wanting to increase their self-knowledge and self-worth. Men were more concerned with trying to live up to their ideal selves by living and doing “right.” Men also wanted to feel like they were needed by others. Both men and women said they wanted to feel a sense of purpose. The results suggest that patients who attempt suicide could benefit from gender-specific treatment approaches, according to the researchers. (Medical Care, Feb. 1, 2021)
|
Temporary financial assistance helps homeless Veterans find stable housing
 Photo: ©iStock/turk_stock_photographer (02/16/2021)
Temporary financial assistance increases the likelihood of homeless Veterans finding stable housing, found a VA study. Researchers looked at data on nearly 42,000 Veterans experiencing homelessness who were enrolled in the VA Supportive Services for Veteran Families program. About 70% of those Veterans received temporary financial assistance for housing-related expenses. In total, 81% of Veterans in the program achieved stable housing. Veterans who received financial assistance were significantly more likely to find stable housing. Receiving more financial assistance led to a greater chance of finding stable housing. The results suggest that providing temporary financial assistance may be an effective way to address Veteran homelessness, say the researchers. (JAMA Network Open, Feb. 1, 2021)
|
Unexpected or morally questionable combat experiences increase suicide risk
 Photo: ©iStock/Rockfinder (02/10/2021)
A study by VA Puget Sound researchers and colleagues identified specific combat experiences that may be linked with increased suicide risk in service members. Researchers looked at data on nearly 58,000 service members. Any combat exposure did not increase suicide risk. However, high combat severity and specific events were associated with the chance of suicide attempts. In particular, being attacked or ambushed, seeing dead bodies or human remains, and being directly responsible for the death of a noncombatant significantly increased a service member’s risk of suicide. This connection was often mediated by PTSD. The results suggest that clinicians should inquire about the nature of combat experiences when assessing service members for suicide risk, say the researchers. (JAMA Network Open, Feb. 1, 2021)
|
Back and neck pain common after upper-limb amputation
 Photo: ©iStock/Aleksej Sarifulin (02/10/2021)
Back and neck pain is common in Veterans with upper-limb amputations, found a Providence VA Medical Center study. People with an upper-limb amputation may experience back and neck pain because they change the way they move to compensate for the missing limb. Researchers evaluated nearly 800 Veterans with upper-limb amputation for pain. They found that 61% had back pain and 48% had neck pain. About 52% of respondents had both back and neck pain. Persistent pain was associated with lower quality of life. The findings show that additional pain prevention and intervention are needed in Veterans with amputation, according to the researchers. (American Journal of Physical Medicine and Rehabilitation, Jan. 11, 2021)
|
Bacteria immunization may improve stress response
 Image: ©iStock/wildpixel (02/10/2021)
Immunization with M. vaccae bacteria could improve the body’s response to stress, according to a study led by a VA Rocky Mountain MIRECC researcher. Mycobacterium vaccae is a bacterium derived from soil. It has been shown to have anti-inflammatory and immune regulation properties. Researchers immunized mice with M. vaccae to study its effects on the stress response. The bacterium stabilized the gut microbiome in the mice. This in turn led to a more proactive behavioral response to stress exposure through the connection between the gut and the brain. The immunization also appeared to promote stress resilience. The results suggest that M. vaccae could be used to improve negative reactions to stress. (Frontiers in Physiology, Jan. 5, 2021)
|
Veterans with ALS at high suicide risk
 Photo: ©iStock/shapecharge (02/02/2021)
Veterans with amyotrophic lateral sclerosis (ALS) are at high risk for suicide, according to a VA Rocky Mountain Mental Illness Research Education and Clinical Center study. ALS is a disease that affects nerve cells in the brain and spinal cord, causing muscle weakness and an increasing loss of function. There is no cure. Researchers looked at data on more than 7,000 Veterans with ALS and 1.5 million without. They found that Veterans with ALS had nearly four times higher risk of suicide. The most common means of suicide was with a firearm. The results show a need for additional efforts to prevent suicide in Veterans with ALS, according to the researchers. (Muscle and Nerve, Jan. 20, 2021)
|
Technology-based physical activity therapy for COPD cost-effective
 Photo: ©iStock/Antic Zlatko (02/02/2021)
A technology-based physical activity therapy is cost-effective for chronic obstructive pulmonary disease (COPD), found a VA study. Regular physical activity is recommended for patients with COPD. COPD patients were given either a pedometer alone, or a pedometer along with website-based support. The website provided goal-setting, feedback, motivation, and support. Researchers assessed cost-effectiveness by comparing cost per quality-adjusted life years, a measure of disease burden. Cost of both interventions fell below participants’ willingness to pay for better quality of life. The results show that a technology-based approach to physical activity can directly benefit COPD patients. (American Journal of Respiratory and Critical Care Medicine, Dec. 23, 2020)
|
Study: Shock waves can cause structural brain damage
 Image: ©iStock/4X-image (02/02/2021)
A study by VA researchers and colleagues using a mouse model provides new insights into how the brain is affected by shock waves from explosions. Researchers measured shock wave pressure and velocity during a simulated explosion experiment. The measurements will help researchers better understand how much force is absorbed by the brain during a shockwave. Mice exposed to low-intensity blasts showed signs of structural damage to the cells of the brain. Researchers found abnormalities in cell mitochondria, axons, and synapses. The findings provide new data on how blast exposure can cause traumatic brain injury, say the researchers. (Military Medicine, Jan. 25, 2021)
|
Identifying chronic cough with natural language processing
 Photo: ©iStock/AaronAmat (01/26/2021)
Natural language processing can identify chronic cough through patient records, found a study by a Richard L. Roudebush VA Medical Center researcher and colleagues. Chronic cough was defined as a cough lasting eight or more weeks. Chronic cough is difficult to identify in electronic health records because of incomplete diagnostic codes. Researchers used natural language processing, a form of machine learning that looks at written health care notes, to study more than 200,000 appointments. More than 20,000 of those patients had chronic cough. Natural language processing was able to identify chronic cough in 74% of these patients. Looking at diagnoses or prescriptions alone identified only 15% of chronic cough cases. Natural language processing could be a useful tool in treating unrecognized chronic coughs, according to the researchers. (Chest, Dec. 17, 2020)
|
Timed muscle stimulation makes wheelchair use easier
 Photo: ©iStock/ljubaphoto (01/26/2021)
Stimulating trunk and hip muscles at the right time can improve manual wheelchair propulsion, found a VA Advanced Platform Technology Center study. Researchers used an accelerometer attached to a manual wheelchair user’s wrist to time the two main phases of propulsion: contact and recovery. Using this data, they were able to time stimulation of trunk and hip muscles to assist in the movements. With properly timed stimulation, the wheelchair user had improved acceleration and reported that pushing the wheelchair was easier. The findings show that a simple accelerometer can detect wheelchair user movements. These measurements can improve muscle stimulation and make wheelchair use easier, say the researchers. (American Journal of Physical Medicine and Rehabilitation, Jan. 11, 2021)
|
Stepped care treatment model improves knee osteoarthritis
 Photo: ©iStock/thebigland88 (01/26/2021)
A stepped care model could be an effective way of delivering exercise therapy to patients with knee osteoarthritis, according to a Durham VA study. In a stepped care model, patients move through different steps if initial treatment is not effective. In the knee osteoarthritis program, step 1 is three months of an internet-based exercise program. If patients do not have pain improvement, they proceed to step 2, three months of biweekly physical activity coaching phone calls. Those who advance to step 3 receive in-person physical therapy visits. In a group of 230 patients, 65% progressed to step 2 and 35% progressed to step 3. After nine months, patients in the step program had modest improvements in knee osteoarthritis symptoms, compared to a control group. The results show that the stepped care model could be an efficient therapy method for osteoarthritis, say the researchers. (Annals of Internal Medicine, Dec. 29, 2020)
|
Potential new medication for treating COVID-19
 Photo: ©iStock/shunyufan (01/21/2021)
A team led by a Jesse Brown VA Medical Center researcher created a potential new medication to treat COVID-19. The virus behind COVID-19 binds with an enzyme in the body called ACE2, which allows it to enter human cells. The researchers designed a peptide (a chain of amino acids) that blocks ACE2 from binding with the spike proteins on the outside of the virus. They gave the new peptide to mice with symptoms that mimic COVID-19 as a nasal spray. The spray reduced fever, protected the lungs, and improved heart function and the mice’s movement. The results could lead to an important new treatment for COVID-19, according to the researchers. (Journal of Neuroimmune Pharmacology, Jan. 11, 2021)
|
Sleep coach program improves insomnia
 Photo: ©iStock/grandriver (01/21/2021)
A program combining cognitive behavioral therapy and positive airway pressure can improve insomnia, found a study by VA researchers and colleagues. Patients with both insomnia and obstructive sleep apnea participated in weekly sessions with a “sleep coach,” along with using a C-PAP machine. The sleep coach used cognitive behavioral therapy, a psychotherapy focused on dealing with distressful thoughts, to provide support on several sleep-related behaviors, such as stimulus control and relaxation techniques. A C-PAP uses air pressure to improve the user’s breathing during sleep. Patients receiving the coaching showed greater improvement in sleep quality, compared with a control group. They also more frequently used their C-PAP machines. The results show that the program can improve both C-PAP adherence and insomnia, say the researchers. (Sleep, Nov. 21, 2020)
|
Cognitive impairment common in homeless adults
 Photo: ©iStock/LordHenriVoton (01/21/2021)
Cognitive and functional impairments are common among homeless adults, found a study by VA San Diego researchers. One hundred participants staying at a homeless shelter completed a neurological assessment. Overall, 65% of participants had signs of cognitive impairment. About 30% had impaired processing speed, and 11% met the criteria for cognitive disability. Of the total sample, 48% were assessed with functional impairment, meaning cognitive problems made carrying out functions of their daily lives difficult. Poorer cognitive performance was linked to greater functional impairment. The results underscore the need for routine cognitive screening as part of homelessness services, say the researchers. (Psychiatric Services, Jan. 5, 2021)
|
Frailty increases the risk of death after surgery
 Photo: ©iStock/Satyrenko (01/14/2021)
Frailty raises the risk of death after most types of surgery, found a study by VA researchers. Frailty refers to increased vulnerability and weakness associated with aging. Researchers analyzed data on outcomes after surgery in nine non-cardiac specialties. They found that frail patients had a significantly higher risk of dying compared to non-frail patients, regardless of the type of surgery. This held true for low-intensity procedures such as plastic surgery, moderate-intensity surgeries such as neurosurgery, and high-intensity operations like vascular surgery. The results suggest that frailty should be assessed before surgery across all specialties, according to the researchers. (JAMA Surgery, Nov. 18, 2020)
|
Patients with kidney disease have mixed results on blood thinners
 Photo: ©iStock/Hailshadow (01/14/2021)
Beginning blood thinners for patients with kidney disease and atrial fibrillation has both benefits and problems, according to a study by Memphis VA Medical Center researchers and colleagues. Researchers looked at data on more than 22,000 Veterans with end-stage renal disease and atrial fibrillation (erratic heart beat) who began dialysis treatment. Patients with atrial fibrillation are often prescribed the blood thinner warfarin to prevent conditions like stroke, but its effect on dialysis is unknown. Warfarin use was linked to a higher risk of ischemia (lack of blood flow to an organ) and bleeding. However, patients taking warfarin had a lower risk of death than other patients. More study is needed to determine the net benefit of blood thinners in patients with kidney disease, say the researchers. (JACC Clinical Electrophysiology, Dec. 14, 2020)
|
Brain volume abnormalities linked to impulsive suicide attempts
 Photo: ©iStock/MachineHeadz (01/14/2021)
Impulsive suicide attempts are linked with abnormalities in the cingulate cortex of the brain, found a VA study. The cingulate cortex is a brain region known to be involved in inhibitions and impulsive behavior. Researchers conducted magnetic resonance imaging on the brains of 52 Veterans with either suicidal thoughts or attempts. They found that those who had attempted suicide had lower white matter volume in the cingulate cortex, compared with those who had suicidal thoughts but not attempts. Those with lower white matter volume also scored higher on an assessment of impulsivity. The results suggest that abnormalities in this part of the brain could lead to more unplanned suicide attempts, according to the researchers. (Journal of Affective Disorder, Dec. 3, 2020)
|
Disadvantaged patients less likely to receive flu shots
 Photo: ©iStock/annebaek (01/06/2021)
Socioeconomic factors can predict the likelihood of flu vaccination in patients with diabetes, found a study including a Michael E. DeBakey VA Medical Center researcher. The study looked at data on more than 25,000 patients with diabetes. About 36% of those did not receive a flu shot. Younger age, Black race, being uninsured, and having no usual source of health care all decreased the odds of getting a flu shot. Nearly 64% of patients with all four of these socioeconomic factors did not receive a flu shot. The findings highlight the need to increase vaccine coverage in disadvantaged communities, say the researchers. (Journal of the Endocrine Society, Sept. 24, 2020)
|
Nerve stimulation may improve cognitive performance
 Illustration: ©iStock/sankalpmaya (01/06/2021)
Stimulating the vagus nerve may improve cognitive performance, found a study by VA San Diego researchers. The vagus nerve is a large nerve connected to the brain. It is involved with controlling the heart, lungs, and digestive tract. The researchers stimulated the nerve from outside the body using electrical current in 15 subjects, who then performed cognitive tests. Compared with participants who did not receive nerve stimulation, the subjects had higher accuracy on both easy and hard mental reasoning tests. The researchers hypothesize that stimulating the vagus nerve could increase attention, thereby enhancing cognitive function. The results suggest that vagus stimulation could be a low-risk, low-cost treatment for cognitive disorders, according to the researchers. (Neuromodulation, Nov. 25, 2020)
|
Higher suicide risk in sexual minority Veterans
 Photo: ©iStock/Srdjanns74 (01/06/2021)
Suicide rates are high in sexual minority Veterans, according to a VA Salt Lake City study. Researchers looked at data on more than 8 million Veterans for an 18-year period. They found that risk of death from suicide was four times higher in sexual minority Veterans, compared with the general population. Sexual minority Veterans had more than twice the risk of death by suicide than the general Veteran population. Sexual minority was defined as identifying as gay, lesbian, bisexual, or other sexual orientations not heterosexual. In 2017, suicide was the fifth-leading cause of death in sexual minority Veterans. For both men and women Veterans belonging to a sexual minority, suicide was the most common cause of death for 18- to 20-year olds. The most common method of suicide for this group was by firearm, used in 40% of deaths. The results suggest that more attention to suicide prevention is needed in this population, say the researchers. (JAMA Network Open, Dec. 1, 2020)
|
Lab study sheds light on insomnia caused by alcohol withdrawal
 Photo: ©iStock/1281086710.jpg (12/22/2020)
Researchers at the Harry S. Truman Memorial Veterans’ Hospital found the possible cause of alcohol withdrawal-related insomnia, using a mouse model. Insomnia is the most common symptom of alcohol withdrawal. However, why alcohol withdrawal causes insomnia is not known. In the study, mice exposed to chronic alcohol had severe insomnia-like symptoms, similar to those in humans with alcohol use disorder. During seven days of alcohol withdrawal, the mice had a significant reduction in a chemical process called histone acetylation in several parts of the brain. This process allows histones (a type of protein) to regulate gene expression. Giving the mice a chemical compound called Trichostatin A, which aids in histone acetylation, reduced insomnia symptoms. The results could explain how alcohol withdrawal causes insomnia and lead to better treatment, say the researchers. (Neuropharmacology, Dec. 1, 2020)
|
Veterans homeless services use reduces death by suicide
 Photo: ©iStock/AleksandarGeorgiev (12/22/2020)
Use of homeless services by Veterans significantly lowered the risk of death, including from suicide, according to a study by the VA National Center of Homelessness among Veterans. Researchers studied data on almost 170,000 Veterans who reported housing instability between 2012 and 2016. More than half of the Veterans studies accessed VA homeless services, such as emergency housing or work therapy programs. Those who used these services had a 6% reduction in the risk of death from any cause, compared with those not using the services. Veterans who accessed VA homeless services had a 21% lower risk of dying by suicide. The results show that social programs that address homelessness can be an important method to prevent Veteran suicide, according to the researchers. (Journal of Epidemiology and Community Health, Nov. 18, 2020)
|
Higher rates of drug use disorder among transgender patients
 Photo: ©iStock/Atiwat Studio (12/22/2020)
Transgender VA patients have increased odds of having drug use disorders, found a VA Puget Sound study. Researchers looked at data on nearly 9 million VA patients, more than 8,000 of whom were transgender. Transgender patients had a 67% higher likelihood of having any drug use disorder, compared with cisgender patients. The difference was highest for amphetamine use. The presence of mental health conditions did not affect the disparity in drug use disorder rates. The results point to a need for more research into health disparities for transgender patients, say the researchers, particularly toward potential barriers to substance use treatment. (Journal of Addiction Medicine, Nov. 25, 2020)
|
Nurses at higher risk of COVID-19 than other health care workers
 Photo: ©iStock/FG Trade (12/16/2020)
Nurses are more likely than other health care workers to test positive for the virus causing COVID-19, found a study including an Edward Hines, Jr. VA Hospital researcher. Researchers looked at COVID-19 test data for more than 6,500 health care workers. Nearly 2,000 of those were nurses. About 5% tested positive for the virus. Nurses had nearly twice the odds of testing positive, compared with other health care workers. Administrators who worked in hospitals but did not interact with patients were the least likely to test positive. Nurses who saw patients receiving high-flow oxygen therapy had a 45% higher risk of contracting the virus, and those treating patients receiving kidney dialysis had 57% higher odds, compared with other nurses. The results show that health care workers who spend more time around COVID-19 patients, such as nurses, are at increased risk from the virus, say the researchers. (Open Forum Infectious Disease, Dec. 9, 2020)
|
Number of concussions does not affect cognitive treatment response
 Photo: ©iStock/TefiM (12/16/2020)
The number of concussions one sustains does not affect treatment response, according to a study of service members with a history of brain injury. Participants underwent six weeks of cognitive rehabilitation for traumatic brain injury. All patients in the study improved in cognitive deficits and psychological distress over the course of treatment. Participants who had more concussions showed about the same level of improvement as those with fewer concussions. Participants with more concussions did report more cognitive difficulties both before and after treatment. The results show that cognitive rehabilitation is effective regardless of the number of concussions sustained, say the researchers. (Archives of Clinical Neuropsychology, Dec. 3, 2020)
|
Psychiatric conditions not linked to worse nicotine withdrawal
 Photo: ©iStock/Juanmonino (12/16/2020)
Patients with PTSD or depression had less increase in nicotine withdrawal symptoms than those without psychiatric conditions, in a study of Veterans who smoked. Smokers with psychiatric disorders often have increased trouble quitting. Researchers measured smokers’ nicotine withdrawal symptoms both before and during a two-day period without nicotine. Contrary to what the researchers expected, those without psychiatric conditions had greater increases in withdrawal symptoms when deprived of nicotine. The researchers suggest that high levels of distress and craving, not increased withdrawal symptoms, may account for the difficulties people with psychiatric conditions have to quit smoking. (Nicotine and Tobacco Research, Nov. 27, 2020)
|
Race-based COVID-19 disparities
 Photo: ©iStock/JONGHO SHIN (12/10/2020)
African American and Hispanic populations have higher rates of COVID-19 infection and death compared with other ethnic groups, according to a VA Portland review. Researchers reviewed 37 studies on COVID-19 data. They found that African American and Hispanic patients had disproportionately higher rates of virus infection, hospitalization, and death from COVID-19, compared with white patients. While these groups had a higher proportion of deaths from COVID-19, they did not show a higher risk of death in confirmed COVID-19 cases. Asian patients had similar COVID-19 rates as white patients. Not enough data exist on other racial groups to draw conclusions. The higher COVID-19 rates appear to be due to differences in health care access and exposure risk rather than any biological disposition, according to the researchers. (Annals of Internal Medicine, Dec. 1, 2020)
|
Post-traumatic headaches are often more complex than non-traumatic headaches
 Photo: ©iStock/Nenad Cavoski (12/10/2020)
Headaches caused by traumatic brain injury usually include more symptom features than non-traumatic headaches, found a study by VA researchers and colleagues. Headaches are a common symptom of mild traumatic brain injury. Researchers assessed more than 1,000 soldiers for different headache features, such as pain level, pulsating sensation, and visual auras. Soldiers with post-traumatic headaches were more likely to have all 12 headache features assessed, compared with soldiers with headaches but no traumatic brain injury. Unsurprisingly, soldiers who experienced a wider variety of headache symptoms, termed headache complexity, were more likely to use health care services. The results suggest that post-traumatic headaches differ from non-traumatic headaches in severity more than type of headache, say the researchers. Headache complexity could be a useful tool to assess post-traumatic headaches. (Cephalalgia, Nov. 27, 2020)
|
New technique could improve wound healing
 Photo: ©iStock/yenwen (12/10/2020)
A study led by a Corporal Michael J. Crescenz VA Medical Center researcher has demonstrated a process that could lead to better wound healing. Wounds often heal with fibrous scar tissue that can cause problems. In a mouse model, researchers used medication to activate pain receptor cells in the skin to promote wound healing. Activating the pain receptors stimulated the skin cells to produce interleukins, proteins involved in the body’s immune response. Triggering this immune response led to less scar tissue and promoted tissue regeneration. The results present a new avenue for research into faster and healthier wound healing, according to the researchers. (Science Immunology, Aug. 28, 2020)
|
Elevated immune response leads to more severe COVID-19
 Photo: ©iStock/JONGHO SHIN (12/02/2020)
Elevated immune response is associated with more severe COVID-19 and death, found a review led by a Michael E. DeBakey VA Medical Center researcher. The review analyzed 16 previous studies. Researchers found that COVID-19 patients with higher levels of interleukins, proteins secreted by the immune system, were more likely to have worse symptoms or die, compared with patients with lower levels. Conversely, high levels of a different type of immune proteins (CD4 and CD8) were linked to better prognosis in COVID-19 patients. The results suggest that medications that block interleukin production could be a useful treatment for COVID-19, say the researchers. A number of interleukin blockers are already being tested as possible treatments. (Diabetes and Metabolic Syndrome, November–December 2020)
|
Blood pressure medications not linked to worse COVID-19
 Photo: ©iStock/anyaivanova (12/02/2020)
Common blood pressure drugs are not linked to worse COVID-19 outcomes, according to a review by VA Portland researchers. Researchers reviewed 17 studies on how angiotensin-converting enzyme (ACE) inhibitors and angiotensin-receptor blockers (ARBs) interact with the SARS-CoV-2 virus. Both types of drugs are used to treat high blood pressure and heart failure. Evidence suggests that taking ACE inhibitors or ARBS does not lead to more severe COVID-19. The drugs also were not linked to positive SARS-CoV-2 test results. The researchers found four studies looking at ACE inhibitors or as COVID-19 treatments, but results from these studies are not yet available. (Annals of Internal Medicine, Aug. 4, 2020)
|
Phone-based diabetic kidney disease care effective for African American patients
 Photo: ©iStock/kali9 (12/02/2020)
A telehealth program could effectively slow kidney decline in African American patients, according to a Durham VA and Duke University study. Pharmacists delivered a phone-based intervention to patients with diabetic kidney disease. The program focused on behavioral and medication management. African American patients who received the program had significantly greater control of eGFR levels (a measure of kidney function), compared with patients receiving usual care. Non-African American patients in the program had a much faster decline in eGFR levels. The results suggest that this high-risk population may respond well to a telehealth approach to diabetic kidney disease care, say the researchers. (Medical Care, November 2020)
|
Inflammation may cause motor slowing in patients with schizophrenia
 Photo: ©iStock/1147468451 (11/23/2020)
Inflammation may play a role in schizophrenia-related movement problems, according to an Atlanta VA and Emory University study. Fine motor deficits are common in patients with schizophrenia. Researchers had patients with schizophrenia complete motor tasks (e.g., a finger tap test) and also tested their blood. As expected, patients with schizophrenia were slower on motor tests than controls without the disease. Patients with slower motor performance also had higher concentrations of molecules associated with inflammation in their blood. The results add to growing evidence that inflammation is the cause of motor slowing in people with schizophrenia and other mental conditions, say the researchers. (NJP Schizophrenia, April 1, 2020)
|
Walking program improves diabetes control
 Photo: ©iStock/monkeybusinessimages (11/23/2020)
A new walking program improves older patients’ health and diabetes control, found a South Texas Veterans Health Care System study. Patients 60 and older with diabetes participated in the Geriatrics Walking Clinic (GWC), a six-week program to promote physical activity. Participants were given a pedometer and weekly phone calls to monitor progress and give encouragement. Participants showed lowered HbA1c levels—a measure of diabetes control—at three, six, and 12-month follow-ups. They also improved their walking speed. The results highlight the benefits of exercise programs such as GWC for older patients with diabetes. (Geriatric Nursing, Nov. 3, 2020)
|
Perceived discrimination linked to worse arthritis outcomes
 Photo: ©iStock/LightFieldStudios (11/23/2020)
Perceived discrimination contributes to poor osteoarthritis outcomes, found a study by VA researchers and colleagues. Researchers evaluated more than 500 older Veterans with knee osteoarthritis. They found that those with higher cumulative disadvantage had significantly higher perceived discrimination. Cumulative disadvantage was defined as belonging to multiple socially disadvantaged groups. The researchers identified female gender, African American race, low income earning, and unemployment due to disability as known social disadvantages. Those with higher disadvantage also had higher pain and depression symptoms. Analysis showed that perceived discrimination was largely responsible for this connection. The results show that discrimination can lead to poorer physical and mental health outcomes, say the researchers. (Arthritis Care & Research, Oct. 7, 2020)
|
Stroke survivor mental deficits negatively affect caregiver well-being
 Photo: ©iStock/Chinnapong (11/19/2020)
Stroke patients’ emotional or cognitive deficits negatively impact caregiver well-being, found a North Florida/South Georgia VA study. Researchers surveyed 109 caregivers of stroke survivors. They found that higher cognitive and emotional deficits in the stroke patient led to more depression and burden in the caregiver. Cognitive/emotional deficits negatively affected caregiver mental quality of life. Higher motor or functional deficits in those they cared for did not significantly affect caregiver outcomes. The results suggest that cognitive/emotional deficits impact caregivers more than physical deficits, say the researchers. (Disability and Health Journal, Nov. 4, 2020)
|
Program helps lower self-stigma from PTSD
 Photo: ©iStock/SDI Productions (11/19/2020)
A new group program could help Veterans with PTSD deal with self-stigma, according to a VA Maryland study. Self-stigma is when someone comes to believe that common negative stereotypes and assumptions about PTSD are true of oneself. Researchers began a pilot program: Ending Self-Stigma for PTSD. The program involves nine group sessions aimed at learning tools to address PTSD stigma and self-stigma. Compared with Veterans receiving usual care, those in the program showed significantly less self-stigma and depression symptoms. They also had higher social confidence and feelings of belonging. The results show that the new program could help Veterans cope with negative views of PTSD, say the researchers. (Journal of Traumatic Stress, Oct. 15, 2020)
|
Exercise alleviates sleep problems caused by nicotine withdrawal
 Photo: ©iStock/PeopleImages (11/19/2020)
Exercise can help with sleep problems caused by nicotine withdrawal, found a Pittsburgh VA study. Sleep disturbances, including insomnia, are common symptoms of nicotine withdrawal. Researchers tested the effects of exercise on 49 daily smokers who were quitting. They found that engaging in daily exercise improved the patients’ ability to stay asleep. Patients with the greatest withdrawal severity had the most trouble falling asleep. But these participants also had the greatest benefits from afternoon exercise in how long it took them to fall asleep. The findings suggest that an exercise routine can improve sleep problems in people trying to quit smoking. (Experimental and Clinical Psychopharmacology, Oct. 29, 2020)
|
Gene variant increases risk of blast-induced memory problems
 Photo: ©iStock/peterschreiber.media (11/12/2020)
A specific gene variant may make people more vulnerable to cognitive problems from explosive blasts, found a study by VA Boston researchers and colleagues. Researchers examined the genomes of nearly 500 Veterans. They found that those with a common variant of the apolipoprotein (APOE) gene had an increased risk of memory problems after close-range blast exposure. This APOE variant is known to be a risk factor for Alzheimer’s disease. The results suggest that carriers of the gene variant could suffer worse outcomes from blast injuries than those with different forms of the gene, according to the researchers. They point out the importance of considering genetic risk when studying cognitive effects of trauma. (Journal of the International Neuropsychological Society, Nov. 3, 2020)
|
Involuntary opioid dose reduction does not lead to more chronic pain
 Photo: ©iStock/Charles Wollertz (11/12/2020)
Involuntary opioid dose reduction did not affect chronic pain severity, in a VA study. The study involved nearly 300 VA patients with chronic pain. Over the past year, about equal numbers had their opioid doses reduced involuntarily, reduced voluntarily, or kept the same. All three groups had similar pain levels before medication doses were adjusted. After 18 months, no significant differences in pain severity were found between the three groups. The findings suggest that reducing opioid dosing, whether voluntarily or involuntarily, does not lead to an increase in chronic pain, according to the researchers. (Journal of General Internal Medicine, Nov. 3, 2020)
|
Toxic exposure linked to rheumatoid arthritis-related antibodies
 Photo: ©iStock/katleho Seisa (11/12/2020)
Military toxic exposure was linked to antibodies associated with rheumatoid arthritis, in a VA study. In rheumatoid arthritis, the body’s immune system attacks its own tissue, including joints. Participants in a Veteran rheumatoid arthritis study were surveyed about inhalant exposures during their military service. The researchers found that Veterans with military burn pit or waste disposal exposure were more likely to have anti-cyclic citrullinated peptide antibodies, compared with those without toxic exposure. This type of antibody is an immune protein that mistakenly attacks healthy cells in the body. It is common in patients with rheumatoid arthritis. The results suggest that toxic exposure changes antibody expression and can increase the risk of rheumatoid arthritis, say the researchers. (Arthritis & Rheumatology, Oct. 15, 2020)
|
Molecular DNA changes linked to depression
 Photo: ©iStock/Gio_tto (11/06/2020)
A study involving an Atlanta VA researcher identified molecular DNA changes in the brain that may contribute to major depressive disorder. Researchers studied DNA methylation in the brain tissue of more than 600 older patients. DNA methylation is a process in which molecules called methyl groups attach to the DNA molecule. The researchers identified four new locations on the genome where methylation appears to be linked to major depressive disorder risk. Notably, the association between methylation levels and depression was stronger in men than in women. The results help explain how molecular changes could be involved in depression, according to the researchers. (Translational Psychiatry, July 30, 2020)
|
Cannabis use linked to psychiatric problems
 Photo: ©iStock/digihelion (11/06/2020)
Cannabis use is linked to psychiatric problems in Veterans, found a study by VA San Diego researchers and colleagues. Researchers surveyed more than 3,000 Veterans about their cannabis use and mental health. Those who used cannabis had higher odds of PTSD and mood, anxiety, and substance use disorders, compared with those who never used cannabis. Cannabis users also had higher rates of current suicidal thoughts, suicide attempts, and mental health treatment utilization. Veterans with cannabis use disorder (CUD) had higher odds of PTSD, mood and anxiety disorders, nicotine and alcohol dependence, and suicidal thoughts, compared with those who used cannabis but did not meet CUD criteria. While the researchers suggest that cannabis use could increase mental health burden, it is also possible that many Veterans with psychiatric issues turn to cannabis as a form of self-medication. Outreach and education are needed about possible cannabis-related psychiatric burden, say the researchers. (Journal of Affective Disorder, Sept. 29, 2020)
|
Risk factors for COVID-19 death
 Photo: ©iStock/homeworks255 (11/06/2020)
VA Puget Sound researchers identified risk factors for death from COVID-19. The study included almost 89,000 patients tested in the VA health system. More than 10,000 tested positive for COVID-19. Higher risk of death from the disease was linked to being older than 50, being male, and having more health conditions. The researchers could not confirm several risk factors identified in other, smaller studies. These factors include obesity, Black race, Hispanic ethnicity, and smoking. The findings can help predict disease outcomes and plan treatment accordingly, say the researchers. (JAMA Network Open, Sept. 1, 2020)
|
Cigarette smoke makes lung infection bacteria more dangerous
 Photo: ©iStock/bagi1998 (10/28/2020)
Cigarette smoke alters the genes of bacteria in the lungs, making them more resistant to the immune system, found a VA San Diego study. Researchers exposed the bacteria P. aeruginosa to cigarette smoke extract. Infection with this bacteria often leads to pneumonia. Smoke exposure changed the gene expression in the bacterium, making it more resistant to white blood cells. Cigarette smoke also increased biofilm formation, making the bacteria more resistant to antibiotics. P. aeruginosa also became more harmful in a mouse model of pneumonia when exposed to smoke. The results show one way that smoking cigarettes can increase the danger of lung infections, say the researchers. (Infection and Immunity, Oct. 19, 2020)
|
Transcranial magnetic stimulation reduces PTSD-linked anger
 Photo: ©iStock/fotografixx (10/28/2020)
Transcranial magnetic stimulation could reduce anger in Veterans with PTSD, found a Providence VA study. In transcranial magnetic stimulation, magnetic fields are applied to the outside of the skull to influence electrical currents in the brain. Researchers applied a form of this treatment called intermittent theta burst stimulation to patients with PTSD in 10 daily sessions. Patients receiving the treatment reported significantly reduced anger, compared with control patients. The change remained one month after treatment. Results suggest that the treatment could be an effective way to control increased anger caused by PTSD, according to the researchers. (Neuromodulation, Sept. 17, 2020)
|
Identity disruption linked to Veteran reintegration trouble
 Photo for illustrative purposes only. ©iStock/Geber86 (10/28/2020)
Identity disruption is linked to Veteran difficulty reintegrating into civilian life, according to a Minneapolis VA study. Identity disruption refers to questioning one’s sense of self and place in the world. Researchers surveyed more than 200 Veterans who served in Afghanistan and Iraq. About 49% of those surveyed showed signs of identity disruption. Identity disruption was linked to more severe PTSD symptoms, lower satisfaction with life, greater reintegration difficulty, and less social support. The findings suggest that understanding identity disruption could help Veterans better reintegrate into civilian life, say the researchers. (Developmental Psychology, November 2020)
|
Poor oral health linked to less gut bacteria diversity
 Veterans Health Administration photo (10/21/2020)
Oral health is linked to changes in the makeup of colon bacteria that could contribute to disease, found a study by Michael E. DeBakey VA Medical Center researchers and colleagues. Poor oral health has been associated with several diseases, but the reason for this link is not well understood. Researchers examined colonoscopy biopsies along with oral health questionnaires of 62 patients. They found that more tooth loss and gum disease were linked to lower bacteria diversity in the digestive tract. People with more tooth loss had lower levels or Faecalibacterium, bacterium known to be anti-inflammatory. Lower levels of this bacterium could indicate systemic inflammation, according to the researchers. The results suggest that poor oral health could lead to other health problems by altering the gut microbiota. (Digestive Diseases and Sciences, Sept. 24, 2020)
|
Immunotherapy improves cancer survival
 Photo: ©iStock/blueringmedia (10/21/2020)
Immune checkpoint inhibitors seem to improve cancer patients’ survival, according to a VA Boston study. Immune checkpoint inhibitors are drugs that block specific proteins. This allows immune cells to recognize and attack cancer cells. The researchers looked at data on more than 11,000 VA patients, in one of the largest studies on the topic. The most common type of cancer treated was lung cancer, followed by melanoma. Odds of survival a year after treatment were somewhat lower in this group of VA patients, compared with other studies of immune checkpoint inhibitors. However, mortality rates were similar after adjusting for frailty. Patients given immune checkpoint inhibitors generally survived longer than patients receiving standard care. This study provides a platform for further analysis of immunotherapy outcomes in real-world patients, say the researchers. (Journal of Clinical Oncology, Oct. 19, 2020)
|
TBI increases risk of dementia to different degrees based on race
 Photo for illustrative purposes only. ©iStock/Juanmonino (10/21/2020)
Traumatic brain injury significantly increases the risk of dementia, and race appears to affect this relationship, found a San Francisco VA study. Researchers studied data on nearly a million older Veterans. Overall, Veterans with a TBI were more than twice as likely to be diagnosed with dementia than those without TBI. White Veterans were nearly three times more likely to have dementia if they had a TBI. Dementia was more than twice as likely in Black Veterans with TBI, compared to Black Veterans without TBI. TBI nearly doubled the risk of dementia in Hispanic Veterans. More research is needed to understand how race contributes to TBI’s connection to dementia, say the researchers. (Neurology, Sept. 29, 2020)
|
Many Veterans with suicidal thoughts not receiving mental health care
 Photo: ©iStock/vadimguzhva (10/14/2020)
More than 3 in 5 Veterans who have suicidal thoughts are not engaged in mental health treatment, according to a VA study. Researchers looked at data from 2011 on more than 3,000 Veterans. About 7% said they have suicidal thoughts. Only 36% of those were receiving mental health treatment. Younger Veterans; women; those with current depression; and those with more lifetime suicide attempts, lifetime trauma, and medical problems were more likely to be in treatment. Mistrust of mental health providers and fear of damaging one’s reputation were linked to lower mental health treatment. The results highlight a need to find new ways to engage Veterans at risk for suicide in mental health care, say the researchers. (Journal of Psychiatric Research, July 29, 2020)
|
Novel risk factors for heart attack in younger patients
 Photo for illustrative purposes only. ©iStock/digitalskillet (10/14/2020)
Younger patients who had heart attacks had both traditional and non-traditional risk factors, found a study by Michael E. DeBakey VA Medical Center researchers and colleagues. The study looked at characteristics of patients younger than 55 who had a heart attack. Younger patients were at higher risk of heart attack if they had HIV, lupus, and obstructive sleep apnea. Younger patients with rheumatoid arthritis had a lower risk of heart attack. Cigarette smoking, obesity, high lipid (fat) content in the blood, and a family history of coronary artery disease were linked to heart attack risk in both younger and older patients. Younger patients with HIV, lupus, or sleep apnea should be monitored for heart attack, in addition to those with traditional risk factors, conclude the researchers. (International Journal of Cardiology, Sept. 23, 2020)
|
Yoga a cost-effective treatment for back pain
 Photo for illustrative purposes only. ©iStock/jacoblund (10/14/2020)
Yoga can be a cost-effective treatment for Veterans with chronic low back pain, found a VA San Diego study. Patients were assigned to either 60-minute yoga sessions twice a week for 12 weeks or delayed treatment, in which they would receive the yoga treatment after the study. Yoga instruction could be provided for about $300 per participant. An analysis indicated that the costs of this program are offset by long-term reductions in health care costs for participants. Research suggests that yoga may have health benefits similar to physical therapy and can likely be delivered at a lower cost. The study suggests that yoga could be a useful non-opioid option for patients with chronic low back pain, say the researchers. (Medical Care, September 2020)
|
Head and neck cancer rates increasing
 Illustration: ©iStock/Nerthuz (10/08/2020)
Head and neck cancer in VA patients has become more common in recent years, found a Michael E. DeBakey VA Medical Center study. Researchers looked at data on more than 12,000 patients with head and neck cancers. They found that the incidence of this type of cancer in VA patients declined between 2000 and 2006, but then increased between 2006 and 2012. The increase was seen across ethnic and age groups. Although smoking remains highly connected to this type of cancer, the percentage of cancer in those who never smoked has increased. About 8% of those with head or neck cancer were nonsmokers in 2000. This number increased to 16% in 2012. The finding suggests a different cause of the cancer beyond smoking, such as human papilloma virus, say the researchers. (Head and Neck, Sept. 12, 2020)
|
Air pollution linked to stroke risk in atrial fibrillation patients
 Photo: ©iStock/lapandr (10/08/2020)
Higher air pollution increases the risk of stroke in patients with atrial fibrillation, found a study by VA Pittsburgh and University of Pittsburgh researchers. The study followed more than 31,000 patients with atrial fibrillation along with pollution measures for a number of years. Atrial fibrillation refers to irregular heartbeat. Those exposed to greater fine particulate matter had a significantly higher risk of stroke, compared with those exposed to less pollution. Fine particulate matter refers to airborne particles less than 2.5 micrometers in diameter. The higher the air pollution, the higher the risk of stroke. The results highlight the need to address how air pollution contributes to cardiovascular disease, according to the researchers. (JAMA Network Open, Sept. 1, 2020)
|
American Indian/Alaskan Native Veterans have higher risk of death
 Photo for illustrative purposes only. ©iStock (10/08/2020)
American Indian/Alaskan Native Veterans had higher death rates than other ethnic groups, found a VA Greater Los Angeles study. Researchers looked at health and census data on more than 5 million Veterans. They found that American Indian/Alaskan Native Veterans had a 7% higher risk of death from any cause in a given year, compared to Black and white Veterans. Mortality rates were similar between other ethnic groups when controlling for other factors. Neighborhood segregation was a large contributor to this disparity. American Indian/Alaskan Native Veterans who lived areas with greater non-Hispanic Black segregation had a lower risk of death than those in other areas. Living near tribal reservations also seemed to lessen the disparity. The results suggest that social characteristics of neighborhoods need to be examined to address racial disparities, say the researchers. (Health Services Research, October 2020)
|
Risk factors for lower-limb re-amputation
 Photo: ©iStock/Morsa Images (09/30/2020)
VA Puget Sound researchers identified risk factors that led to further lower-limb amputation in Veterans. The study included more than 7,000 VA patients who had an amputation because of diabetes or peripheral artery disease. Re-amputation included removing tissue and bone near the amputation site or amputation higher on the leg, and might become necessary because of improper healing. Re-amputation was highest (41%) in patients who had part of the foot removed. About 25% of amputations at the tibia and 9% at the femur required re-amputation. Risks for re-amputation included chronic obstructive pulmonary disease, reduced blood flow, and alcohol misuse. Different levels of amputation carried different risk factors. The results will help surgeons and patients make decisions on amputation level, according to the researchers. (European Journal of Vascular and Endovascular Surgery, Aug. 12, 2020)
|
Combat exposure linked to suicidal thoughts through PTSD symptoms
 U.S. Army photo by Maj. Thomas Cieslak (09/30/2020)
PTSD symptom severity largely controls the link between combat exposure and suicidal thoughts in Veterans, found a Durham VA study. Previous findings have been mixed on whether combat exposure is directly related to suicidal thoughts or if other factors are involved. Researchers evaluated 319 Veterans at the beginning of the study, as well as six and 12 months later. They found that the link between combat exposure and the risk of suicidal thoughts was controlled by how severe PTSD symptoms were in 64% of cases. The results emphasize the importance of addressing PTSD symptoms when trying to prevent suicide, say the researchers. (Suicide and Life-Threatening Behavior, Aug. 8, 2020)
|
One-day mental health workshop helps rural Veterans in distress
 Photo: ©iStock/davidperks (09/30/2020)
Rural Veterans in mental distress found community-based mental health workshops helpful, in a VA study. VA researchers partnered with nonprofit organizations to identify distressed Veterans in rural areas. They conducted a one-day acceptance and commitment therapy group workshop in rural locations for 31 Veterans. Each Veteran was interviewed after the workshop, as well as one and three months later. Veterans appreciated the structure, content, and environment of the workshops. Most used the learned coping skills in their daily lives, and some initiated new treatment after the workshop. Veterans scored better on measures of functioning and reintegration afterward. They also showed higher feelings of meaning and purpose and reduced distress. The results show that partnering with rural non-profits can help engage rural Veterans in mental health care, say the researchers. (Journal of Behavioral Medicine, Sept. 17, 2020)
|
Nondrug therapy use for chronic pain common
 Photo by Robert Turtil (09/23/2020)
Nondrug therapy use is common in Veterans with chronic pain, found a Minneapolis VA study. Researchers surveyed nearly 9,000 Veterans who had been prescribed long-term opioid therapy for chronic pain. In the past year, 80% used at least one nondrug therapy for pain. Therapies included meditation, psychotherapy, yoga, and other techniques. Younger Veterans and female Veterans were more likely to use nondrug therapies. Greater pain severity was linked to lower use of exercise and movement therapies. Further research into complementary and integrative health could lead to more nondrug treatment for chronic pain, say the researchers. (Medical Care, September 2020)
|
Exploring gene expression in prostate cancer
 Photo: ©iStock/jamesbenet (09/23/2020)
A team including Southeast Louisiana Veterans Health Care System researchers found multiple gene expression trends linked to prostate cancer. Gene expression refers to the creation of proteins based on genetic instructions. The team studied data from three large genomic databases. They found that gene expression of the protein FBXW7 was significantly lower in prostate cancer, compared to in normal prostate tissue. Expression of several related proteins (FBXW8–10) was higher in prostate cancer, as well. The study also found higher expression of several different FBXW proteins in metastatic castration-resistant prostate cancer, a hard-to-treat form of the cancer, compared with more common prostate cancers. The results help explain the role genes play in prostate cancer risk, say the researchers. They also suggest that FBXW7 has potential as a treatment to suppress tumor growth. (American Journal of Clinical and Experimental Urology, Aug. 15, 2020)
|
Cause of light sensitivity the same in multiple conditions
 Photo: ©iStock/laflor (09/23/2020)
Light sensitivity associated with three separate conditions could share a common cause, according to a review by VA researchers and colleagues. Patients with dry eye disease, migraines, and traumatic brain injury all commonly have a sensitivity to light. These conditions are usually considered different types of medical issues. However, they often occur together. By reviewing available studies, the researchers found that light sensitivity is linked to disruptions in brain connectivity in all three conditions. Light sensitivity is closely connected to increased activity of the protein CGRP. The results suggest that treatments that target neural pathways should be considered for light sensitivity in these conditions, according to the researchers. (British Journal of Ophthalmology, July 23, 2020)
|
Understanding prostate cancer molecular processes
 Photo: ©iStock/selvanegra (09/17/2020)
Minneapolis VA researchers explored molecular processes involved in prostate cancer growth. Protein kinase CK2 is an enzyme involved in the life cycle of the cell. It is known to be elevated in many types of cancer, but its function within cancer cells is not well known. The researchers exposed prostate cancer cell lines in the lab to compounds that inhibit protein kinase CK2. They found that inhibiting the enzyme led to decreased levels of calcium ions in the body of the cell and increased levels in the endoplasmic reticulum and mitochondria, two discrete or structures in the cell. Calcium ions are known to drive signaling of processes within cells. Calcium levels were much lower within cells given enough protein kinase CK2 inhibitors to kill the cell. This study increases the understanding of the processes involved in cancer cell growth and death. It could lead to new areas of study for treatment of prostate cancer. (Molecular and Cellular Biochemistry, July 2020)
|
Opioid misuse linked to emotion dysregulation
 Photo: ©iStock/VladimirSorokin (09/17/2020)
Opioid misuse could cause emotion dysregulation, according to a study by VA Salt Lake City researchers and colleagues. Researchers had patients on long-term opioid therapy for chronic pain complete an emotion regulation task. The task involved viewing emotionally charged pictures while trying to control one’s emotions. Patients were measured for heart rate and galvanic skin response (a change in the electrical resistance of skin caused by emotional stress). Patients who correctly followed their medication protocols were able to control their emotional responses. Those who misused opioids had increases in the reaction measures during tests involving negative emotion. They also did not show signs of emotional control during positive emotion tests. The results suggest that opioid misuse is linked with an inability to control emotions that occurs immediately after emotional provocation, say the researchers. (Progress in Neuro-Psychopharmacology and Biological Pharmacology, June 24, 2020)
|
Blast exposure linked to attention problems
 DOD photo by Lance Cpl. Immanuel Johnson (09/17/2020)
Blast pressure from an explosion contributes to cognitive problems caused by traumatic brain injury (TBI), found a VA Mid-Atlantic Mental Illness Research, Education, and Clinical Center (MA-MIRECC) study. Explosions cause a pressure wave in the air that can strike people near the blast. More than 250 post-9/11 Veterans completed cognitive tests and surveys about blast exposure. Those with a mild TBI performed worse on cognitive tests than those without TBI. The severity of blast pressure seemed to control this relationship. In Veterans with mild TBI, those who had experienced more severe blasts showed lower performance on a simple attention task, even with the same TBI diagnosis. The results show that severe pressure waves could lead to persisting attention difficulties that impede cognitive function in Veterans with TBI, say the researchers. (Neuropsychology, July 16, 2020)
|
3D-printed masks can be decontaminated of coronavirus using standard methods
 Photo: ©iStock/beerkoff (09/11/2020)
VA researchers identified several methods that effectively decontaminate 3D-printed mask material of the virus that causes COVID-19. The researchers tested viral activity on mask material using multiple disinfectants. They found three solutions that inactivated the virus: bleach, quaternary ammonium sanitizer, and hydrogen peroxide. Likewise, exposing the material to dry heat for 30 minutes inactivated the viruses. The liquid alcohol isopropanol was not as effective. The cleaning methods tested did not interfere with the integrity of the 3D-printed material. Standard decontamination methods can be an effective way to allow for reuse of 3D-printed material when surgical mask supplies are limited, conclude the researchers. (Infection Control and Hospital Epidemiology, Aug. 12, 2020)
|
Educational program increases Veterans’ confidence in suicide crisis hotline
 Photo for illustrative purposes only. ©iStock/BraunS (09/11/2020)
Educating Veterans about the Veterans Crisis Line improves their views of the suicide prevention resource, found a study by the VA Center for Clinical Management and Research. The Veterans Crisis Line is a toll-free, confidential hotline staffed by mental health professionals 24 hours a day. It offers support and help to Veterans thinking about suicide. Usage numbers suggest that the hotline is likely underutilized by high-risk Veterans. Researchers developed a program to educate Veterans about the hotline. It includes discussing participants’ perceived barriers and calling the hotline together with their therapist to provide firsthand experience with the service. Researchers provided the program to 301 Veterans. Preliminary results suggest that the program significantly increased Veterans’ comfort with and confidence in the hotline. The program could increase the likelihood of high-risk Veterans in crisis using the hotline for help. The Veterans Crisis Line can be reached by calling 1-800-273-8255 or texting #838255. (Cognitive and Behavioral Practice, June 25, 2020)
|
Testing for virus presence after COVID-19 infection
 Photo: ©iStock/homeworks255 (09/11/2020)
Researchers from the San Francisco VA and University of California San Francisco studied how long it took health care workers with COVID-19 to test negative after initial infection. They tested 12 employees with reverse transcriptase polymerase chain reaction (RT-PCR). RT-PCR measures the amount of a specific type of RNA (genetic material). It can be used to test for the presence of the virus that causes COVID-19. The time between initial COVID-19 infection and a negative test ranged from seven to 57 days. The average time was 34.5 days. Understanding this time range could help institutions make decisions on when it is safe for employees to return to work, say the researchers. (Journal of Occupational and Environmental Medicine, Aug. 13, 2020)
|
Veterans Choice Program did not reduce appointment wait times
 Photo: ©iStock/SDI Productions (09/02/2020)
Giving Veterans the choice to receive specialty care from non-VA community providers did not lower appointment wait times, according to a VA Boston study. The Veterans Choice Program, passed in 2014, allowed Veterans to access care in the community if they live far from a VA facility. Researchers looked at data from 2013 to 2019 to study wait times in four specialties: cardiology, gastroenterology, orthopedics, and urology. The data included 6.9 million VA consultations and 869,000 community visits. The results showed that average wait times for appointments within VA were shorter than those in the community. Administrative delays did not account for the difference. Wait times in VA declined during the study period. However, the decline began before Veterans Choice was implemented. Geographical areas with the highest VA wait times also had the highest community wait times. The results suggest that increasing eligibility for community care may be insufficient to lower Veterans’ wait times, say the researchers. (JAMA Network Open, Aug. 3, 2020)
|
HIV drug may increase kidney disease, fractures
 Photo: ©iStock/erdikocak (09/02/2020)
A common treatment for HIV was associated with higher odds of chronic kidney disease and osteoporotic fractures, found a study by Columbia VA researchers and colleagues. The team compared outcomes for nearly 5,000 VA patients with HIV. Some were on the medication tenofovir disoproxil fumarate, sold as Viread, while others were not. Those taking the drug had 48% higher odds of chronic kidney disease. They also had more than twice the risk of osteoporotic fracture. In osteoporosis, bones become more fragile due to bone deterioration or low bone mass. HIV regimens using this drug have been associated with impaired kidney function and loss of bone mineral density in the past. The results shed light on the extent of this association. (Current Medical Research and Opinion, Aug. 28, 2020)
|
Patient portal use higher in those with more severe depression
(09/02/2020)
Patients with more severe depression were more likely to use an online patient portal, found a study of VA users. Researchers looked at whether more than 3,000 Veterans with depression used the patient portal My HealtheVet. My HealtheVet allows VA patients to refill prescriptions, manage appointments, message their doctors, and view their health records. Patients with more severe depression were more likely to have registered for the portal and downloaded medical records, compared to those with milder symptoms. Male patients had lower rates of registration than women. Older patients were also less likely to register than younger patients. African American Veterans had lower rates of portal use, compared with other races. The results highlight the need to address barriers to patient portal use, say the researchers. (Journal of Affective Disorder, Oct. 1, 2020)
|
Lower weight, diabetes increase risk of death from pulmonary hypertension
 Photo: ©iStock/Rostislav_Sedlacek (08/26/2020)
Lower weight and diabetes are risk factors for death in patients with pulmonary hypertension, found an Atlanta VA study. Pulmonary hypertension refers to high blood pressure in the arteries of the lungs and heart. Researchers looked at data on more than 110,000 Veterans diagnosed with pulmonary hypertension. Diabetes increased patients’ risk of death by 28% to 33%. Surprisingly, higher body mass index was linked to lower mortality. Underweight and normal weight patients were at higher risk of death than those who were overweight or obese. The results underscore the need for more research on how metabolic factors affect pulmonary hypertension, say the researchers. (American Journal of Cardiology, Aug. 15, 2020)
|
Neurostimulation could prevent wheelchair falls
 Photo: ©iStock/vadimguzhva (08/26/2020)
Researchers with the VA Advanced Platform Technology Center in Cleveland developed a neurostimulation system to help stop users from falling out of wheelchairs. The team developed an algorithm to detect sudden stops during wheelchair use. Sudden stops are often a cause of falls in paralyzed wheelchair users. The team then tested the algorithm with three volunteers with spinal cord injury who had an implanted neurostimulation system and three nondisabled volunteers. When the program detected a sudden stop, the system triggered stimulation to stiffen the muscles of the user’s trunk. This allowed the user to maintain a seated posture. The system was able to detect sudden stops with a 93% success rate. The participants consistently reported feeling safer when the system signaled their implants to stiffen their muscles, providing more stability. The results suggest that the neurostimulation system could improve wheelchair safety for paralyzed users, according to the researchers. (Journal of Spinal Cord Medicine, Aug. 14, 2020)
|
Racial/ethnic disparities exist in diabetes control
 Photo: ©iStock/vitapix (08/26/2020)
Disparities in diabetes control based on race and ethnicity exist across the country, found a study of VA patients. Researchers looked at data on more than a million VA patients with diabetes. They found that the percentage of patients with uncontrolled diabetes varied by location, ranging from 19% to 29%. Hispanic patients and non-Hispanic Black patients were more likely to have uncontrolled diabetes, compared with non-Hispanic white patients. The disparity was consistent across most geographic areas. The results highlight areas that need to be addressed in diabetes care, say the researchers. (Diabetes Care, Aug. 7, 2020)
|
Treatment for depression linked to apathy
 Photo: ©iStock/duncan1890 (08/19/2020)
Selective serotonin reuptake inhibitor (SSRI) use may be linked with higher rates of apathy syndrome, found a Central Arkansas Veterans Healthcare System study. SSRIs are a common treatment for depression. Apathy has been reported as a potential side effect of SSRIs, but this association has not been systematically assessed. Apathy refers to loss of motivation, energy, and curiosity. The researchers compared scores on an apathy evaluation scale between patients in mental health treatment taking an SSRI and those not on the medication. They found that 92% of patients on SSRIs had clinically significant apathy, compared to 61% not on SSRIs. Apathy was most common in patients with dementia. The results suggest that clinicians should assess apathy when evaluating patients on SSRIs, say the researchers. (Medicine, Aug. 14, 2020)
|
Many patients receive potentially dangerous medication combinations from dentists
 Photo: ©iStock/licsiren (08/19/2020)
Many older patients receive opioids from dentists that can cause adverse reactions with their other medications, according to a study by VA researchers and colleagues. The researchers looked at data on more than 40,000 older dental patients. They found that about 10% were prescribed a potentially inappropriate medication combination. Patients given potentially dangerous combinations were more likely to seek health care for an acute condition after the dental visit. Higher opioid doses prescribed by a dentist increased this likelihood. More support is needed to make sure dentists are aware of possible dangerous medication combinations, say the researchers. (Pharmacotherapy, Aug. 7, 2020)
|
Keeping women Veterans in PTSD therapy
 Photo: ©iStock/SDI Productions (08/19/2020)
Women Veterans with PTSD are more likely to stay in psychotherapy when treatment aligns with their preferences, found a study by VA Palo Alto researchers. The researchers surveyed more than 6,000 women Veterans with PTSD. They found that 79% used psychotherapy. Of those, 42% received enough psychotherapy (at least eight visits) to be clinically meaningful. According to the survey, receiving treatment aligned with gender- and group-related preferences was associated with higher therapy retention. Other mental health conditions, exposure to military sexual trauma, and being a minority were also linked to higher psychotherapy use. Being a parent was linked to lower retention. Enhancing efforts to use shared decision-making for mental health care could increase PTSD treatment retention for women Veterans, according to the researchers. (Women’s Health Issues, July 14, 2020)
|
Potential new migraine medication developed
 Photo: ©iStock/NickyLloyd (08/12/2020)
An international team including an Iowa City VA researcher has developed a potential new nasal migraine medication. Previous research has established that the peptide (a string of amino acids) CGRP is involved in migraine development. The researchers prepared a compound that blocks the receptors in the brain that bind to CGRP. Using a mouse model, they found that the compound significantly reduced CGRP’s ability to activate the receptors, compared to other compounds. The compound can be formulated into a dry powder without degrading, meaning it potentially could be used nasally to treat migraines, according to the researchers. (Journal of Pharmacy and Pharmacology, June 25, 2020)
|
Acid reflux may accelerate COPD progression
 Photo: ©iStock/stevanovicigor (08/12/2020)
Gastroesophageal reflux disease (GERD) may accelerate chronic obstructive pulmonary disease (COPD) progression, according to a study by Minneapolis VA researchers. GERD, a chronic form of acid reflux, commonly occurs with COPD. The researchers looked at nearly 6,000 patients with COPD over a five-year study. They found that those with GERD had faster decline in some measures of lung function, compared to those without GERD. Patients taking common medications for GERD had faster lung function decline than those not taking the medications. Although the lung function differences were relatively small, say the researchers, more study is warranted on how GERD affects COPD progression because of its high prevalence. (Respiratory Health, Aug. 3, 2020)
|
Veterans with unstable housing at greater risk of death
 Photo: ©iStock/Rawf8 (08/12/2020)
Veterans who experience homelessness or a threat of unstable housing have a higher risk of death from external causes, found a large VA study. Researchers looked at data on nearly 6 million Veterans over a four-year period. About 3% had unstable housing or were at imminent risk of homelessness during the study period. Veterans with unstable housing had a 1.69 times risk of death than those with stable housing. Those at imminent risk of housing instability had a nearly 1.5 times higher risk of death as well. Unstably housed Veterans had over three times greater risk of dying by homicide and unintentional injury. They also had a 1.75 times higher risk of dying by suicide. Veterans at imminent risk for housing instability had over twice the risk of dying by homicide and nearly two times the risk of dying by injury or suicide. The results show that more proactive measures are needed to prevent death in Veterans with unstable housing, say the researchers. (Journal of Social Distress and Homelessness, Aug. 5, 2020)
|
Copper-impregnated hospital surfaces may reduce microbial contamination
 Photo: ©iStock/monkeybusinessimages (08/07/2020)
Copper-impregnated surfaces may reduce microbial contamination in hospital rooms, according to a Central Texas VA study. High-touch hospital surfaces such as sinks, tray tables, and bedrails were replaced with a new material made of 20% copper oxide in a polymer-based resin. Researchers tested for bacterial colonies on high-touch surfaces in hospital rooms with and without copper-impregnated materials. Surfaces were tested three times a day for three days to see whether the copper stopped microbes from re-accumulating. In further evidence of copper’s germ-fighting ability, copper-impregnated surfaces had about 40% the bacterial count as standard laminate surfaces. Copper-impregnated solid surfaces could reduce microbial contamination in patient rooms, conclude the researchers. (Open Forum Infectious Diseases, June 19, 2020)
|
Implanted electrical stimulation device for paralysis safe and effective
 Photo: ©iStock/jxfzsy (08/07/2020)
Researchers from VA’s Advanced Platform Technology Center showed that nerve health is maintained after implanting an electrode stimulation device in a patient with spinal cord injury (SCI). A patient with leg paralysis from an SCI was given an implanted nerve cuff electrode device to stimulate his leg muscles and allow him to stand. In the first such human trial, the researchers examined physiologic changes to the nerves during the surgery and a year later. After a year, the nerves remained healthy. The patient showed strengthened motor responses from the electrical stimulation. Some nerve irritation occurred during the surgery but did not continue afterwards. The results show that implanted electrodes to restore function after SCI can be safe and effective, according to the researchers. (Journal of NeuroEngineering and Rehabilitation, July 14, 2020)
|
New assessment for pulmonary hypertension
 Photo: ©iStock/yodiyim (08/07/2020)
VA researchers and colleagues have established what they propose as a new standard for assessing pulmonary hypertension. Pulmonary hypertension is high blood pressure in the lung arteries. If the condition is left untreated, average survival is two to three years after diagnosis. However, a uniform, evidence-based definition for pulmonary hypertension has not existed till now. The researchers looked at data on more than 40,000 patients in the VA health care system over a nine-year period. They found that patients with pulmonary vascular resistance of 2.2 Wood units (a measure of blood flow from the pulmonary artery to the lungs) or higher were at elevated risk of death. This number is well below what is currently associated with the disease in clinical practice. The new standard will help identify patients at risk of death who previously had been considered normal, say the researchers. (Lancet Respiratory Medicine, July 27, 2020)
|
Measuring brain connectivity after magnetic stimulation
 Photo: ©iStock/fotografixx (07/29/2020)
Researchers at the Providence VA Medical Center have developed a way to study how brain connectivity is affected by transcranial magnetic stimulation (TMS). In TMS, magnetic pulses are used to affect brain signals as a treatment for PTSD or depression. The researchers studied intermittent theta burst stimulation (iTBS), a form of TMS that uses low-frequency magnetic pulses. They used an EEG (electroencephalography) to image the brains of participants with PTSD and controls before and after iTBS. They also used machine learning programs to track changes. This system was able to successfully track which patients had received iTBS 75% of the time. Using the brain imaging, the researchers were able to show that iTBS increased connectivity between the midline central/occipital regions of the brain and decreased it between the frontal and central regions. The results could provide a window into exactly how TMS affects the brain, according to the researchers. This approach could help develop individualized treatment methods for PTSD, they say. (European Archives of Psychiatry and Clinical Neuroscience, July 27, 2020)
|
Alcohol use changes linked to HIV medication non-adherence
 Photo: ©iStock/eclipse_images (07/29/2020)
Changes in alcohol use were linked to non-adherence to HIV medication, found a study of VA patients. Researchers looked at how well more than 21,000 patients with HIV kept up with their antiretroviral therapy. They found that increased alcohol use led to a decrease in medication adherence. The finding confirms previous research that found alcohol use increases non-adherence. However, the study also found that a decline in alcohol use was linked to decreased medication adherence. Patients whose alcohol use remained steady had the most stable HIV medication adherence. The results suggest that unstable alcohol use—which could reflect underlying alcohol use disorder—can lead to lower antiretroviral therapy adherence, say the researchers. (AIDS and Behavior, July 2, 2020)
|
History of sexual assault linked to increased emergency department use
 Photo: ©iStock/MJFelt (07/29/2020)
Women Veterans who had experienced sexual assault were more likely to use emergency departments, in an Iowa City VA study. Researchers conducted phone interviews with nearly 1,000 women Veterans who used VA health care. Of those, 64% had visited a VA or non-VA emergency department in the previous five years. Women with a history of mental health diagnosis and those who had experienced sexual assault were almost twice as likely to have visited an emergency department, compared with those without a history of sexual assault. It is unclear whether the findings are due to greater health care needs, suboptimal access to treatment, or lack of health care coordination, say the researchers. (Women’s Health Issues, June 19, 2020)
|
Efforts to change sexual orientation increases suicidal thoughts, actions
 Photo: ©iStock/kieferpix (07/22/2020)
Efforts to change one’s sexual orientation lead to much higher rates of suicidal behavior, found a study by a VA Pittsburgh researcher and colleagues. Researchers looked at survey data from more than 1,500 non-transgender lesbian, gay, and bisexual adults. About 7% had experienced sexual orientation change efforts. These efforts, sometimes referred to as conversion therapy, include various approaches, meant to condition a person against attraction to the same gender. More than 80% of change efforts in the study were administered by religious leader. Participants who experienced change efforts were nearly twice as likely to have suicidal thoughts at some point in their lives. Change efforts increased odds of planning to attempt suicide by 75%. Odds of a suicide attempt increased by 88% with change efforts. The results support minimizing exposure to sexual orientation change efforts and offering identity-confirming care to sexual minorities, say the researchers. (American Journal of Public Health, June 10, 2020)
|
Medical record notes often inaccurate
 Photo: ©iStock/Zinkevych (07/22/2020)
Medical records often contain errors that may affect care and billing, found a Jesse Brown VA Medical Center study. Patients covertly recorded medical appointments to compare with medical record notes. In 105 appointments, the study found 636 documentation errors. The errors included 181 charted findings that did not take place and 455 findings that were not charted. Almost all (90%) of the notes contained at least one error. The results show that the medical records should not be assumed to reflect care delivered, according to the researchers. Efforts are needed to improve documentation requirements, they say. (Journal of the American Medical Informatics Association, May 1, 2020)
|
Possible molecular link between nonalcoholic fatty liver disease and cancer
 Photo: ©iStock/jxfzsy (07/22/2020)
A team including Harry S. Truman Veterans’ Hospital researchers has identified the possible connection between liver cancer and nonalcoholic fatty liver disease (NAFLD). The rates of both NAFLD and hepatocellular carcinoma (liver cancer) have been increasing at an alarming rate. While NAFLD appears to be a risk factor for liver cancer, the mechanism behind this relationship is largely unknown. Researchers found that patients with liver cancer had reduced activity from the HADHA gene. They also found that mice with a deficiency of a protein analogous to HADHA were likely to develop NAFLD when young. Older mice with the protein deficiency developed hepatocellular carcinoma. The results suggest that impairment of this gene can lead to the progression from NAFLD to liver cancer, say the researchers. (International Journal of Cancer, March 16, 2020)
|
Increased blood flow in the brain linked to blast exposure
 Photo: ©iStock/mr.suphachai praserdumrongchai (07/16/2020)
Blast exposure may cause increased blood perfusion in the brain, found a VA Boston study. Perfusion refers to blood flow from the blood vessels to organ tissue. Previous studies have shown that damage to blood vessels may be related to poorer brain function after traumatic brain injury. Researchers performed brain scans on 160 military personnel. They found that as the number of blast exposures increased, perfusion also increased in many areas of the brain. The findings suggest that perfusion could be an important biomarker of brain health after blast exposure, say the researchers. (Journal of Cerebral Blood Flow and Metabolism, June 24, 2020)
|
New wheelchair design reduces bacterial contamination
 Photo by April Eilers (07/16/2020)
A new ergonomic wheelchair designed by Minneapolis VA researchers reduces bacterial hand contamination. In most manual wheelchairs, users push directly on the tires or on a push rim directly connected to the tires to move forward. This can allow contaminants from the ground to get on the hands. VA researchers designed a wheelchair with separate push rims connected to the wheels with a bicycle chain. The intent was to improve shoulder ergonomics. The researchers measured bacteria on the hands of volunteers using both the new design and standard wheelchairs in a hospital. Bacterial counts on the hands were 10-fold lower using the ergonomic wheelchair. The results show that this new design can keep wheelchair users’ hands cleaner in addition to improving shoulder ergonomics, according to the researchers. (Disability and Rehabilitation: Assistive Technology, July 3, 2020)
|
Racial disparity in sleep apnea treatment adherence
 Photo: ©iStock/yelo34 (07/16/2020)
Black patients were less likely than white patients to use prescribed sleep apnea devices, in a VA Greater Los Angeles Healthcare System study. Researchers looked at data on more than 2,000 Veterans diagnosed with obstructive sleep apnea. All patients were prescribed a positive airway pressure (PAP) machine. Black patients were 36% less likely than white patients to adhere to PAP use 30 days after diagnosis. The results suggest health inequality related to sleep apnea, according to the researchers. More research is needed on the cause of this disparity, they say. (Journal of Clinical Sleep Medicine, April 8, 2020)
|
Cirrhosis hospitalizations decline due to COVID-19
 Photo: ©Peter Horrox (07/16/2020)
Hospitalizations for cirrhosis have dropped sharply because of COVID-19, found a study by Corporal Michael J. Crescenz VA Medical Center researchers. They looked at data on more than 7,000 VA patients with cirrhosis in 2019 and 2020. Hospitalizations related to cirrhosis per week were significantly fewer in mid-2020, compared with before the pandemic. Shelter-in-place orders or rates of COVID-19 cases and deaths did not affect the weekly average. The researchers found significantly more end-stage liver disease admissions as the pandemic went on, indicating more severity. This finding suggests cirrhosis patient outcomes are being hurt by the pandemic, say the researchers. The study also showed that as the pandemic went on, academic hospital admissions, length of stay, and hospital transfers all decreased. These changes likely reflect efforts to preserve inpatient resources, and guidance urging people to stay home, say the researchers. How these patients are being managed as outpatients is unclear, but it is likely they do not currently have adequate health care access, say the researchers. They add that the findings parallel changes seen in other resource-intensive conditions, such as congestive heart failure. (Gastroenterology, May 6, 2020)
|
Trauma exposure worsens work-related outcomes in women Veterans
 Photo: ©iStock/PeopleImages (07/09/2020)
Women Veterans who experienced trauma had worse work-related outcomes, in a study by VA Boston researchers. More than 350 women Veterans answered surveys about trauma experiences and work. Participants reported high rates of trauma exposure. Nearly half were not working. Military-related trauma, military sexual assault, and adult sexual assault were all linked to worse job functioning. Participants with PTSD and depression related to trauma were less likely to be employed than those without these conditions. The results highlight the need to screen for trauma exposure and address work-related needs of women Veterans, say the researchers. (International Journal of Environmental Research and Public Health, June 25, 2020)
|
Telehealth adherence in patients with heart failure
 Photo: ©iStock/FG Trade (07/09/2020)
VA researchers identified factors that added to home telehealth adherence for patients with heart failure. The researchers studied data on Veterans with heart failure in the VA Home Telehealth Program at several time points after enrollment. Patients in the program are expected to participate in daily monitoring of their symptoms and health. The researchers found that participation increased the longer patients remained in the program. Being older and not having depression were also associated with greater program adherence. Black and other non-white patients had lower adherence, compared with white patients. The findings can help target patients who need more encouragement to use the program, according to the researchers. (Journal of Gerontological Nursing, July 1, 2020)
|
Statin use linked to lower risk of death in older patients
 Photo: ©iStock/rogerashford (07/09/2020)
Taking statins was linked to lower risk of death in older patients, in a study by VA Boston Healthcare System researchers. Statins are medications for lowering cholesterol. Until recently, medical guidelines recommended halting statin therapy at age 75. The study of more than 300,000 Veterans using VA health care found that people 75 and older without heart disease who were prescribed a statin had a 25% lower risk of all-cause mortality and a 20% lower risk of heart-related death, compared with those not on the drug The results suggest that age is not a reason to not prescribe statins, say the researchers. (JAMA, July 7, 2020)
|
Treadmill training helps correct walking problems in prosthetic users
 Photo: ©iStock/JohnnyGreig (07/06/2020)
Split-belt treadmill walking can help people with prosthetic legs correct gait asymmetry, found a VA Eastern Colorado study. People who use a prosthetic leg because of an amputation often have trouble taking the same sized step with both legs. Researchers had participants with gait asymmetry walk on a treadmill with separate belts for each leg. When each belt was moving at a different speed, participants were able to adjust their gait. They were able to maintain this adaptation after the belts were returned to the same speed, creating more symmetry in their gait in the short term. The results show that adapting step-length symmetry is possible without modifying the prosthetic limb, say the researchers. (Gait & Posture, May 31, 2020)
|
Hormone biomarkers give insight into PTSD treatment response
 Photo: ©iStock/Mikhail Artamonov (07/06/2020)
A VA study showed that biomarkers could be used to tell which patients are likely to respond well to PTSD treatment. Researchers studied function of the neuroendocrine system—which regulates hormones—in patients undergoing prolonged exposure therapy for PTSD. Prolonged exposure therapy involved confronting traumatic memories, and is one of the gold standards in PTSD treatment. The researchers found that higher cortisol levels during therapy was linked to more severe PTSD. They also found that baseline levels of three hormones, allopregnanolone, pregnanolone, and cortisol, could predict how well patients reacted to treatment. Higher levels of these hormones before prolonged exposure were linked to greater reductions in PTSD. The findings suggest that neuroendocrine biomarkers could be used to monitor PTSD treatment response, according to the researchers. (Psychoneuroendocrinology, June 8, 2020)
|
Frailty linked to low bone mineral density in men
 Photo: ©iStock/PIKSEL (07/06/2020)
Frailty is associated with lower bone mineral density in males, found a study by VA researchers and colleagues. Frailty refers to increased vulnerability and weakness due to age. It is often linked to poor health, including low bone mass and fracture risk. Researchers assessed frailty and bone mineral density in both male and female patients with rheumatoid arthritis. They found that women had a higher rate of frailty than men. However, frailty was associated with low bone mineral density only in male patients. The results suggest that sex may influence the relationship between bone mineral density and frailty. (Bone Reports, May 22, 2020)
|
Opioid misuse common in older adults
 Photo: ©iStock/Aleksandr_Gromov (06/23/2020)
Opioid misuse is common in older adults, found a study by Providence VA researchers and colleagues. Most research on opioid misuse focuses on younger people. The researchers studied Medicare data on more than 7 million patients over the age of 65 to find opioid use disorder rates. In the year studied, 1% of patients had opioid use disorder documented on a hospital claim. Among this group, 17% had opioid use disorder as the primary diagnosis, and 83% had it as a secondary diagnosis. One in five opioid-related hospitalizations were for overdose. Given the high prevalence, more research is needed on the needs of older adults with opioid use disorder, say the researchers. (Journal of the American Medical Directors Association, April 2020)
|
Exercise training reduces protein linked to muscle pain
 Photo: ©iStock/Mary Swift (06/23/2020)
A study by Iowa City VA researchers explored the biological process behind muscle pain caused by exercise. Pain can often limit how much exercise people can engage in. Researchers found that mice undergoing high-intensity interval training had less immediate pain after exercise, based on brain scans. These mice had lower levels of proteins called acid-sensing ion channels (ASICs) in neuron cells. The researchers also found that mice that genetically did not produce the ASIC protein did not experience immediate exercise-induced muscle pain. The results suggest that pain after exercise is linked to ASICs. They also suggest that high-intensity exercise training reduces ASIC production, thereby reducing muscle fatigue. Low-intensity exercise was not linked to less ASIC. The findings help explain why training increases exercise capacity, according to the researchers. (Journal of Applied Physiology, May 28, 2020)
|
Less sleep time may predict higher chance of dementia
 Photo for illustrative purposes only. ©iStock/amenic181 (06/23/2020)
Total sleep time may be a useful biomarker of dementia, according to a Michael E. DeBakey VA Medical Center study. Researchers studied data from nearly 70,000 sleep studies conducted over a 20-year period in VA. They found that lower total sleep time predicted greater odds of dementia diagnosis in patients. The study suggests that less than 360 minutes (six hours) per night is a good cut-off to predict greater odds of dementia. This cut-off could help clinicians assess a patient’s risk of dementia, say the researchers. (Sleep, May 27, 2020)
|
Mental health treatment improves lung cancer outcomes
 Photo: ©iStock/Chinnapong (06/16/2020)
Treatment for mental health disorders led to better outcomes in patients with lung cancer, found a study by San Francisco VA researchers and colleagues. Researchers looked at data on more than 55,000 Veterans diagnosed with non-small cell lung cancer. About 18,000 had pre-existing mental health disorders. Among this group, those in mental health treatment programs were less likely to be diagnosed at a later stage of their cancer and were more likely to receive stage-appropriate cancer treatment, compared to those not in mental health treatment. They were also less likely to die from lung cancer or any other cause during the study period. Participation in housing and employment support programs was also linked to similar cancer outcome improvements. The results show that investing in mental health and social needs can improve other aspects of health such as cancer, say the researchers. (JAMA Oncology, June 4, 2020)
|
Prolonged exposure therapy reduces trauma-related guilt
 Photo: ©iStock/kieferpix (06/16/2020)
Prolonged exposure therapy for PTSD and substance use disorder reduces feelings of guilt, according to a VA study. PTSD is often accompanied by trauma-related guilt, which is usually related to negative views of one’s actions or inactions during a traumatic event. Researchers assessed guilt in more than 100 Veterans with both PTSD and SUD. Half received prolonged exposure therapy designed to treat both conditions together. The rest received therapy focusing on coping skills. The prolonged exposure group reported significantly lower guilt over time, compared to the other group. The results show that exposure-based treatment for both PTSD and SUD is more effective at reducing guilt than non-exposure treatment, conclude the researchers. (Journal of Traumatic Stress, June 10, 2020)
|
Patient-aligned care teams help keep patients in VA care
 Photo for illustrative purposes only. ©iStock/FatCamera (06/16/2020)
Patient-aligned care teams (PACTs) positively affect patient use of VA health care, found a study of data on 1.5 million patients. PACTs are a team-based approach to care that involves the patient in decision-making. The model focuses on easy access to care, care coordination, better communication, and self-management. Researchers used a quality measure of how well PACTs had been implemented at each VA primary care practice. Patient attrition was lower in practices with higher PACT implementation scores, compared to those with worse implementation. Out of the 1.5 million patients, 4.4% dropped out of care during a two-year follow-up. At the lowest-scoring PACT locations, this rate was 4.8%. At the highest-scoring locations, the attrition rate was 4.0%. The results show that better PACT implementation positively affects patients’ decisions to stay in VA care. (Healthcare, June 2020)
|
Psychotic symptoms linked to solitary confinement in incarcerated individuals
 Photo: ©iStock/Rattankun Thongbun (06/03/2020)
Incarcerated people with psychotic symptoms are more likely to be placed in solitary confinement, found a Maryland VA researcher and colleague. People with psychiatric disorders are disproportionately represented in the U.S. prison system. The researchers surveyed 176 previously incarcerated people. Those with a schizophrenia diagnosis or psychotic symptoms were more than twice as likely to have been placed in solitary confinement, compared to those without psychiatric conditions. More research is needed to determine whether prisoners are placed in solitary confinement based solely on behaviors related to psychiatric illness, according to the researchers. Such action could violate the Americans with Disabilities Act, they say. (Psychiatry Research, May 21, 2020)
|
Secure messaging from clinicians improves diabetes patient self-management
 Photo: ©iStock/fizkes (06/03/2020)
Diabetes patients who received online messaging support from their clinicians better self-managed their care, in a study by researchers at the Edith Nourse Rogers Memorial Veterans Hospital in Massachusetts. Secure messaging over the internet allows doctors and patients to communicate in between visits. The study included more than 400 Veterans with diabetes who used VA’s My HealtheVet online patient portal. Patients who received at least one proactive message about their care were more likely to engage in better diabetes self-management, compared to patients who were not messaged. They also reported a higher sense of self-confidence. Proactive communication from clinical teams can foster a patient’s sense of autonomy and encourage better self-care, conclude the researchers. (Journal of General Internal Medicine, May 21, 2020)
|
Blood thinner linked to higher fracture risk
 Photo: ©iStock/Hailshadow (06/03/2020)
Atrial fibrillation patients taking the blood thinner warfarin had a higher risk of fractures than patients taking other blood-thinning drugs, in a study by Minneapolis VA researchers and colleagues. Atrial fibrillation is an irregular heart rate that causes poor blood flow. Patients with the condition are often prescribed blood thinners (anticoagulants) to prevent stroke and other problems. Some evidence has shown that the common anticoagulant warfarin may be linked to poor bone health. The researchers looked at data on nearly 170,000 patients with atrial fibrillation. They found that patients taking warfarin were more likely to have bone fractures, compared to those taking newer oral anticoagulants. This difference was especially high in patients with osteoporosis. The drug apixaban had the lowest fracture risk. The findings suggest that caution should be used when prescribing warfarin to patients with a high risk of fracture, say the researchers. (JAMA Internal Medicine, February 2020)
|
Blood pressure variability linked to heart failure risk
 Photo: ©iStock/LumiNola (05/28/2020)
Blood pressure variability is associated with heart failure risk in people with diabetes, according to a study by VA researchers. Blood pressure variability is known to be a risk factor for cardiovascular disease. But its relationship with heart failure is less clear. The study found that variability in both systolic and diastolic blood pressure was connected to increased risk of heart failure. Variability increased the risk independently of elevated average blood pressure. The effects of blood pressure variability appear to be related to dips in pressure, not with elevations. The results will help optimize blood pressure treatment in patients with diabetes, according to the researchers. (Diabetes Care, April 23, 2020)
|
Parkinson’s patients with sleep disorder have poorer mental function
 Photo for illustrative purposes only. ©iStock/adamkaz (05/28/2020)
Disordered sleep was linked to poorer mental function in patients with Parkinson’s disease, found a VA San Diego study. Many patients with Parkinson’s disease are affected by rapid eye movement sleep behavior disorder. Researchers compared cognitive performance between Parkinson’s patients with and without the sleep disorder. Those with disordered sleep had poorer executive functioning and learning performance. They also had poorer neuropsychological functioning across all cognitive domains. Those with sleep disorder also showed poorer medication management skills. The results underscore the importance of assessing for sleep disorder in patients with Parkinson’s disease, say the researchers. (Journal of the International Neuropsychological Society, May 7, 2020)
|
HIV linked to lung impairment
 Photo: ©iStock/yodiyim (05/28/2020)
HIV-positive men were at increased risk of lung impairment, found a study including a Minneapolis VA researcher. Previous studies have suggested that HIV may increase the risk of chronic lung diseases. The researchers compared several measures of lung function in men with and without HIV infection. Those with HIV had worse defusing capacity, the ability of oxygen to pass from the lungs into the blood. Worse defusing function has been linked to worse quality of life, worse exercise capacity, and higher risk of respiratory disease. HIV status did not affect forced expiratory volume, a measure of how much air can be exhaled during a forced breath. The impairment of the gas defusing capacity may be behind a higher risk of respiratory diseases in men with HIV, according to the researchers. (AIDS, April 13, 2020)
|
PTSD suppresses the brain’s immune system
 Photo: iStock/JohnnyGreig (05/21/2020)
A study by VA Connecticut and Yale University researchers showed how PTSD is linked with neuroimmune suppression. The researchers compared brain scans of 23 patients with PTSD and 26 without. They found that patients with lower levels of a protein TSPO in the prefrontal-limbic part of the brain had worse PTSD symptom severity. This protein is a biomarker for activation of microglial cells, the brain’s first form of immune defense. Those with PTSD had significantly lower TSPO levels than those without PTSD. Those with lower TSPO concentration also had higher levels of C-reactive protein, a protein that is increased when inflammation is present in the body. The findings suggest that PTSD hinders the function of the immune system in the brain, according to the researchers. (Nature Communications, May 12, 2020)
|
Veterans from lower ranks less likely to use mental health care
 Photo: iStock/SDI Productions (05/21/2020)
Veterans from lower ranks were less likely to use VA mental health care, found a VA study. Researchers analyzed data on almost 10,000 post-9/11 Veterans. Of those, 34% had at least one mental health condition. Veterans from junior enlisted ranks were significantly less likely than those from higher ranks to use mental health programs and services. Use of these services was similar between male and female Veterans. The study also showed more similarities than differences in mental health care use between Veterans of different racial/ethnic backgrounds. Veterans exposed to combat, with a medical discharge, or with ongoing medical conditions were much more likely to use VA health care services. The results highlight the need to encourage Veterans from lower ranks to seek mental health services, say the researchers. (Psychiatric Services, May 12, 2020)
|
Adding social workers to primary care teams reduces emergency room visits
 Photo: iStock/peakSTOCK (05/21/2020)
Including social workers on VA primary care teams reduced emergency room visits, found a study led by Providence VA Medical Center researchers. The study looked at the effects of adding social workers to rural primary care teams in VA facilities. Results showed that, among high-risk patients, introducing a social worker decreased emergency department visits by 3%. Acute hospital admissions declined by 4.4%. Among all Veterans receiving care at these facilities, social work encounters increased by 33% after social workers were integrated into primary care teams. The results show that including social workers in care is a key strategy to improve care coordination for high-risk patients, say the researchers. (Health Affairs, April 2020)
|
PTSD may increase risk of autoimmune diseases
 Photo: iStock/KenTannenbaum (05/13/2020)
Service members with PTSD may have a higher risk of autoimmune diseases, found a VA-funded study of active duty personnel. As part of the Millennium Cohort Study, researchers looked at data on more than 120,000 service members. They found that those with a history of PTSD had a 58% higher chance of having an autoimmune disease. Autoimmune diseases included rheumatoid arthritis, lupus, inflammatory bowel diseases, and multiple sclerosis. The connection between PTSD and autoimmune diseases was independent of combat experience or prior trauma. The results add to growing evidence that PTSD is a risk factor for autoimmune disease, say the researchers. (BMC Psychiatry, Jan. 15, 2020)
|
PTSD and alcohol use disorder feed into each other
 Photo: iStock/axelbueckert (05/13/2020)
PTSD and alcohol use disorder can feed into one another and make both worse, according to a VA San Diego study. PTSD and alcohol use disorder often occur together. Researchers studied symptoms in 107 Veterans being treated for PTSD and alcohol use disorder. They found that greater PTSD symptom severity was linked with greater future alcohol use. Likewise, greater alcohol use was linked with greater future PTSD symptom severity. The effect of PTSD on drinking was higher than the other way around. The findings support the idea of mutual maintenance between PTSD and alcohol use. Integrated treatments for both PTSD and alcohol use may be better than expecting patients to reduce alcohol use before beginning trauma-focused treatment, say the researchers. (Psychology of Addictive Behavior, Feb. 27, 2020)
|
Migraine genetically linked to other health conditions
 Photo: iStock/g-stockstudio (05/13/2020)
Migraine headaches have a shared genetic basis with multiple other conditions, found a study including several VA researchers. The study used data from the UK Biobank, a large repository of genetic information. Researchers found that people with migraine had similar gene variants as those with many other conditions, including heart disease, high cholesterol, and autoimmune diseases. The results confirm past studies suggesting a connection between these conditions. The researchers also identified a genetic similarity between migraine and Type 2 diabetes risk, a connection that had not been identified previously. Notably, the data showed that blood pressure directly contributes to migraine, suggesting that high blood pressure may partially cause migraines in addition to sharing genetic risk factors. (International Journal of Epidemiology, April 19, 2020)
|
Elective percutaneous coronary interventions in VA largely appropriate
 Photo: iStock/adventtr (05/06/2020)
Most procedures for stable coronary artery disease in VA medical centers were appropriate, found a study by Rocky Mountain Regional VA and VA Puget Sound researchers. Percutaneous coronary interventions involve treating narrowing arteries with angioplasty or stenting. In patients with stable coronary artery disease, these interventions can relieve symptoms but do not increase survival. They also may cause complications such as bleeding, kidney injury, stroke, or death. Researchers looked at data on these procedures in 59 VA medical centers over a two-year period. They found that 30% of elective procedures were classified as appropriate, and 60% as “may be appropriate.” About 10% were deemed “rarely appropriate.” While most procedures were appropriate or possibly appropriate, efforts to improve patient selection are still needed, according to the researchers. (JAMA Network Open, April 1, 2020)
|
Many Veterans prefer virtual health care visits
 Photo: iStock/SDI Productions (05/06/2020)
Many patients using VA-issued tablets preferred video health care to in-person care, found a VA Palo Alto study. In 2016, VA began issuing tablets to Veterans to allow them to receive care virtually. The program aimed to improve care access for Veterans who face barriers such as transportation issues. Researchers surveyed about 600 tablet recipients about their experiences with telehealth. Satisfaction with the tablet program was high. Almost a third of patients said they preferred virtual care to in-person visits, while 36% said care was “about the same.” Patients were more likely to prefer video visits if they felt uncomfortable in a VA setting, had communicated well with their doctor, had substance use disorder, or lived in a place with better broadband coverage. Patients with more chronic conditions were less likely to prefer video visits. The results will help identify which patients would benefit from virtual care, say the researchers. (Journal of Medical Internet Research, April 15, 2020)
|
Survey: Majority of women Veterans feel welcome at VA
 Photo: iStock/monkeybusinessimages (05/06/2020)
Researchers surveyed women Veterans at 26 VA locations. Out of more than 1,000 women, 85% said they felt welcome at VA. Not quite a third of the women surveyed answered an open-ended prompt about their experience with VA. Of those, 26% told of feeling uncomfortable or being harassed at a VA facility. Suggestions to improve VA included providing additional resources and clinical services for women Veterans, changing male Veterans’ behavior toward women, and making treatment of women and men the same. Although most women Veterans felt welcome in VA, opportunity exists to make them more comfortable and improve their experience in VA, say the researchers. (Women’s Health Issues, April 24, 2020)
|
High-dose folic acid may improve diabetic foot ulcer healing
 Photo: iStock/MangTeng (04/29/2020)
High-dose folic acid may improve diabetic foot ulcer healing, found a Hunter Holmes McGuire VA Medical Center study. Researchers reviewed the charts of 29 Veteran patients with chronic, non-healing diabetic foot ulcers who were treated with high-dose folic acid. Of the study group, 90% saw complete wound closure after folic acid treatment. The researchers also compared the wound healing rate of four subjects with patients who had not received high-dose folic acid. Over a four-week period, the patients treated with folic acid showed significant improvements, compared with the non-treated group. The researchers recommend larger randomized clinical trials to establish how effective high-dose folic acid is at treating diabetic foot ulcers. (Wound Repair and Regeneration, March 5, 2020)
|
Shifting risk factors for cirrhosis
 Photo: iStock/Rasi Bhadramani (04/29/2020)
The most common risk factors for cirrhosis may have shifted, found a study by Michael E. DeBakey VA Medical Center researchers. Previous studies identified active viral infection with hepatitis B or C as the most common risk factors for cirrhosis and liver cancer. In this study, researchers looked at more than 1,000 patients with cirrhosis. They found that the most common cirrhosis and liver cancer risk factors had shifted to resolved hepatitis C and fatty liver disease. They also found racial and ethnic differences in risk factors. Hispanic patients with cirrhosis were more likely to have obesity, diabetes, and non-alcoholic fatty liver disease, compared with other groups. These risk factors were less common in black patients. Black patients had higher rates of alcoholic liver disease and heavy alcohol drinking than other groups. The results suggest that minorities may still face a higher burden of chronic liver disease, say the researchers, and that multiple risk factors should be examined to monitor for cirrhosis. (Gastroenterology, March 29, 2020)
|
High-dose flu vaccine may improve response in rheumatoid arthritis patients
 Photo: iStock/SDI Productions (04/29/2020)
High-dose flu vaccines posed no risk and offered some benefits to patients with rheumatoid arthritis, found an Iowa City VA study. People with rheumatoid arthritis taking arthritis medications are at risk for severe cases of the flu and may not respond well to the flu vaccine. Rheumatoid arthritis patients were given either a standard or high dose of the flu vaccine. High-dose patients had a higher antibody response, although the difference was small. Neither group showed any safety concerns. Although larger studies are needed, high-dose flu vaccines may be a good option for rheumatoid arthritis patients considering their increased flu risk, say the researchers. (Vaccine, April 12, 2020)
|
PTSD increases women Veterans’ risk of heart disease
 Photo for illustrative purposes only. ©iStock/patrickheagney (04/23/2020)
PTSD significantly increased the risk of ischemic heart disease in woman Veterans, found a VA Greater Los Angeles Health Care System study. In ischemic heart disease, the heart does not get enough blood because of plaque in the arteries. It is the most common type of heart disease. Researchers looked at data on women Veterans visiting VA medical centers between 2000 and 2017. Out of more than 800,000 women, about 18% had PTSD. These women had significantly higher risk for ischemic heart disease, compared with women without PTSD. This risk was independent of age, obesity, alcohol use, and other factors related to heart disease. Previous research has linked PTSD with ischemic heart disease in men, but studies in women have been limited. The researchers recommend early and routine screening for ischemic heart disease in women Veterans with PTSD. (Journal of the American College of Cardiology, March 2020)
|
Opioid agonist therapy infrequent in VA
 Photo: ©iStock/Hailshadow (04/23/2020)
Opioid agonist therapy is delivered infrequently in VA hospitals, found a study by VA Portland researchers and colleagues. Opioid agonists are medications, such as methadone and buprenorphine, that help prevent withdrawal from and cravings for opioids. Researchers looked at data on more than 12,000 patients with opioid use disorder who were hospitalized at a VA facility. Only 15% received opioid agonists, mostly to help with withdrawal symptoms. Just 2% began agonist treatment after discharge. Treatment delivery frequency varied across the health system. The results show that policy and educational steps should be taken to promote hospital-based opioid agonist therapy, say the researchers. (Journal of General Internal Medicine, April 14, 2020)
|
Brain activity relation to emotions could predict PTSD treatment response
 Photo: ©iStock/alvarez (04/23/2020)
How well patients respond to PTSD treatment may be linked to how regions of the brain activate and connect with other regions, according to a VA study. Researchers used MRI to study brain signals in Veterans with PTSD. Patients were treated with either prolonged exposure therapy, medication, or both and compared to a control group. Results showed that patients with greater activation in brain regions related to emotional processing and modulation before treatment responded better to all types of treatment. Greater connectivity between brain regions involved in attention and emotional processing also positively affected PTSD improvement. The findings suggest that measuring how these brain regions function could help predict PTSD treatment response, according to the researchers. (Depression and Anxiety, April 19, 2020)
|
Editorial: Pandemic could increase suicide risk
 Photo for illustrative purposes only. ©iStock/Marjan_Apostolovic (04/16/2020)
An editorial by VA Puget Sound psychologists warns that COVID-19 may lead to increased risk of suicide. The “secondary consequences” of social distancing could put people at higher risk. These consequences include economic stress, social isolation, decreased community support, and barriers to mental health treatment. Increased national anxiety linked to 24/7 news coverage and a surge in U.S. gun sales could also raise the suicide risk for some, say the researchers. The editorial suggests several steps to improve suicide prevention during the crisis. Staying socially connected by telephone and video can help ease feelings of isolation. Efforts to increased access to mental health care, especially using telemedicine, could give at-risk patients the support they need. The authors also offer an optimistic view of one possible result of the pandemic. Suicide rates have historically declined after national disasters and tragedies such as the 9-11 terrorist attacks. It is possible that pulling together when facing trying times can strengthen social connectedness and make people feel that life is more precious, say the researchers. (JAMA Psychiatry, April 10, 2020)
|
Prolonged exposure therapy could improve sexual desire problems
 Photo: ©iStock/vadimguzhva (04/16/2020)
Prolonged exposure therapy for PTSD could improve sexual desire problems, found a study that included an Atlanta VA researcher. People with PTSD often report difficulties with sexual functioning, including sexual desire. The researchers assessed nearly 200 Veterans who were undergoing prolonged exposure therapy for PTSD. They found that patients who saw PTSD symptom improvement also experienced improved sexual desire. Those who did not respond to the treatment did not see sexual desire improvements. Patients with severe depression at the start of treatment showed less sexual desire improvement than patients without depression, regardless of PTSD improvement. The results suggest that prolonged exposure could help with PTSD-related sexual desire problems. (Psychiatry, April 1, 2020)
|
Spiritual difficulties may increase suicidal thoughts
 Photo for illustrative purposes only. ©iStock/PeopleImages (04/16/2020)
Spiritual difficulties were linked with increased suicidal thoughts, in a Durham VA study. Researchers collected data on religion and spirituality for a thousand Iraq and Afghanistan Veterans. They found that perceived lack of control and problems with self-forgiveness increased the risk of suicidal thoughts. Perceived punishment by God and a lack of meaning or purpose significantly increased the risk of suicide attempts. The results suggest that screening for spiritual difficulties, possibly in collaboration with chaplains, could help detect Veteran suicide risk, according to the researchers. (Depression and Anxiety, April 5, 2020)
|
Study: Patient outcomes similar with nurse practitioners or physicians
 Photo for illustrative purposes only. ©iStock/GlobalStock (04/10/2020)
VA patients with a nurse practitioner as their primary care provider (PCP) had similar health outcomes as those with a medical doctor as the PCP, found a VA Puget Sound study. Researchers looked at data on over 800,000 VA patients who had originally been assigned a doctor as their PCP. Each patient’s PCP had left VA practice, meaning the patient was then reassigned to either a doctor or nurse practitioner. The researchers found little difference between the two groups for clinical outcomes, costs, and receipt of diagnostic tests. Patients reassigned to a nurse practitioner were less likely to use primary or specialty care services, but still had similar health results. The study confirms that nurse practitioners offer a cost-effective way to address anticipated shortages of primary care physicians, say the researchers. (Health Services Research, April 2020)
|
Mind-body skills intervention improves PTSD symptoms
 Photo: ©iStock/PeopleImages (04/10/2020)
A mind-body skills group significantly improved patients’ PTSD symptoms, in a study at the Southeast Louisiana VA. A group of 108 Veterans with PTSD received 10 weeks of either the mind-body skills intervention along with standard treatment, or standard treatment only. The mind-body program included meditation, guided imagery, biofeedback, and group support. Standard treatment consisted of trauma-focused psychotherapy. Patients in the mind-body group had significantly better PTSD improvement compared with the control group. They saw improvements in hyperarousal and avoidance that lasted at least two months after treatment, as well as decreased anger and sleep disturbances. The findings show that the mind-body skills intervention offers promise for relieving PTSD symptoms, according to the researchers. (Psychological Trauma, March 5, 2020)
|
Stem cells accelerate diabetic wound healing in mouse model
 Photo: ©iStock/dra_schwartz (04/10/2020)
Stem cells could accelerate diabetic wound healing, found a study that included a VA Connecticut researcher. The team embedded human smooth muscle cells derived from stem cells into a 3-D collagen scaffold. They then placed the scaffold into diabetic wounds on mice. The stem-cell implantation increased concentrations of biological products involved in wound healing. The stem cells accelerated the healing process, compared to control wounds not treated with the scaffold. While the technique has to be studied further, say the researchers, it is a promising potential therapy for diabetic wounds. (Regenerative Medicine, March 31, 2020)
|
Patient hassles lead to delayed or skipped care
 Photo for illustrative purposes only. ©iStock/DjelicS (04/02/2020)
Health care hassles greatly increase patients’ likelihood of delaying or forgoing care, according to a VA Greater Los Angeles study. Researchers surveyed women Veterans receiving care at 12 VA medical centers. They found that 39% reported four or more hassles to obtaining care, while 26% reported no hassles. Hassles included the work a patient must do to get questions answered between appointments or to navigate pharmacy, testing, and specialty services. Patients who said they faced four or more hassles were five times more likely to delay or skip care, compared to those with no hassles. Improving communication and coordination hassles is an important step in improving patients’ access to care, say the researchers. (Healthcare (Amsterdam, Netherlands), Feb. 29, 2020)
|
Gender differences in newly separated Veterans’ health care use
 Photo for illustrative purposes only. ©iStock/Human Role (04/02/2020)
Researchers from the VA Central Western Massachusetts Healthcare System identified gender differences in newly separated Veterans’ health care use. They surveyed nearly 50,000 Veterans about 90 days after military separation and then again a year later. Results showed that sleep problems, anxiety, and depression were linked to greater health care use for both men and women. Women were twice as likely as men to use health care in general. However, men and women were equally likely to use VA care. For women Veterans, unstable housing at separation was linked with less health care use a year later, especially for those with mental health issues. The results suggest that VA needs to do more to reach out to women Veterans considering that they are more likely to use health care than men but not more likely to use VA care, say the researchers. One way to improve this disparity, they say, may be housing assistance programs targeting women. (American Journal of Managed Care, March 2020)
|
Infectious disease specialist consultation improves long-term S. aureus outcomes
 Photo: ©iStock/South_agency (04/02/2020)
Infectious disease consultation improves long-term outcomes for patients with Staphylococcus aureus bacteremia, found an Iowa City VA study. Bacteremia is when the bacterial infection makes it into the bloodstream. Studies have shown that 15% to 30% of patients with S. aureus bacteremia die within 30 days. They also have high rates of infection recurrence. Researchers studied data on more than 30,000 VA patients who had the infection. About half of the patients had a consultation with an infectious disease specialist during their initial hospital stay. These patients were 23% less likely than patients who had not had a consultation to die from any cause in the five years after hospitalization. They were also 32% less likely to have a bacteremia recurrence five years later. The results suggest that consulting infectious disease specialists improves patients’ long-term health, say the researchers. (JAMA Network Open, Feb. 5, 2020)
|
Trust of electronic health records sharing differs by race
 Photo for illustrative purposes only. ©iStock/DragonImages (03/19/2020)
Patient views on sharing electronic health records differed by race, in a study of nearly 20,000 Veterans. Currently, VA patients must opt in to allow their electronic health records to be shared with outside health care providers. But as VA transitions to a new electronic health record system, it is switching to an opt-out model to make data-sharing easier. In the opt-out model, patient data can be shared with other health care providers unless the patient withdraws consent. Researchers surveyed patients about their preferences for providing data-sharing consent. A majority of white patients, 57%, preferred an opt-out policy. But patients of other races were less likely to prefer the opt-out model: 48% of Asian/Pacific Islander patients, 45% of Hispanic patients, 40% of black patients, and 38% of Native American patients preferred this policy to opt-in. The results show that cultural sensitivity and trust must be considered during the electronic health records implementation, say the researchers. (Journal of the American Informatics Association, March 9, 2020)
|
Hoarding treatment shows promise
 Photo: ©iStock/Dennis Torkhov (03/19/2020)
A community-based intervention for hoarding disorder shows promise, found a VA San Diego study. Hoarding refers to compulsively acquiring and saving large quantities of things, and it can often impede daily living. It is much more common in older adults than younger people. Researchers tested a treatment called Cognitive Rehabilitation and Exposure/Sorting Therapy (CREST). During an initial two-year program, 15 out of 37 participants completed the program. In those 15, there was significant improvement in hoarding severity and clutter volume. After the initial test, the program was expanded to reach more patients. The results suggest that CREST can be successfully used in the community with positive results, according to the researchers. (International Psychogeriatrics, March 5, 2020)
|
Many providers unaware of COPD treatment guidelines
 Photo for illustrative purposes only. ©iStock/nimis69 (03/19/2020)
Many primary care providers in VA are unaware of recommendations for treating chronic obstructive pulmonary disease, found a VA study. Inhaled corticosteroids are recommended for COPD only when patients have frequent exacerbations. But more than 50% of Veterans with mild to moderate COPD are prescribed the medication. A survey of primary care providers at 13 VA facilities found that providers are largely unaware of current evidence and recommendations. For example, 46% of those surveyed did not know of the risk of pneumonia caused by corticosteroids. Providers said they were unable to keep up with current literature because of the broad scope of practice. Many were also reluctant to change prescriptions from other doctors. The results support the idea that lack of awareness on guidelines is an important part of corticosteroid overuse, say the researchers. (Journal of General Internal Medicine, January 2020)
|
Augmentee status and mental health risk in women service members
 (U.S. Army Reserve photo by Master Sgt. Michel Sauret,for illustrative purposes only.) (03/12/2020)
Women in the Reserves or National Guard who deploy on temporary duty assignments without their home unit may be at higher risk of mental health problems than those who serve in their regular units. Researchers with the Central Arkansas and Iowa City VA health care systems surveyed women who deployed to Iraq or Afghanistan as individual-augmentees. Individual-augmentees are service members who deploy with a unit other than their regular one. Compared to women who deployed with their home unit, these women were more likely to experience depression, PTSD, and binge drinking. Women in the Reserves or National Guard also had higher mental health risk than active duty women. Prior studies have found similar results in men. The results suggest that particular focus should be given to the mental health risks of Reserve/Guard women who deploy as individual-augmentees, say the researchers. (Women’s Health Issues, Feb. 18, 2020)
|
Antimicrobial hospital curtains fall short in curbing contamination
 Photo: ©iStock/pixelci (03/12/2020)
Antimicrobial curtains did not reduce hospital room contamination in an Iowa City VA and University of Iowa study. Researchers compared the microbe levels on hospital room privacy curtains in an intensive care unit. Some rooms had standard curtains, while others had curtains impregnated with halamine, an antimicrobial polymer. The rooms with antimicrobial curtains did not have lower contamination levels than the rooms with standard curtains. Antimicrobial curtains that were sprayed twice weekly with disinfectant had lower microbe levels than unsprayed antimicrobial curtains, but the effect lasted only 72 hours. Further study is needed to find out what, if any, effect antimicrobial curtains have on infection rates, according to the researchers. (American Journal of Infection Control, March 2, 2020)
|
Exercise boosts quality of life after liver transplant
 Photo for illustrative purposes only. ©iStock/Yuri_Arcurs (03/12/2020)
Exercise can improve quality of life after a liver transplant, found a review including a VA Pittsburgh researcher. Physical fitness and frailty often improve slowly and may even deteriorate after a liver transplant. Based on a review of the available literature, researchers found that an exercise program can improve both fitness and quality of life for transplant patients. In addition to combating muscle loss and frailty, exercise can counteract post-transplant metabolic syndrome, which causes complications such as diabetes and hypertension. Exercise can improve post-transplant quality of life through both better health and increased social support. The researchers suggest that a tailored exercise program be part of post-transplant care. (Liver Transplant, March 3, 2020)
|
Quality of life improvements for PTSD patients differ by gender
 Photos for illustrative purposes only. ©iStock/ Petko Ninov; DigitalSkillset (03/06/2020)
How PTSD treatment improves quality of life differs in men and women patients, found a study by VA San Diego researchers. While cognitive processing therapy has been shown to improve PTSD symptoms, the treatment’s effect on quality of life is less well-understood. The study looked at quality of life outcomes of men and women undergoing this treatment. Results showed that a reduction in depression symptoms was most likely to improve quality of life for women with PTSD. For men, reduced feelings of anger best predicted quality of life improvements. The findings suggest that the effectiveness of PTSD treatment should be evaluated within the context of gender, say the researchers. (Military Medicine, Feb. 20, 2020)
|
Neurofeedback has potential as schizophrenia treatment
 Photo: ©iStock/leezsnow (03/06/2020)
Neurofeedback could improve cognitive function in patients with schizophrenia, but more study is needed, according to a VA San Diego and University of California at San Diego study. In neurofeedback, patients are able to directly see visual or auditory representations of their own brain activity. It may allow patients to modulate their neural activity. The review found some evidence that neurofeedback can lead to measurable changes in brain function in schizophrenic patients. However, most studies on the subject are either case studies or studies with small sample sizes. Large, randomized clinical trials are needed to validate the effectiveness of neurofeedback in schizophrenia, according to the researchers. (Schizophrenic Bulletin, March 2, 2020)
|
Possible biomarkers of traumatic brain injury identified
 Photo: ©iStock/nicolas (03/06/2020)
VA researchers and colleagues identified six new biomarkers that could possibly be used to identify traumatic brain injury caused by blasts. In a mouse model of blast exposure, the researchers performed two different tests to identify proteins linked to TBI. They found 75 unique proteins present in the thalamus of blast-exposed mice but not in control mice. They also tested the blood and found antibodies linked to 46 proteins in blast-exposed mice. Six of the identified proteins showed up in both tests. These six proteins have potential as biomarkers to identify blast-related TBI through blood tests, say the researchers. (Heliyon, Feb. 17, 2020)
|
Study finds unexpected relationship between social connectedness, depression
 Photo: ©iStock/kali9 (02/27/2020)
A VA Portland study found an unexpected relationship between social connectedness and depression. Researchers surveyed 262 Veterans with depression, asking about social connectedness. Social connectedness comprised social support, interpersonal conflict, loneliness, social norms, and number of confidants. Surprisingly, higher levels of loneliness were linked to decreased depression and suicidal thoughts one year later. A higher number of confidants was linked to increased depression. A more expected result was that higher levels of emotional support led to fewer mental health visits. More study is needed on the seemingly paradoxical relationship between depression and social connectedness, say the researchers. (Social Psychiatry and Psychiatric Epidemiology, Nov. 6, 2019)
|
Online therapy with peer support useful for depression
 Photo for illustrative purposes only. ©iStock/JohnnyGreig (02/27/2020)
An online cognitive behavioral therapy program with peer specialists improved short-term depression symptoms and quality of life for Veterans with depression, in a VA Ann Arbor study. Patients with depression were given either usual care or a computerized cognitive behavioral therapy treatment supported by peer specialists in addition to usual care. Usual care consisted of medication and in-person psychotherapy. The online program included videos, interactive assignments, and symptom self-monitoring, in addition to peer support. Peer specialists were other Veterans who had lived with depression. The treatment group had greater improvement of depression symptoms than the treatment-as-usual group. However, the groups had similar symptoms six months later. The treatment group did have greater improvements in quality of life and mental health recovery three months after treatment. The results show that cognitive behavioral therapy with peer support may be an effective treatment for depression. (Psychological Services, Jan. 14, 2020)
|
Telehealth PTSD treatment as effective as in-person care, but has higher drop-out
 Photo for illustrative purposes only. ©iStock/FatCamera (02/27/2020)
Telehealth is an effective way to deliver PTSD treatment, but it does lead to higher drop-out rates than in-person treatment, found a VA San Diego study. Veteran patients with PTSD received prolonged exposure treatment in one of three ways. Some received treatment at home via teleconferencing. Others received teleconference treatment at a VA facility. For a third group, a therapist traveled to the patient’s home for in-person treatment. All three groups saw similar levels of clinical effectiveness. The results confirm previous studies that found telehealth to be an effective way to treat PTSD. However, patients in the home or office telehealth groups were significantly more likely to drop out of treatment before completion. Patients in the at-home in-person group had lower drop-out rates than the other two groups. The results show that prolonged exposure can be effectively delivered via telehealth, say the research, but that treatment with an in-person element can help curb drop-out. (Depression and Anxiety, Dec. 24, 2019)
|
Study: Increased opioid dose not linked to improved chronic pain
 Photo: ©/Charles Wollertz (02/21/2020)
Increasing opioid dosing does not seem to improve chronic pain, found a study by VA Portland researchers and colleagues. The study followed more then 500 patients with musculoskeletal pain for two years. All patients were on a steady opioid dose at the beginning of the study. About 20% of participants had their opioid dose increased at some point. But only 3% of those patients showed any meaningful improvement in their pain. The entire group showed small improvements in pain intensity and other symptoms, regardless of whether their dose had been increased or not. The results suggest that, while stable doses of long-term opioid therapy can improve pain, higher doses do not lead to better results, according to the researchers. (Pain, Jan 24, 2020)
|
VA patient portal leads to fewer duplicate lab tests
 Photo by Jerry Daliege (02/21/2020)
Use of the MyHealtheVet digital portal decreased duplicate diabetes testing among patient who use more than one type of health care, found an Iowa City VA study. MyHealtheVet is a website that allows Veterans to access their VA health care information. It includes a feature called VA Blue Button, which allows users to download their VA medical records. The researchers studied how using the portal affected HbA1c testing in patients receiving health care from both VA and non-VA providers. Those who used Blue Button at least once were significantly less likely to have duplicate testing. Duplicate testing was defined as more than five HbA1c tests in a year. The results show that the VA patient portal can lead to better information-sharing and less wasteful testing. (Telemedicine Journal and e-Health, Feb. 11, 2020)
|
Mixed results from peer specialists for formerly homeless Veterans
 Photo: ©iStock/kevinruss (02/21/2020)
Peer specialists offered some benefit to formerly homeless Veterans for housing stability, but not behavioral health problems, found a VA study. Researchers looked at outcomes for Veterans in the U.S. Housing and Urban Development-VA Supported Housing (HUD-VASH) program. Participants were assigned peer specialist services or treatment as usual. Peer specialists were other Veterans who had shown significant recovery from mental health issues. They used a structured curriculum to meet with their assigned Veteran participants for up to 40 weeks. Peer meetings focused on mental health, substance use recovery, and community integration. Veterans working with the top-performing peer specialists showed greater housing stability between 400 and 800 days after the program began. However, the overall average time spent in housing for the peer group was not statistically higher than those receiving treatment as usual. Behavioral health problems, such as mental health symptoms and addiction severity, were not affected by the peer specialist program. Further study with more sensitive measures is needed on how beneficial the peer program is to these Veterans, say the researchers. (Medical Care, Jan. 7, 2020)
|
Insight on how subtle cognitive difficulties predict decline
 Photo for illustrative purposes only. ©iStock/fizkes (02/13/2020)
Patients with subtle cognitive difficulties showed signs of brain changes linked to cognitive decline and Alzheimer’s disease, in a study by VA San Diego researchers. They ran PET and MRI brain scans on more than 700 patients. The scans showed that patients with subtle cognitive difficulties had faster amyloid accumulation than cognitively normal patients. Amyloid is a toxic protein. Its build-up in the central nervous system has been linked to Alzheimer’s. Patients with subtle cognitive difficulties also showed thinning of a section of the brain called the entorhinal cortex. Patients with mild cognitive impairment—a more advanced stage of cognitive decline—had faster atrophy in the entorhinal cortex and hippocampus. The findings suggest that objective psychological measures of subtle cognitive difficulties could help identify brain changes before impairment becomes noticeable, say the researchers. (Neurology, Jan. 28, 2020)
|
Sense of purpose may protect against cognitive decline
 Photo: ©iStock/FG Trade (02/13/2020)
Having a sense of purpose in life may protect against cognitive decline, found an Atlanta VA and Emory University study. In a survey of more than 5,000 middle-aged participants, a greater sense of purpose was linked with less perceived cognitive decline. Statistical analysis showed that purpose in life is a strong predictor of cognitive decline when considered along with known protective and risk factors for cognition. Protective factors include education, exercise, and activity levels. Risk factors for cognitive decline include depression, health problems, and smoking. Interventions to enhance purpose in life as early as middle age may be useful, according to the researchers. (Journal of Affective Disorders, Feb. 15, 2020)
|
Benefits of testosterone therapy limited; more research needed
 Photo for illustrative purposes only. ©iStock/FlairImages (02/13/2020)
Testosterone treatment in older men may provide small improvements in sexual functioning and quality of life, but little benefit for other common symptoms of aging, according to a Minneapolis VA review. In men with low testosterone, sexual functioning and quality of life improved after testosterone therapy. However, the improvements were low to moderate. The review found little to no effect of testosterone therapy on physical functioning, depression, energy and vitality, or cognition. Not enough evidence exists to draw conclusions on how testosterone treatment affects cardiovascular events or prostate cancer. More research in needed on the possible harms of the treatment. (Annals of Internal Medicine, Jan. 7, 2020)
|
Pet ownership linked to lower risk of high blood pressure
 Photo for illustrative purposes only. ©iStock/adamkaz (02/05/2020)
Pet ownership was associated with lower rates of high blood pressure, in a study by Michael E. DeBakey VA Medical Center researchers and associates. Having a pet has previously been linked to lower cardiovascular risk, mostly due to increased physical activity and social support. Researchers looked at data on more than 10,000 participants to examine the link between pets and health. Pet owners in the study had lower hypertension rates than non-owners. Owning a pet did not seem to affect rates of heart failure, coronary artery disease, diabetes, or stroke. Further studies are needed to draw conclusions on the protective effect of pet ownership, say the researchers. (American Journal of Cardiology, Jan. 29, 2020)
|
Study points to shortcomings in VA outcomes for joint replacement surgery
 Photo for illustrative purposes only. ©iStock/sturti (02/05/2020)
VA patients have poorer short-term outcomes than non-VA patients in the general population after hip or knee replacement, found a large retrospective study. Researchers, including one from the VA Central Western Massachusetts Health System, looked at data on more than 10,000 VA and nearly 60,000 non-VA patients who had joint replacement surgery. They found that VA patients were more likely to have hospital readmission, prolonged length of stay, and complications. The finding held even after the researchers adjusted for higher rates of illness in the VA population. More research is needed to understand and address the discrepancy between VA and non-VA outcomes, say the researchers. (Journal of the American Academy of Orthopedic Surgeons, Jan. 30, 2020)
|
Toilet flushing may increase bacteria contamination in hospitals
 Photo: ©iStock/contrastaddict (02/05/2020)
Toilet flushing may contribute to the spread of harmful bacteria in hospitals, according to a study including Iowa City VA researchers. Flushing a toilet can send tiny particles of fecal matter into the air. Researchers took air samples in the rooms of patients with C. difficile infections. They found that concentrations C. difficile and other harmful bacteria were significantly higher after the toilet was flushed. The researchers suggest evaluating prevention measures such as adding toilet lids where they are not currently in place. (Infection Control and Hospital Epidemiology, Jan. 31, 2020)
|
Sexual dysfunction linked to suicidal thoughts in Veterans with PTSD
 Photo for illustrative purposes only. ©iStock/milanvirijevic (01/30/2020)
Sexual dysfunction was linked to suicidal thoughts in Veterans with PTSD, in a San Diego VA study. Sexual dysfunction is common in people with PTSD. Researchers assessed 138 Veterans and their partners before they began couples-based PTSD treatment. The assessment showed that decreased sexual pleasure and decreased frequency of sexual intercourse were linked with more recent suicidal thoughts in male Veterans. For female Veterans, increased sexual frequency was marginally linked with increased suicidal thoughts. The results stress the importance of assessing sexual function as a component of mental health for Veterans with PTSD, say the researchers. (Archives of Sexual Behavior, Jan. 8, 2020)
|
Training program leads to less unnecessary antibiotic prescribing
 Photo: ©iStock/izusek (01/30/2020)
A training program led to less antibiotic prescribing in the VA Pittsburgh Healthcare System. Overprescribing of antibiotics has led to the rise of antimicrobial-resistant bacteria. While many antibiotic stewardship programs have focused on hospitals, most antibiotics are prescribed in outpatient settings. Researchers studied seven VA primary care clinics that underwent antibiotic interventions. The programs involved clinician education, peer comparisons, and computer decision support. The overall number of antibiotic prescriptions decreased significantly after the program. The rate of unnecessary antibiotic prescribing decreased by 36% six months after training. This rate was 25% lower than baseline a year later. The results show that interventions such as this can reduce potentially harmful antibiotic prescribing practices. (Clinical Infectious Diseases, Dec. 9, 2019)
|
Understanding chemotherapy-resistant lung cancer
 Photo: ©iStock/Design Cells (01/30/2020)
Researchers with the Miami VA Healthcare System uncovered a mechanism by which some lung cancer cells resist the chemotherapy drug cisplatin. Researchers used cells in the lab, human blood samples, and mouse models to examine cancer cells at a molecular level. They found that cisplatin-resistant cells had higher activity of an enzyme called IDO1 and higher levels of reactive oxygen species, a chemical byproduct found in many cancers. Reactive oxygen species can cause cell breakdown. But IDO1 initiates the metabolization of kynurenine (an amino acid), which helps cancer cells cope with excessive reactive oxygen species. The researchers were able to use drugs to suppress IDO1 activity. This increased reactive oxygen species levels and in turn inhibited cancer cell growth. The results suggest that IDO1 inhibitors may be a suitable treatment in patients whose lung cancer resists cisplatin, say the researchers. (Molecular Cancer Research, January 2020)
|
More study needed on best C. difficile prevention practices
 Photo by Mitch Mirkin (01/23/2020)
A study of C. difficile in VA hospitals did not find a clear link between prevention practices and infection rates. Researchers surveyed 123 VA facilities. Since implementing prevention practices in 2012, 49% of facilities reported decreased C. difficile rates. Eighteen percent reported an increase, and 33% reported no change. The variation did not appear to be linked to self-reported cleaning practices, length of contact precautions, use of private rooms, or certification of infection preventionists. More study is needed on what practices prevent C. difficile spread, say the researchers. (Infection Control and Hospital Epidemiology, January 2020)
|
Primary care visits linked to better statin adherence
 Photo for illustrative purposes only. ©iStock/monkeybusinessimages (01/23/2020)
More frequent primary care visits were linked to higher statin use and adherence, in a Houston VA study. Researchers looked at more than a million patients with atherosclerotic cardiovascular disease at 130 VA facilities. About 80% of patients were on statins to control cholesterol. Patients who frequently saw their primary care providers had more common statin use, higher-intensity statin use, and better statin adherence. Better adherence may be related to a greater rapport between provider and patients, suggest the researchers. (American Heart Journal, Dec. 7, 2019)
|
Genetics linked to cognitive impairment
 Photo: ©iStock/Nicolas (01/23/2020)
Schizophrenic and bipolar patients with cognitive impairment had genetic variations that have also been linked to cognitive problems in the general population, in a study using Million Veteran Program data. Researchers analyzed the genomes of more than 5,000 patients with schizophrenia or bipolar disorder. No single gene variant showed a significant link to cognitive impairment. However, the researchers did find minor correlations between overall cognitive function and a number of variants shown in the past to be involved in cognitive performance, intelligence, and schizophrenia risk. Greater genetic risk of schizophrenia was linked to poorer cognitive performance. The results add to the understanding of how genetics affect cognition, say the researchers. (American Journal of Medical Genetics, Dec. 24, 2019)
|
Mindfulness program could curb suicide among Veterans
 Photo for illustrative purposes only. ©iStock/electravk (01/16/2020)
Mindfulness-based cognitive therapy shows promise for reducing suicide among Veterans, found a VA New Jersey study. Researchers evaluated 140 Veterans at high risk for suicide. Veterans received either Mindfulness-Based Cognitive Therapy adapted for Suicide (MBCT-S) or VA treatment as usual. MBCT-S combines mindfulness therapy with suicide safety planning. Patients receiving MBCT-S along with usual treatment made fewer suicide attempts within 100 days of treatment. Five of the MBCT-S group attempted suicide, compared with 13 from the control group. MBCT-S patients also showed greater distress tolerance over time. MBCT-S was especially effective in participants who also received VA residential care. No participants receiving both MBCT-S and residential care attempted suicide during the study period. Patients receiving both also had significantly greater improvement on depression, hopelessness, distress tolerance, and suicide-related coping, compared with controls. MBCT-S could be a useful intervention for patients at-risk for suicide, according to the researchers. It can be integrated within existing VA programs, they say. (International Academy of Suicide Research, Oct. 29, 2019)
|
Study probes link between exercise-induced breathing problems and military exposures
 Photo by Senior Airman Julianne Showalter, USAF (01/16/2020)
Findings on the link between military exposures and exercise-induced breathing problems were mixed in a VA New Jersey study. Exposure to fine particulate matter in the air can lead to breathing problems. Service members in Iraq and Afghanistan were regularly exposed to dust and sand, smoke from burn pits, vehicle exhaust, and regional air pollution. Researchers tested the breathing of 24 Veterans without asthma who were not currently seeking treatment for breathing problems. After an exercise challenge, 17% tested positive for bronchial constriction. This rate is similar to the prevalence in the general population. However, a further 42% of the participants had a probable constriction response that did not meet the full diagnostic criteria. Many of the participants reported persistent cough, wheeze, and shortness of breath at the time of testing. The researchers urge continued monitoring of respiratory symptoms in this population. (Military Medicine, Dec. 31, 2019)
|
Study: End-of-life care for Vets with hearing and vision loss is up to par
 Photo for illustrative purposes only. ©iStock/seb_ra (01/16/2020)
Older Veterans with hearing and vision loss receive similar end-of-life care in VA as those without sensory loss, found a Corporal Michael J. Crescenz VA Medical Center study. Researchers looked at data on more than 42,000 Veterans at 145 VA medical centers. They found that end-of-life care quality indicators were similar between patients with and without sensory loss. Patients with hearing loss had slightly lower pain management scores and less satisfaction with communication. Patients with vision loss were less likely to have received a palliative care consult or contact with a chaplain. Patients with vision loss were also less likely to report excellent overall care and satisfaction with emotional support, but most care outcomes were similar to those of patients without vision loss. (Journal of the American Geriatrics Society, Dec. 30, 2019)
|
Complicated grief may make PTSD treatment less effective
 Photo for illustrative purposes only. ©iStock/fizkes (01/16/2020)
Patients with complicated grief have poorer responses to PTSD treatment, found a VA study. Complicated grief refers to feelings of loss after the death of someone close that are debilitating and do not improve with time. It often occurs with PTSD in military personnel. Researchers analyzed outcomes from Veterans being treated with prolonged exposure therapy and medication for combat-related PTSD. They found that those who also had complicated grief had lower response to PTSD treatment than those with PTSD only. Those with complicated grief had greater PTSD severity and trauma-related guilt both before and after treatment. They were also more likely to have suicidal thoughts during the study than patients with PTSD only. The results suggest that screening for complicated grief as well as PTSD may be needed, say the researchers. (Depression and Anxiety, January 2020)
|
Gene mutation linked to ALS
 Photo: ©iStock/koto_feja (12/19/2019)
A large genetic study including a VA researcher identified a gene linked to ALS. Amyotrophic lateral sclerosis (ALS) is a neurodegenerative disease that affects nerve cells. People with ALS progressively lose control of the body’s muscles, which eventually leads to death. Researchers studies the genomes of more than 20,000 patients with ALS and almost 60,000 without to look for genetic causes of the disease. They found that a specific mutation of the gene KIF5A is linked with developing ALS. Mutations to this gene previously have been linked to two other neurodegenerative diseases: hereditary spastic paraplegia and Charcot-Marie-Tooth type 2. However, ALS appears to be linked to a different mutation to gene KIF5A than the other two diseases. The discovery will add to scientists’ understanding of the causes and progression of ALS. (Neuron, March 21, 2018; available in PubMed Central in March 2019)
|
Post-exertion malaise symptom inconsistent in Vets with Gulf War illness
 Photo for illustrative purposes only. ©iStock/ClarkandCompany (12/19/2019)
Although many Veterans with Gulf War illness experience post-exertional malaise, the causes and patterns of the condition remain unknown, found a VA study. Post-exertional malaise refers to increased pain, fatigue, and cognitive problems after physical or mental exertion. It is a common symptom of GWI. Researchers compared symptoms of 39 Gulf War Veterans with and 28 without GWI after exercise. Some participants with GWI perceived exercise as more painful and fatiguing, compared with a control group. However, not all participants with GWI reported post-exertional malaise. The results show that post-exertional malaise is not always a symptom of GWI, say the researchers, and more research is needed on the condition. (International Journal of Psychophysiology, Nov. 28, 2019)
|
Opioids negatively affect pain relief from antidepressant
 Photo: ©iStock/chesiireCat (12/19/2019)
Patients prescribed both opioids and the antidepressant venlafaxine for low back pain had reduced pain relief, in a study including a VA Pittsburgh researcher. Venlafaxine (sold as Effexor) is an antidepressant commonly given to people with chronic pain along with opioids. Because chronic pain and depression are related in a complex way, antidepressant treatment can also reduce pain. The researchers looked at pain relief in older adults with chronic low back pain and depression. They found that patients taking both opioids and venlafaxine had less pain reduction in response to venlafaxine, compared with those not taking opioids. Depression symptoms were not altered by the drug interaction. The study suggests that clinicians may want to reconsider prescribing the two medication together. (Pain Medicine, Oct. 21, 2019)
|
Drug use treatment up for urban and rural Vets in recent years
 Photo for illustrative purposes only. ©iStock/Viktoriia Hnatiuk (12/12/2019)
Substance use disorder treatment has increased in recent years for both urban and rural Veterans, found an Iowa City VA study. Researchers looked at admissions data from non-VA treatment centers between 2011 and 2016. The study included data on more than 90,000 Veterans. Both urban and rural Veterans had similar rates of treatment for SUD. Rural Veterans had slightly higher rates of admission for injectable and opiate drug use. Admissions for opioid, heroin, and injectable drug use increased between 2011 and 2016 for both groups. The study shows that monitoring Veteran care outside VA is crucial to understanding and combating drug use in Veterans, say the researchers. (Journal of Rural Health, Dec. 6, 2019)
|
Sense of purpose appears to ward off cognitive decline
 Photo for illustrative purposes only. ©iStock/Image Source (12/12/2019)
Greater purpose in life is linked with lower cognitive decline in middle age, according to an Atlanta VA and Emory University study. Researchers used a machine learning algorithm to assess how purpose in live affects perceived cognitive function. Purpose in life refers to a tendency to derive meanings and purpose from life events. Average participant age was 63. Researchers tested cognitive function with a questionnaire that assesses perceived functional problems that may not yet rise to clinical impairment. Those with greater purpose in life had less perceived cognitive decline. This result held true even after considering other factors that affect cognitive decline, such as activity level and depression. The results suggest that purpose in life is a robust protective factor of cognitive decline in middle age. (Journal of Affective Disorders, February 2020)
|
Low-vision intervention helps, but challenges remain
 Photo by Jerry Daliege (12/12/2019)
Low-vision services improved visual ability for patients with macular disease, but patients still lost reading ability, in a study of 255 VA patients. Researchers compared outcomes after patients were given either low-vision assistive devices alone or devices along with therapist rehabilitation. Both groups showed significant improvement in visual ability one year later. However, both groups lost visual reading ability during the study period. This loss in reading ability reduced the benefits gained from the low-vision services provided, according to the researchers. They recommend yearly low-vision follow-ups to assess disease progression and modify treatment. (Optometry and Vision Science, October 2019)
|
CPAP compliance lowers diabetic retinopathy risk
 Photo for illustrative purposes only. ©iStock/Darunechka (12/04/2019)
Using prescribed CPAP machines reduces diabetic retinopathy, found a VA Maine Health Care System study. Obstructive sleep apnea has been linked to diabetic retinopathy. Diabetes can cause damage to the blood vessels in the eyes, a condition called retinopathy. It can eventually lead to blindness. Researchers looked at the rates of retinopathy in patients with diabetes who had been prescribed continuous positive airway pressure (CPAP) therapy to treat sleep apnea. Those who used their CPAP machines regularly were significantly less likely to have retinopathy than those who were not compliant with their treatment. The results show that improving CPAP compliance could lower risk of diabetic retinopathy, say the researchers. (Optometry and Vision Science, November 2019)
|
Present-centered therapy eases PTSD, but not as much as cognitive behavioral therapy
 Photo: ©iStock/Pornpak Khunatorn (12/04/2019)
Present-centered therapy can reduce PTSD symptoms, but is less effective than cognitive behavioral therapy, according to a review by VA National Center for PTSD researchers and colleagues. Present-centered therapy (PCT) focuses on the patient’s current life and how to cope with PTSD symptoms. It does not directly confront trauma memories as cognitive behavioral therapy (CBT) does. The review found that PCT reduces PTSD severity, compared with no treatment. However, studies show that CBT is more effective than PCT. Because PCT has a lower treatment dropout rate than CBT, it could be a useful PTSD treatment when patients are resistant to CBT, say the researchers. (Cochrane Database of Systematic Reviews, Nov. 18, 2019)
|
Amino acid may protect against kidney damage
 Photo: ©iStock/cdascher (12/04/2019)
Researchers with the Washington DC VA Medical Center have identified an amino acid that may help reverse kidney damage. They tested the effects of the amino acid L-ornithine on proximal tubular cells, the most common type of cells in the kidney. They found that the amino acid activated a protein called calcium-sensing receptor, which protected the kidney cells from harmful chemicals called reactive oxygen species. When ornithine activates the calcium-sensing receptors, they stop reactive oxygen species from being produced. The results show that ornithine could be useful in reversing kidney diseases involving proximal tubular cell damage, according to the researchers. (Cellular Signalling, Nov. 23, 2019)
|
Excess medication supply potentially a problem for many Vets
 Photo for illustrative purposes only. ©iStock/Burlingham (11/27/2019)
Excess medication supply was high among VA health care users, in a study by the VA Center for Healthcare Organization and Implementation Research. Excess medication was defined as having more doses of a prescription than needed to treat a condition. It can occur for a number of reasons, including being prescribed two different formulations of the same drug. Experts consider this a problem because it can increase the risk of overdose and other harms. In a study of almost 5 million Veterans with prescriptions through VA, 64% had at least one duplicated medication. Excess medication was more likely for Veterans with both VA and non-VA health care and with more medical conditions. Patients who had a copay for medication were less likely to have excess medication. The results show that further efforts are needed to make sure patients receive the right amount of medication, say the researchers. (Medical Care, November 2019)
|
Insulin overtreatment common in VA nursing homes
 Photo: ©iStock/Maya23K (11/27/2019)
Diabetes insulin overtreatment is common in VA nursing homes, found a San Francisco VA Medical Center study. Researchers looked at data on more than 5,000 patients with Type 2 diabetes in VA nursing homes. They found that 14% patients showed signs of overtreatment, based on their HbA1c levels. Only 1.4% showed likely undertreatment. The results suggest that insulin regimens that were appropriate when patients were healthier and living in the community may be too intensive when they get older and transition into nursing homes, say the researchers. Nursing home admission may be a good time to reevaluate diabetes treatment, they conclude. (Journal of Internal Medicine, Nov. 8, 2019)
|
Study suggests a more accurate approach to diabetes diagnosis
 Photo: ©iStock/ftwitty (11/27/2019)
Using HbA1c levels alone can lead to both over- and under-diagnosis of diabetes, according to Atlanta VA researchers and colleagues. HbA1c blood tests determine glucose levels over the previous two to three months. It is the most common test to diagnose diabetes and assess how well patients are controlling their blood sugar. However, for some people the HbA1c test is inaccurate. Some may have higher or lower HbA1c readings than would be expected based on actual glucose levels. The researchers gave participants with diabetes oral glucose tolerance tests, which compare fasting glucose levels with levels after the person is given oral glucose. They found that using HbA1c alone led to under-diagnosis of diabetes for people who had lower HbA1c mismatches, and over-diagnoses for people with mismatches in the other direction. The results suggest oral glucose tests should be used along with HbA1c to ensure a proper diagnosis, say the researchers. ( Diabetic Medicine, Nov. 13, 2019)
|
Swimming may help protect against knee arthritis
 Photo: ©iStock/microgen (11/18/2019)
A study including a Houston VA researcher found that swimming may help protect against knee arthritis. Researchers surveyed more than 2,000 people about their exercise history and knee health. Participants with a history of swimming for exercise had a modestly lower rate of knee osteoarthritis, compared to those who did not swim. Participants who reported swimming at a younger age (between 12 and 34) were less likely to have osteoarthritis than those who swam when older. Swimmers had slightly lower rates of knee pain than non-swimmers, although the results were not statistically significant. The researchers note the possibility that participants with less arthritis led healthier, more active lifestyles in general and the effects seen were not just from swimming. However, a previous study by the same group showed that people who ran for exercise had lower rates of symptomatic arthritis but not radiographic arthritis, suggesting the benefits in the new study were specific to swimming. They also found that people who played football had higher rates of knee arthritis. Swimming is often recommended for patients with osteoarthritis because it is a non-weight bearing exercise that is easy on the joints. But more study is needed to confirm the benefits of swimming on knee health, say the researchers. (Physical Medicine and Rehabilitation, Oct. 19, 2019)
|
Studies lacking on women with TBI
 Photo for illustrative purposes only. ©iStock/SDI Productions (11/18/2019)
Female Veterans and service members are not well-represented in traumatic brain injury research, according to a Washington DC VA Medical Center review. Using several databases, the researchers found 29 studies on TBI in Veterans that included women. They found that few studies focused on gender, and most that did had only a small number of female participants. Most guidelines on TBI care are not differentiated based on gender, most likely due to lack of research. Limited evidence suggests that female Veterans with mild TBI report more neurobehavioral symptoms and use more outpatient health services than male Veterans. Studies also show that female Veterans with TBI are more often diagnosed with depression. More research is needed on how TBI specifically affects female Veterans and service members, say the researchers. (Physical Medicine and Rehabilitation, Aug. 10, 2019)
|
E-cigarettes may make it harder for the body to fight off infection
 Photo: ©iStock/danchooalex (11/18/2019)
Electronic cigarettes weaken the body’s ability to fight infection by affecting immune cells called neutrophils, found a study by VA San Diego and University of California San Diego researchers. Neutrophils are white blood cells that help control infections. Researchers exposed human cells to e-cigarette vapor in a lab. Exposure to the vapor interfered with neutrophils’ ability to respond to the presence of bacteria. The vapor hindered the neutrophils’ ability both to move to the site of bacteria and to produce infection-fighting substances. The neutrophils were affected even when nicotine was not present in the vapor, meaning that e-cigarette ingredients other than nicotine may be harmful. The researchers also found that mice exposed to e-cigarette vapor were less able to fight off bacterial infections than control mice. The results suggest that using e-cigarettes could change the immune response and make people more susceptible to infections, according to the researchers. (American Journal of Physiology, Oct. 30, 2019)
|
Mantram therapy curbs PTSD hyperarousal
 Photo for illustrative purposes only. ©iStock/electravk (11/06/2019)
Mantram repetition therapy may reduce hyperarousal in patients with PTSD, found a VA San Diego study. Hyperarousal, a common PTSD symptom, is a heightened state of anxiety. Common PTSD treatments are less effective at treating hyperarousal than other PTSD symptoms. In the study, researchers had Veterans practice mantram repetition to deal with hyperarousal. Mantram therapy is a type of meditation that employs repeated phrases to train attention and regulate emotions. Those using mantram repetition had greater reductions in hyperarousal, compared with patients using standard psychotherapy only. Those with reduced hyperarousal had greater overall PTSD symptom reduction. The results show that mantram treatment that focuses specifically on hyperarousal could lead to lower PTSD symptoms more generally, according to the researchers. (European Journal of Psychotraumatology, Sept. 30, 2019)
|
Does frequent switching of reminder signs help hand hygiene in hospitals?
 Illustration: ©iStock/Victor_Brave (11/06/2019)
Frequently changing reminder signs did not increase hand hygiene adherence in a study at nine VA medical centers. Proper hand hygiene by health care workers during direct patient contact reduces hospital-acquired infections. But adherence in hospitals to hand-washing guidelines is low. Researchers tested whether increasing the frequency with which hand-hygiene visual reminders were changed would boost adherence. Signs next to antibacterial hand soap dispensers were changed either weekly or monthly to make them more noticeable, or were left the same. Over six months, , hand-washing rates remained nearly the same in all three groups. The researchers concluded that frequently changing signs had no effect on hand hygiene, possibly because of the abundance of other notices in the acute-care setting. (JAMA Network Open, Oct. 2, 2019)
|
New genetic risk factors for PTSD identified
 Illustration: ©iStock/poba (11/06/2019)
A large genome study identified new genetic risk factors for PTSD. The international study included multiple VA researchers. It examined the genomes of over 30,000 participants with PTSD and 170,000 controls without PTSD. The researchers estimate that 5 to 20% of PTSD risk can be attributed to inherited genes, with heritability higher in women than men. The analysis identified three new locations on the genome where gene variations affect a person’s risk for PTSD. Two of these were found only in people of European ancestry and one was only in people of African ancestry. Three other gene locations related to PTSD risk were identified in men only. The study also found that a gene previously linked to Parkinson’s disease is also associated with PTSD. The findings advance the understanding of the genetic basis of PTSD, say the researchers. (Nature Communications, Oct. 8, 2019)
|
Mouse study explores benefits of calorie restriction
 Photo: ©iStock/Eduard Lysenko (11/01/2019)
A VA mouse study has challenged the understanding of how calorie restriction improves health. Limiting calories is known to improve health in mammals, including humans. Prior thought was that this is achieved through improved insulin sensitivity. Researchers at the Madison, Wisconsin, VA tested the effects of calorie restriction on mice with insulin resistance. Calorie-restricted mice had improved fitness and longevity compared to control mice. Calorie rest riction led to similar improvements in both insulin-resistant and non-insulin-resistant mice. The results show that the health benefits of calorie restriction are not solely based on insulin sensitivity, say the researchers. (Cell Reports, Oct. 1, 2019)
|
Opioids overused in dental care
 Photo for illustrative purposes only. ©iStock/tommaso79 (11/01/2019)
U.S. dentists prescribe far more opioids than dentists in other countries, found a review that included a Edward Hines, Jr. VA Hospital researcher. For example, 22.3% of U.S. dental prescriptions in 2016 were for opioids, while only 0.6% were for opioids in the United Kingdom. Dentists are among the most frequent prescribers of opioids. Two large reviews cited by the study also showed that other types of pain medication are at least as effective as opioids for controlling dental pain. Because of the risk of opioid addiction, there is clear patient benefit to avoiding opioids for dental pain, say the researchers. (Journal of the American Dental Association, October 2019)
|
Serious mental illness no barrier to hepatitis C treatment
 Photo: ©iStock/Gligatron (11/01/2019)
Serious mental illness such as schizophrenia doesn’t affect access to hepatitis C treatment in VA, found a VA Capitol Healthcare Network study. Researchers looked at data on more than 4,000 VA patients with hepatitis C in a two-year period. About 30% of patients began treatment with the hepatitis drug sofosbuvir, one of the newer medications responsible for dramatically high cure rates. There was no difference in treatment rates between patients with and without serious mental illness. The results suggest that VA efforts to expand treatment using the new hepatitis C drugs have extended equally to those with serious mental illness, a group that has traditionally experienced barriers to optimal health care. (Psychiatric Services, Oct. 16, 2019)
|
Dietary oils could help with diabetic nerve damage
 Photo: ©iStock/mescioglu (10/28/2019)
A rat study has shown that dietary oils could be an effective treatment for nerve damage caused by diabetes. Researchers from the VA Iowa City Health Care System and University of Iowa simulated diabetes by giving rats a high-fat diet. They then replaced the fat in the rats’ diets (from lard) with unsaturated fats from several dietary oils. Rats given fish oil and flaxseed oil showed improvement in peripheral nerve damage. Enriched fish oil also led to the greatest improvements in vascular dysfunction and cognitive activity. The other dietary oils tested—olive oil, safflower oil, and evening primrose oil—provided no or only small improvements. The results show that dietary fat modification, especially with fish oil, could be a useful treatment for vascular and nerve problems caused by diabetes, say the researchers. (Journal of Diabetes Research, Aug. 7, 2019)
|
Researchers identify genes related to schizophrenia
 Illustration: ©iStock/Lars Neumann (10/28/2019)
A team including VA researchers identified several regions on the genome related to schizophrenia risk. The team sequenced the DNA of more than 1,500 patients with schizophrenia. They found seven regions of the genome that appear to relate to neurological dysfunction in schizophrenia. The analysis also confirmed multiple schizophrenia-related regions identified in previous studies. The results help explain the biological processes of schizophrenia and could lead to new targeted treatments, according to the researchers. (JAMA Psychiatry, Oct. 9, 2019)
|
Smoking linked to higher prostate cancer mortality
 Photo: ©iStock/sanjagrujic (10/28/2019)
Smoking is linked to a higher risk of dying from prostate cancer, found a VA San Diego Health Care System study. Researchers looked at more than 73,000 VA patients diagnosed with prostate cancer. The rate of death from prostate cancer was 5.2% for currents smokers within 10 years of their diagnosis. Past smokers had a 4.8% mortality rate, while those who never smoked had a rate of 4.5%. The study shows that prostate cancer diagnosis may be an important opportunity to discuss quitting smoking. (Prostate Cancer and Prostate Diseases, Oct. 17, 2019)
|
Diabetic Veterans find peer mentors valuable
 Photo for illustrative purposes only. ©iStock/Kali9 (10/17/2019)
Veterans with diabetes found value in a peer mentor program aimed at improving self-care. Veterans at the Corporal Michael J. Crescenz VA Medical Center who had trouble controlling their diabetes were paired with other Veterans who had gotten their blood sugar under control. Mentors called mentees daily to offer encouragement and advice. The researchers interviewed both groups after a six-month period. Participants described several benefits of the program, including accessible support, improved self-confidence, and increased accountability. Some participants faced barriers to the experience, such as scheduling problems and interpersonal conflicts. The more successful mentees said they had a strong connection to their mentor. The study shows that a low-cost peer mentor program can offer support to patients with diabetes that may improve their self-care. (Diabetes Educator, Oct. 9, 2019)
|
Alcohol withdrawal in VA hospital patients
 Photo: ©iStock/ZzzVuk (10/17/2019)
Alcohol withdrawal syndrome affected nearly 6% of Veterans hospitalized in VA in 2013, found a VA Puget Sound study. Heavy drinkers may go through withdrawal when they suddenly stop drinking. Withdrawal symptoms include trembling, headache, and even hallucinations and seizures. Researchers looked at data on almost half a million VA hospitalizations. Of those, 5.8% of patients had documented AWS. The prevalence varied widely based on location, facility, admitting specialty, and diagnosis. Psychiatric admissions had a higher rate of AWS than medical or surgical. AWS was especially common during hospitalizations for other alcohol-related disorders, substance use disorders, attempted suicide, and liver injury. (Journal of Addiction Medicine, Oct. 11, 2019)
|
Tinnitus rates going up in active duty service members
 Photo by Spc. Anthony Zendejas/USA (10/17/2019)
Tinnitus rates in active duty service members have increased significantly in recent years, according to a study by South Texas VA Health Care System and University of Texas at San Antonio researchers. They studied the health records of more than 85,000 active duty service members. Between 2001 and 2015, the rate of tinnitus more than tripled. Tinnitus refers to a ringing or buzzing in the ears. It is often caused by blast exposure. This was the first study to assess tinnitus rates in active duty rather than in Veterans. Further studies are needed on how hearing damage impacts active duty service members, say the researchers. (American Journal of Audiology, Oct. 16, 2019)
|
Early deployment could increase suicide risk
 U.S. Army photo by Maj. Thomas Cieslak (10/02/2019)
Early first deployment may increase the risk of suicide attempt, according to a study of U.S. enlisted soldiers. VA San Diego researchers and colleagues looked at data on a large number of soldiers, including 1,700 who attempted suicide. Soldiers who deployed within 12 months of beginning their Army service were 70% more likely to attempt suicide, compared with soldiers who deployed later. The early deployers’ risk was elevated both during and after deployment. More study is needed to understand how training and preparedness affect suicidal behavior, say the researchers. (Suicide & Life-Threatening Behavior, Sept. 23, 2019)
|
Supported employment boosts functional outcomes in PTSD
 Photo: ©iStock/shironosov (10/02/2019)
Supported employment improves overall PTSD-related functioning, found a VA study. Individual Placement and Support is a VA program to help Veterans with PTSD find jobs. It uses individual-centered job development and employment specialists. Past studies have showed that IPS is more effective than transitional work programs at helping Veterans find sustained employment. The new study of 512 Veterans shows that IPS also improves PTSD-related functions in other areas. In addition to greater work functioning, Veterans given IPS had greater improvement in school, relationship, and lifestyle functioning, compared with those given transitional work. The results show that IPS has benefits beyond helping Veterans with PTSD find work. (Psychiatric Rehabilitation Journal, September 2019)
|
Brain structures account for transcranial magnetic stimulation effectiveness
(10/02/2019)
A team including Providence VA Medical Center researchers identified brain structures that influence the effectiveness of transcranial magnetic stimulation for PTSD and depression. In TMS, magnets are placed on the outside of the head to affect electrical signals in the brain. The therapy has emerged in recent studies as a promising treatment for PTSD. Researchers used MRI to study the pre-TMS brain structure of 20 patients. Those with greater connectivity in the anterior thalamic radiation (fiber pathways in the white matter) had greater symptom relief after TMS. The results suggest that this brain area could be a good target for TMS treatment, according to the researchers. (Depression and Anxiety, Sept. 2, 2019)
|
Metformin, versus sulfonylureas, linked to fewer heart issues for diabetes patients with weakened kidneys
 Photo: ©iStock/ljubaphoto (09/26/2019)
The diabetes drug metformin is more effective than sulfonylureas, a separate class of commonly used diabetes drugs, at preventing cardiovascular events in patients with reduced kidney function, according to a Tennessee Valley VA Health Care System study. Past studies showed that metformin is more effective at treating diabetes than sulfonylureas. However, worries over possible kidney damage led the FDA to warn against metformin for people with reduced kidney function. In 2016, the FDA revised its recommendation to say metformin was safe for people with kidney disease. To test metformin’s effectiveness in this population, the researchers studied data on nearly 175,000 VA patients. They found that diabetic patients on metformin had significantly fewer cardiovascular events (such as heart attack or stroke) than those on sulfonylureas. (JAMA, Sept. 19, 2019)
|
Mouse study: Potential stroke treatment only effective in males
 Photo: ©iStock/D-Keine (09/26/2019)
In a mouse study, a potential stroke therapy was found to be effective in males but not females. A team of VA Portland Health Care System researchers and colleagues gave stroke-affected mice a drug called anti-PDL2. An inflammatory immune response can lead to brain tissue death during stroke. Anti-PDL2 potentially block this immune response. The team found that giving anti-PDL2 significantly reduced the amount of brain cell death, but only in male mice. It had no protective effects in female mice. The difference may be due to changes in cell production in the spleen that occurred in males but not females. The results suggest that anti-PDL2’s potential as a stroke treatment may be limited to men, say the researchers. (Metabolic Brain Disease, Aug. 13, 2019)
|
No link found between herbicide exposure and restrictive pulmonary disease
 Photo for illustrative purposes only. Courtesy of Cincinnati VAMC (09/26/2019)
A study by the VA Office of Patient Care Services did not find a link between herbicide exposure in Vietnam and restrictive pulmonary disease. Researchers tested Veterans using a spirometer, which measures lung volume. While participants who sprayed herbicides during their service showed more lung restriction than those who did not, the difference was not statistically significant. Race and waist circumference were much more predictive of restrictive pulmonary disease. Previous studies have shown race and weight to be risk factors for the disease. Black participants were three times more likely than white participants to have restricted breathing. Those with a larger waist circumference were 2.5 times more likely to have restricted breathing than those with a smaller waist. More research is needed on how chemical exposure may affect breathing in Veterans, according to the researchers. (International Journal of Environmental Research and Public Health, Aug. 28, 2019)
|
Gene linked to thinner cortex in PTSD patients
 Photo: ©iStock/Denes Farkas (09/19/2019)
Researchers at the VA Boston Healthcare System found evidence that gene variants are linked to reduced cortical thickness in people with PTSD. Past research has shown that PTSD is connected to reduced thickness in the cortex, the outer layer of the brain. By testing the genomes of 240 Veterans with PTSD, the researchers found that participants with specific variants of the gene PPM1F had reduced cortical thickness. The results suggest that people with these gene variants may be susceptible to greater PTSD severity from changes in brain structure, say the researchers. (Journal of Affective Disorders, Aug. 19, 2019)
|
Many VA providers unaware of corticosteroid risks
 Photo for illustrative purposes only. ©iStock/RgStudio (09/19/2019)
Many providers are unaware of guidelines on corticosteroid use for COPD, according to a survey of VA primary care providers. Inhaled corticosteroids are recommended for chronic obstructive pulmonary disease (COPD) only in severe cases. Their use can lead to pneumonia, fracture risk, cataracts, and poor diabetes control. However, more than 50% of COPD patients in VA are prescribed the drugs. According to the survey, many providers are not aware of the current evidence and recommendations regarding corticosteroids. For example, 46% were unaware of the risk of pneumonia. Participants said it was hard to keep up with current guidelines because of the broad scope of primary practice. Many were also reluctant to change prescriptions made by other providers. More efforts are needed to limit the use of this potentially harmful drug class in VA, say the researchers. (Journal of General Internal Medicine, Aug 8, 2019)
|
Diabetes risk over time for women Vets of Vietnam era
 Photo by CPT George Clemmons/USAF (09/19/2019)
A VA study tracked the diabetes risk of women who served during the Vietnam War. Researchers interviewed 4,500 women who served between 1965 and 1973. Those who served in the warzone in Vietnam had a three-times lower diabetes risk at the start of their service, compared with women serving stateside. However, diabetes risk increased 38% faster in that Vietnam group than in the U.S. group in the decades after service. The researchers speculate that the lower initial risk could be due to the physical and mental fitness standards for service members in warzones. These standards are often not maintained when Veterans separate from service. Diabetes risk did not differ between women serving near but not in Vietnam and those serving in the U.S. The results show that factors related to warzone service that may lower diabetes risk can quickly wane as Veterans age. (Women’s Health Issues, Sept. 10, 2019)
|
VA relatively free of disparities in colorectal cancer screening
 (Photo illustration by Michael Escalante) (09/11/2019)
Many demographic disparities in colorectal cancer screening seen in the general population do not exist in VA. That is the main finding from a study by VA Greater Los Angeles Healthcare System researchers. In the database study, the overall colorectal screening rate for VA patients ages 50 to 75 was 82%. Rates were lowest among American Indians/Alaska Natives, those with a history of serious mental illness or substance abuse, and those with the lowest socioeconomic status. However, screening rates even for these groups topped 75%. Older age, Hispanic ethnicity, black race, Asian race, and co-occurring illnesses were all predictors of higher screening rates. Although screening disparities are relatively rare in VA, groups with lower rates might benefit from targeted efforts to increase uptake, say the researchers. (Medical Care, Aug. 14, 2019)
|
Menopause linked to more opioid prescribing
 Photo for illustrative purposes only. ©iStock/BakiBG (09/11/2019)
VA researchers in San Francisco looked at prescribing data from over 100,000 mid-life women Veterans with chronic pain. They found that menopause symptoms were linked with higher opioid prescribing. Women with symptoms had higher odds of being prescribed long-term opioids, high-dose opioids, and opioids co-prescribed with central nervous system depressants such as sedatives or muscle relaxants, compared with symptom-free women. Another study by the team found that women with menopause symptoms were twice as likely to have chronic pain than those without symptoms. The researchers say more awareness of the links between menopause and pain could help curb risky prescribing. (Journal of General Internal Medicine, Aug. 14, 2019)
|
Cardiology visits linked with more statin use
 Photo: ©iStock/South_agency (09/11/2019)
Houston VA researchers and their colleagues found that cardiology visits lead to more statin use and adherence in patients with cardiovascular disease. Statin drugs lower cholesterol and help ward off heart attacks and strokes. The team studied data on more than a million VA patients with cardiovascular disease. Patients who had visited a cardiologist had greater odds of being on a statin and staying with the treatment, compared with those who had seen only a primary care provider. More cardiology visits were linked with greater statin use and adherence. Referrals to cardiologists may be among the strategies needed to boost appropriate statin use, say the researchers. (American Journal of Cardiology, July 25, 2019)
|
Traumatic loss tied to poorer response to PTSD treatment
 Photo: ©iStock/fizkes (09/11/2019)
In a study that included several VA researchers, service members with PTSD stemming from traumatic losses—such as the death of buddies—were less responsive to treatment than those with PTSD related to other causes. Past studies have shown that combat-related PTSD is less responsive to treatment than PTSD among civilians. The traumatic death of a close friend or colleague is a common deployment experience. The study showed that service members with traumatic loss-related PTSD recovered less from depression than those who experienced other traumatic events. Less recovery from depression predicted less recovery from PTSD. The results suggest that PTSD therapists should take into account loss and grief in military populations. Therapy could be tailored to focus on feelings of grief and guilt, say the researchers. (Journal of Traumatic Stress, Aug. 28, 2019)
|
Veterans in rural areas do not face longer kidney transplant wait times
 Photo: ©iStock/uchar (09/05/2019)
Rural and urban Veterans have similar wait times for kidney transplant, according to an Iowa City VA Medical Center study. Prior research has shown that VA patients in need of new kidneys have lower rates of transplant than non-Veterans. Rural residents also have lower transplant rates than urban residents in the general population. A higher proportion of Veterans live in rural areas, compared with non-Veterans. To see whether these factors affected transplant rates, researchers looked at data on more than 3,000 Veterans participating in VHA's transplant programs. Veterans living in urban areas spent a longer time on dialysis than rural Veterans before registering for the transplant waitlist. But once on the waitlist, rural and urban Veterans did not have a significant difference in how long they waited for a kidney transplant. More research is needed to determine why transplant rates differ between Veterans and non-Veterans, the researchers write. (Transplantation, September 2019)
|
Controlled blast exposure top predictor of service-connected disability
 Photo by Lance Cpl. Immanuel Johnson/USMC (09/05/2019)
Exposure to blasts from controlled detonations was the most common predictor of service-connected disability, in a study of post-9/11 Veterans. The number of controlled blasts experienced was the top predictor of a service-connected disability rating of 50% or greater. Breachers—personnel who use explosives to create entries to buildings—often have repeated exposure to low-level blasts, both in combat and training. The second highest predictor of high service-connected disability was exposure to uncontrolled blasts, such as from improvised explosive devices in combat. The results suggest that military calculations on the minimum safe distance from blasts may be inaccurate, say the researchers. (Military Health System Research Symposium, Aug. 22, 2019)
|
Low-value prostate cancer screening prevalent in VA
 Photo: ©iStock/jarun011 (09/05/2019)
Low-value prostate cancer screening remains prevalent in the VA health system, found a VA Pittsburgh Healthcare System study. Prior research has shown that screening for prostate-specific antigen—a biomarker of prostate cancer in the blood—does not improve survival of men 70 and older. The screening can lead to anxiety about diagnosis and overly aggressive treatment. Out of more than 200,000 male Veterans 75 or older, 18% underwent prostate-specific antigen screening in the study year. The rates of screening for this age group of men varied across VA medical centers, ranging from 3% to 38%. The results show that more efforts are needed to reduce low-value tests in VA, say the researchers. (Journal of the American Geriatrics Society, July 5, 2019)
|
Boosting addiction treatment for opioid misuse
 Photo: ©iStock/KatarzynaBialasiewicz (08/28/2019)
Recommending addiction treatment may increase patients’ interest in and use of treatment for opioid misuse, according to VA New Jersey Health Care System researchers. They surveyed 567 patients taking opioids for chronic pain. A majority (63%) screened positive for opioid misuse. Health care providers had recommended addiction treatment to nearly a third of those misusing opioids. Almost the same number of patients took advantage of the treatment. In the survey, patients who had been offered treatment were more likely to say they were interested in the option, and, not surprisingly, were far more likely to report actually having undergone treatment, compared with those who were misusing but had not received a recommendation. More research is needed on barriers to providers’ recommending addiction treatment for patients taking opioids for chronic pain, write the researchers. (American Psychological Association 2019 convention, Aug. 8, 2019)
|
Telephone goal-setting may ease depression in diabetic patients
 Photo: ©iStock/MartinPrescott (08/28/2019)
Telephone-delivered collaborative goal-setting can help reduce depression in patients with diabetes, found a Michael E. DeBakey VA Medical Center study. One in three patients with diabetes also have depression symptoms. Patients with both uncontrolled diabetes and clinical depression were enrolled in the Healthy Outcomes Through Patient Empowerment (HOPE) program. HOPE includes nine telephone sessions with health care professionals, focusing on collaborative goal-setting to improve health and behavior. Twelve months after participating in HOPE, patients had lower depression symptom scores, compared with patients receiving usual care. HOPE did not lead to improved diabetes control, as measured by HbA1c levels. The results show that HOPE has potential to improve depression in patients with diabetes, say the researchers. (JAMA Network Open, Aug. 2, 2019)
|
Financial incentives fail to boost colorectal screening rates
 Photo: ©iStock/JoKMedia (08/28/2019)
Small financial incentives did not increase colorectal cancer screening participation, in a study including a VA San Diego Healthcare System researcher. Patients were mailed a fecal immunochemical test annually for three years. Some patients were also offered either a $5 or $10 incentive to complete the test. Response rates were similar for patients given outreach only and for both incentive levels. While previous research has shown that financial incentives may improve short-term health behaviors, the results suggest that they may not be effective for longer-term periodic testing, according to the researchers. (Cancer Epidemiology, Biomarkers & Prevention, Aug. 6, 2019)
|
New insight on the genetic basis of psychological resilience
 U.S. Army photo by Spc. Jeffery (08/22/2019)
A genetic study of U.S. soldiers has shown that psychological resilience may have a genetic basis. The study team, which included researchers from the VA San Diego and Connecticut health care systems, used genome mapping and survey data from more than 11,000 new recruits and deployed soldiers of European ancestry. They measured resilience both subjectively, as self-assessed ability to handle stress, and objectively, using mental disorder diagnoses. Two genes—DCLK2 and KLHL36—were linked with self-assessed resilience. Preliminary results on a smaller group of soldiers who had experienced high levels of combat stress suggest that another gene, SLC15A5, may influence objectively measured resilience. The results offer new insights into the possible biological bases for resilience to stressors, say the researchers. (American Journal of Medical Genetics, July 2019)
|
After smokers quit, heart risk declines, but slowly
 Photo: ©iStock/Suriyawut Suriya (08/22/2019)
Former heavy smokers had lower risk of cardiovascular disease five years after quitting but were still at greater risk than people who had never smoked, in a study including VA Tennessee Valley Healthcare System researchers. The study followed nearly 9,000 people for several decades. Heavy smokers who had quit about half the risk of cardiovascular disease five years after they stopped smoking, compared with current smokers. However, they were still at significantly higher risk than people who had never smoked. Former smokers had about the same cardiovascular risk as nonsmokers 10 to 15 years after quitting. The results show that while quitting smoking lowers risk of cardiovascular disease, it may take a decade or more for the risk caused by smoking to totally decline. (JAMA, Aug. 20, 2019)
|
Pre-treatment level of protein could predict cancer drug’s effects
 Photo: ©iStock/Alexey_ds (08/22/2019)
A phase 2 clinical trial that included VA researchers in Miami suggests that measuring a certain protein before treatment could predict whether a second-line cancer drug will be effective. The study added to the evidence that pembrolizumab (sold as Keytruda) may help slow or stop liver cancer progression for some patients. The drug, used for multiple types of cancer, has been given accelerated approval as a second-line treatment for liver cancer, but has not received full approval. The researchers tested the blood of nearly 30 liver cancer patients given intravenous pembrolizumab for three weeks. Tumor progression slowed or stopped in about a third of patients. Blood tests showed that a high level of TBF-beta—a protein involved in cell growth—before treatment was associated with poorer outcomes. The majority of adverse side effects were manageable—such as rash, fatigue, and diarrhea. While more testing is needed on the drug’s effects, it would be reasonable to combine pembrolizumab with first-line treatments to improve response, say the researchers, adding that TGF-beta “could be a predictive biomarker.” (Cancer, June 28, 2019)
|
Mouse study probes nicotine addiction from e-cigarettes
 Photo: ©iStock/sestovic (08/15/2019)
Daily use of electronic cigarettes may lead to nicotine addiction due to similar biological changes as are seen with regular cigarettes, suggests a mouse study by VA San Diego Healthcare System researchers and colleagues. E-cigarettes produce an aerosol that contains nicotine, as an alternative to smoking. To test whether using e-cigarettes (also known as “vaping”) affects the same addiction pathway as conventional cigarettes, researchers exposed mice to nicotine vapor daily, comparable to a chronic e-cigarette use. They found that six months of exposure decreased dopamine concentrations in the striatum area of the brain. Concentrations of the neurotransmitter GABA decreased in the frontal cortex. Concentrations of the neurotransmitters glutamate and glutamine were increased. Changes in glutamate and dopamine levels are known to be involved in drug dependence, including in nicotine addiction. This imbalance of neurotransmitters could drive nicotine addiction from e-cigarettes, say the researchers. (Frontiers in Pharmacology, Aug. 12, 2019)
|
Do more blood pressure drugs pay off for nursing home residents?
 Photo: ©iStock/Creative-Family (08/15/2019)
Nursing home residents with high blood pressure do not get significant added benefit from multiple blood pressure medications, found a study by VA researchers from several systems. Researchers studied data from more than U.S. 250,000 nursing home residents with high blood pressure. They found small increases in hospitalization rates in residents whose blood pressure medication intensity had been increased. On the other hand, these patients had a slightly smaller decline in their activity level, compared with peers on fewer blood pressure medications. Intensity of blood pressure treatment did not affect mortality. On balance, the researchers concluded that the benefits from more intense blood pressure treatment were not significant, especially in light of the increased risk for side effects such as falls and incontinence. (Journal of the American Geriatrics Society, July 22, 2019)
|
The formula for effective rapid response in hospitals
 Photo for illustrative purposes only. ©iStock/stockstudioX (08/15/2019)
A team including VA Ann Arbor Healthcare System and Iowa City VA Medical Center researchers evaluated the factors linked to high performance in rapid response teams for in-hospital cardiac arrest. They interviewed 158 clinicians and staff at nine different hospitals. At top-performing hospitals, rapid response teams were typically staffed by dedicated team members without competing responsibilities. They collaborated with bedside nurses before, during, and after rapid response events. Bedside nurses at top-performing hospitals were empowered to activate rapid responses based on their own judgment. At lower-performing hospitals, rapid response teams often had competing responsibilities and were less engaged with bedside nurses. Nurses at lower-performing hospitals were concerned about potential consequences from activating a rapid response. The findings can provide insights on the best way to handle in-hospital cardiac arrests, say the researchers. (JAMA Internal Medicine, July 29, 2019)
|
Women and men differ in understanding of harassment
 Photo: ©iStock/asiandelight (08/07/2019)
Women and men have different perceptions of stranger harassment on VA facility grounds, found a VA Greater Los Angeles Healthcare System study. Stranger harassment refers to unwanted comments and attention—such as cat-calls and sexual comments. One in four women VA health care users has experienced harassment at VA facilities, according to a recent VA study, usually from male Veterans. In follow-up, researchers held group discussions at four VA medical centers to get patient perspectives on the problem. Women, on the whole, had clear understandings and experiences of what behaviors constituted harassment. Many men, however, expressed confusion about the difference between harassment and acceptable behavior, such as general friendliness and “harmless flirting.” Men said women should set boundaries with men, while women indicated it was not their responsibility to “train” men about acceptable behavior. Both men and women said that VA staff are primarily responsible for preventing harassment. Participating Veterans recommended educating male Veterans on the issue, as well as training staff to address the problem. (Women’s Health Issues, June 25, 2019)
|
Improving ‘affirming care’ for LGBT Veterans
 Photo for illustrative purposes only. ©iStock/asiseeit (08/07/2019)
Researchers with the VA Boston Healthcare System and Michael E. DeBakey VA Medical Center reported on the facilitators and barriers in a program to improve LGBT services for VA patients. The program, launched in 2016, requires every VHA facility to appoint an LGBT Veteran Care Coordinator to support affirming care. Affirming care includes providing LGBT patients with a welcoming environment and addressing their specific health care needs. Researchers surveyed 79 care coordinators to see how well the program has been implemented. The highest positive facilitator to the program was leadership engagement, reported by 53% of coordinators. The largest barrier was insufficient availability of resources, reported by 66% of coordinators. The survey results will help VHA improve the program in the future, say the researchers. (Psychological Services, July 25, 2019)
|
Pre-deployment TBI increases odds of post-deployment alcohol misuse
 iStock/South_agency (08/07/2019)
Traumatic brain injury prior to deployment could lead to problem drinking in soldiers after deployment, according to a study based on the Army STARRS survey. Soldiers who had a TBI that included loss of consciousness prior to deploying to Afghanistan had increased odds of binge drinking (five or more drinks at once) and heavy drinking (weekly binge drinking) three months after deployment. The connection between TBI and drinking appears more pronounced when the TBI occurred prior to age 13. Those who experienced both a prior TBI and a deployment-related TBI had even higher odds of heavy drinking nine months after deployment. The results suggest that routine screening for pre-deployment TBIs may help target efforts to prevent alcohol misuse in military members, say the researchers. (Journal of Head Trauma Rehabilitation, July 29, 2019)
|
Post-TBI symptoms linked to suicide attempts in soldiers
 Photo for illustrative purposes only. By Ensign Haraz Ghanbari/USN (08/01/2019)
Having traumatic brain injury symptoms before deployment was linked to post-deployment suicide attempts in soldiers deployed to Afghanistan, found a study including a VA San Diego Healthcare System researcher. Using the Army STARRS survey, the researchers studied data on 7,677 soldiers deployed to Afghanistan in 2012. Of those, 103 made a suicide attempt. Soldiers who had post-concussive/post-TBI symptoms before deployment had a higher risk of a suicide attempt than those without TBI symptoms. The results show that detecting post-TBI symptoms could help target suicide prevention programs, say the researchers. (Journal of Head Trauma Rehabilitation, July 11, 2019)
|
Diabetes and Alzheimer’s risk factors together linked to greater cognitive decline
 Photo for illustrative purposes only. ©iStock/Juanmonino (08/01/2019)
Patients with both diabetes and Alzheimer’s disease risk factors showed greater cognitive decline than those with one or the other, in a VA San Diego Healthcare System study. Researchers followed the cognitive functioning of patients for five years. Patients with both diabetes and at least one Alzheimer’s risk factor showed the most cognitive decline, greater than those with only diabetes, only Alzheimer’s risk factors, or neither. Alzheimer’s risk factors included subtle cognitive decline, genetic risk, and three biomarkers found in the spinal fluid. The results suggest that diabetes interacts with Alzheimer’s risk factors to increase cognitive decline, according to the researchers. (Alzheimer’s Disease and Associated Disorders, July 10, 2019)
|
Substance use disorder treatment low for both HIV-infected and uninfected Veterans
 Photo for illustrative purposes only. ©iStock/joloei (08/01/2019)
Substance use disorder treatment was low for Veterans both with and without HIV, in a study of more than 160,000 Veterans. Researchers studied how HIV status affected patients’ use of treatment for substance use disorders, considering SUDs are common in patients with HIV. Patients with HIV were slightly more likely than those without to have an SUD. Fewer than 17% of patients with an SUD engaged in treatment in both the HIV and non-HIV groups. Patients with HIV were more likely to stay in SUD treatment for six months, but the difference was small. While the percentage of VA patients with SUDs who receive treatment is higher than SUD treatment rates in the general population, the researchers still say efforts are needed to get more Veterans to engage in SUD treatment, regardless of HIV status.-
- (Journal of Substance Abuse Treatment, August 2019)
|
Aspirin may help cancer patients live longer
(07/25/2019)
Aspirin use was linked with better survival in patients with head and neck cancer, in a study of patients at the Washington DC VA Medical Center. Studies have shown that long-term aspirin use can reduce the risk of developing several types of cancer, but its effects after cancer diagnosis are unknown. Researchers looked at the medical charts of 584 Veterans treated for cancers of the head and neck over a 20-year period. About 26% were prescribed long-term aspirin use. Aspirin users were significantly more likely to survive for at least three years after diagnosis. Overall survival was 79% for aspirin users and 56% for those not taking aspirin. While the study was not designed to show direct cause and effect, the results do suggest that aspirin may be a useful addition to treatment for head and neck cancer, say the researchers. (Head and Neck, May 2019)
|
Blast exposure linked to decreased sound tolerance
 DoD photo by Lance Cpl. Immanuel Johnson (07/25/2019)
Blast exposure increases the likelihood of decreased sound tolerance in Veterans and service members, according to a VA Portland Health Care System study. People with decreased sound tolerance often experience negative physical or psychological reactions to everyday sounds, such as being uncomfortable or overwhelmed from the background noise of a public place. Researchers looked at data on 426 Veterans and service members who participated in a study on hearing. They found that, of those with blast exposure, 33% of service members and 48% of Veterans had decreased sound tolerance. For who had not been exposed to blasts, 28% of service members and 34% of Veterans had decreased sound tolerance. The researchers say more study is needed to understand the connection between blast exposure and sound tolerance, and to examine whether related auditory injuries are going undetected. (Scientific Reports, July 15, 2019)
|
Combined VA, Medicare Part D prescription use increases unsafe medication risk
 Photo: ©iStock/Darwin Brandis (07/25/2019)
Older Veterans who use both VA and Medicare Part D are at increased risk of receiving unsafe medication, according to a study by VA researchers from several VA locations. Almost all Veterans 65 and older with prescription benefits from VA are also eligible for Medicare Part D. To see whether dual use of prescription sources increases seniors’ risk of unsafe medication use, the researchers looked at data for nearly 280,000 Veterans. They found that dual-use patients had a nearly twofold increase in the odds of receiving potentially unsafe medication. The results show that policies to expand Veterans’ access to non-VA providers must ensure patient information is shared to avoid dangerous prescribing, say the researchers. (JAMA Internal Medicine, July 22, 2019)
|
How aspirin helps against cancer
 Photo: ©iStock/sd619 (07/17/2019)
A Michael E. DeBakey VA Medical Center researcher and a colleague have identified the possible mechanism behind aspirin’s anticancer activity. Low-dose aspirin has been found to both help stop many forms of cancer from forming and also block cancer’s ability to spread when taken after diagnosis. The researchers found evidence that aspirin’s ability to inhibit platelet cyclooxygenase-1—an enzyme related to inflammation—is the key mechanism behind this. Platelet levels are often elevated in the later stages of cancer. They are known to promote cancer growth. Past research by the VA and University of Texas team has shown that low-dose aspirin can block the pro-cancer action of platelets, but until now the way this interaction worked was unknown. (Cancer Research, March 7, 2019)
|
Traumatic brain injury linked to higher psychiatric risk and symptoms
 Illustration: ©iStock/Lamenko (07/17/2019)
Service members and Veterans with a history of traumatic brain injury have higher rates and severity of psychiatric conditions, found a Minneapolis VA Health Care System review. Researchers analyzed studies on TBI and psychiatric disorders conducted over a 17-year period, and found 33 relevant studies. The review shows that service members and Veterans with TBIs had higher rates of PTSD, depressive disorder, substance use disorder, and anxiety disorder, compared to those without TBI. One study showed higher rates of suicide attempts in people with TBI. Geographically diverse studies linked TBI to greater symptom severity of PTSD. Results of TBI’s effect on depression and substance use disorder symptom severity were mixed. According to the researchers, the results support a need for increased emphasis on evaluation of psychiatric conditions in service members and Veterans with a history of TBI. (Journal of Head Trauma Rehabilitation, April 25, 2019)
|
Diet quality affects gut microbiome
 Photo: ©iStock/mphillips007 (07/17/2019)
Quality of diet affects the microbiome in the digestive tract, found a Michael E. DeBakey VA Medical Center study. Researchers studied the types of bacteria present in the colon of patients undergoing a colonoscopy. They found that patients who reported eating a good-quality diet—one high in fruits, vegetable, and whole grains and low in sugar, alcohol, and fats—had higher levels of beneficial bacteria, such as those with anti-inflammatory properties. Those with a poor-quality diet, by comparison, had more potentially harmful bacteria, such as bacteria linked to colorectal cancer. The study suggests that the microbiome of the colon can be modified through diet, which could help reduce the risk of chronic diseases, say the researchers. (American Journal of Clinical Nutrition, July 10, 2019)
|
Telehealth helps with HIV management
 Photo: ©iStock/AndreyPopov (07/10/2019)
Telehealth availability improves viral suppression in HIV patients, found a VA Office of Rural Health study. Patients who previously traveled long distances to HIV specialty clinics were offered telehealth visits in nearby primary care clinics. The researchers compared outcomes of patients living in areas where telehealth was available to those of patients in areas without telehealth. In the areas where telehealth was available, 13% of patients used the option. Small average improvements in viral suppression were seen in patients offered telehealth visits compared with patients not offered telehealth, regardless of whether patients took advantage of telehealth or not. Patients who actually used telehealth had large improvements in viral suppression. The results show that HIV clinics should offer telehealth visits for patients facing travel burdens, say the researchers. (Open Forum Infectious Diseases, May 10, 2019)
|
Care cost lower for diabetes patients primarily seeing NPs or PAs rather than physicians
 Photo: ©iStock/Ridofranz (07/10/2019)
Use of nurse practitioners and physician assistants could lead to lower health care costs for diabetes care, according to a Durham VA Health Care System study. Researchers looked at a year of VA data on medically complex patients with diabetes. They found that patients whose primary care provider was a nurse practitioner or physician assistant had 6–7% lower average total care costs than patients with a physician as the primary care provider. The difference was mainly due to more use of emergency and inpatients services by the physician group. The study suggests that nurse practitioners and physician assistants can effectively manage primary care for complex patients with diabetes without increasing care costs. (Health Affairs, June 2019)
|
Newer hepatitis C drugs pose advantage for diabetes risk
 Photo: ©iStock/okskaz (07/10/2019)
Hepatitis C patients treated with directly acting antiviral agents had lower risk of diabetes than patients treated with interferon, in a VA Pittsburgh Healthcare System study. Hepatitis C infection is linked to higher risk of diabetes. Results from previous research were mixed on whether treatment with interferon—an older treatment for hepatitis C—affects diabetes risk. To test how newer directly acting antiviral agent treatment affects diabetes risk, researchers studied data on more than 240,000 people with chronic hepatitis C. For both untreated patients and patients treated with interferon, about 2% developed diabetes. Only 0.1% of patients treated with directly acting antiviral agents developed diabetes after treatment. Patients with more advanced liver fibrosis had even larger diabetes risk reduction. The results show that the new antiviral agents may be better than older treatments at controlling hepatitis C complications, say the researchers. (Clinical Infectious Diseases, April 12, 2019)
|
Continuity of care linked to better outcomes in inflammatory bowel disease
 Photo for illustrative purposes only. ©iStock/Capifrutta (07/09/2019)
Greater continuity of care leads to better outcomes for patients with inflammatory bowel disease, according to a VA Ann Arbor Healthcare System study. Researchers looked at more than 46,000 patients with inflammatory bowel disease—that is, either Crohn’s disease or ulcerative colitis—who received care through VA. Average continuity of care (meaning patients saw the same provider for outpatient visits) was only 23%. Patients with lower care continuity had more flare ups, need for medication, hospitalizations, and surgery than those with more continuity. More research is needed on how to improve continuity of care and how team-based care may affect patient outcomes, say the researchers. (Digestive Disease Week, May 17, 2019)
|
Complementary and integrative health use linked to lower costs
 Photo: ©iStock/Wavebreakmedia (07/09/2019)
Using complementary and integrative health (CIH) approaches for chronic musculoskeletal pain led to lower health care costs and pain in younger Veterans, found a study by VA researchers from several systems. CIH refers to practices not currently part of mainstream, conventional medical practice, such as acupuncture, chiropractic care, and massage. Researchers looked at data on more than 30,000 Veterans who used CIH and nearly 200,000 who did not. They found that CIH use was linked with lower health care costs and less pain from chronic musculoskeletal conditions, compared with one year before patients began CIH. However, the CIH group had slightly higher opioid use than those who did not use CIH. The researchers theorize that the slightly higher opioid use could reflect the fact that many patients turn to CIH treatments as a last resort after trying other pain treatments such as opioids. The results show that use of CIH is cost-effective and can even be cost-saving, they say. (PLoS One, June 5, 2019)
|
Three psychotherapies for depression reduce suicidal thoughts
 Photo for illustrative purposes only. ©iStock/SeventyFour (07/09/2019)
A VA Office of Mental Health and Suicide Prevention study looked at the effectiveness of three psychotherapies for depression at reducing suicidal thoughts. The researchers studied treatment data on interpersonal psychotherapy, cognitive-behavioral therapy, and acceptance and commitment therapy. The analysis showed that all three treatments reduced suicidal thoughts, especially in women Veterans. For male Veterans, decreases in suicidal thoughts were significantly greater in interpersonal psychotherapy and cognitive-behavioral therapy, compared with acceptance and commitment therapy. The results show that all three therapies are effective treatments for suicidal thoughts and depression, say the researchers. They suggest that more research be done on how gender influences the effectiveness of these treatments. (Women’s Health Issues, June 25, 2019)
|
Liver cancer risk remains after successful hepatitis C treatment
 Photo: ©iStock/Hailshadow (07/09/2019)
Patients treated with direct-acting antiviral agents for hepatitis C remained at risk for liver cancer after several years, found a Michael E. DeBakey VA Medical Center study. Hepatitis C increases the risk of liver cancer. Direct-acting antivirals are a new form of medication that are more effective than interferon—an older treatment—at treating hepatitis C. But their long-term effect on cancer risk is unknown. Researchers followed more than 18,000 patients at VA medical centers who had achieved sustained virologic response (meaning that no hepatitis C viruses were found in blood samples) with these new medications. They found that three years later these patients, while having lower cancer risk than people with active hepatitis C infection, still had risk levels that warrant monitoring. The risk was particularly high in patients with cirrhosis. The researchers recommend that hepatitis C patients treated with antivirals continue to be monitored for liver cancer. (Hepatology, June 20, 2019)
|
Collaborative care plus self-management of chronic pain and mood symptoms leads to best results
 Photo: ©iStock/MartinPrescott (06/27/2019)
Adding collaborative care by nurses and doctors to an automated self-management program improves outcomes for Veterans with chronic musculoskeletal pain and mood disorders. That is the main finding from a study at the Roudebush VA Medical Center in Indiana. Nearly 300 patients with both chronic pain and depression or anxiety were treated for 12 months. In addition to standard primary care—including medication as needed—one group received automated monitoring and web-based self-management modules. The other group received self-management along with collaborative care by a team of nurses and physicians, who were responsible for regular phone contact and optimized medication management. While both groups showed a trend toward symptom decline, the collaborative care group were more likely to report overall improvement and less likely to have worsening symptoms. (Journal of General Internal Medicine, June 21, 2019)
|
New insight on role of hippocampus in memory
 Photo: ©iStock/Vera_Petrunina (06/27/2019)
A study including researchers from the VA Boston Healthcare System found that the hippocampus is involved in consolidation of memory even when it is not involved in the initial learning. The hippocampus is a part of the brain involved in spatial memory and navigation. During sleep, the hippocampus helps convert short-term memories to long-term memories for tasks it was initially involved in. To test whether the hippocampus plays a role in other instances of memory formation, the researchers taught a simple motor task to people with hippocampal amnesia (meaning they couldn’t form long-term memories), and to control patients. While both groups showed similar initial learning, only the control group showed memory consolidation overnight, meaning they learned the task over the longer term. In the words of the researchers, “These results demonstrate that the hippocampus can be required for normal consolidation of a task without being required for its acquisition.” The results suggest that the hippocampus plays a broader role than previously thought in memory, they say. (Hippocampus, June 3, 2019)
|
Rat study: Single injection protects against TBI damage in short term
 Photo: iStock/gorodenkoff (06/27/2019)
In a rat study by VA Pittsburgh Healthcare System researchers, a single shot of the drug memantine protected against neurodegeneration caused by traumatic brain injury (TBI), although the effects did not last. Within hours of a TBI, levels of the neurotransmitter glutamate rise in the brain. This can cause cell damage and long-term neurological deficits. To counter this, the researchers gave brain-injured rats a single injection of memantine one hour after injury. Memantine, sold as Nemenda, blocks glutamate receptors in the brain, and is used to treat Alzheimer’s disease. The shot protected cortical tissue and reduced neuronal degradation one day after injury. It also protected the hippocampus from damage seven days after injury. Higher doses of memantine were more effective than smaller doses. Researchers did not see any adverse side effects from the drug in the rats. However, the benefits did not remain past five weeks. While memantine injections have potential to protect the brain from degradation after TBI, a single dose may not be enough for long-term benefits, say the researchers. (Restorative Neurology and Neuroscience, 2019)
|
Diabetes drug equally effective across groups
 Photo for illustrative purposes only. ©iStock/Jelena Danilovic (06/20/2019)
The diabetes medication empagliflozin reduces blood sugar levels for people with diabetes across a variety of demographics, found a VA Palo Alto Health Care System. Empagliflozin, sold as Jardiance, is a medication for reducing A1c (blood glucose) levels. Researchers looked at data on nearly 8,000 VA patients with Type 2 diabetes taking the drug. They found patients had an average of 0.7% reduction in A1c levels after six months on empagliflozin. Black and white patients had similar A1c reductions. Those with and without cardiovascular disease also had similar reductions. Patients with the highest A1c levels at baseline had the largest A1c reductions after six months. Patients also taking insulin had lower A1c reductions than those not taking insulin. (American Diabetes Association, June 9, 2019)
|
More study needed on TBI’s effect of psychiatric treatment
 Illustration ©iStock/laramenko (06/20/2019)
Evidence is lacking on how mild traumatic brain injury (TBI) affects treatment for psychiatric conditions, according to Minneapolis VA Health Care System researchers. The researchers conducted a literature review for studies on patients with mild TBI and several other conditions: PTSD, depression, substance use disorders, suicidal thoughts or attempts, and anxiety disorders. They found seven studies looking at mild TBI occurring with these conditions. None of the studies looked at treatment effectiveness for substance use disorder or suicidal thoughts. For the other conditions, TBI history did not affect treatment outcomes. However, the studies that were analyzed did not use control groups or a randomized trial design, making it hard to assess the strength of the evidence. More studies are needed on how TBI affects treatment for other psychiatric conditions, say the researchers. (Journal of Affective Disorders, June 1, 2019)
|
Breast cancer screening guidance
 Photo by Robin DeMark (06/20/2019)
The American College of Physicians released four guidance statements on breast cancer screening for average-risk women. A researcher from the Minneapolis VA Medical Center was part of the guideline committee. First, they recommend that clinician discuss whether or not to screen for breast cancer with women below age 50 since potential harms often outweigh the benefits in this age group. Second, for women 50 to 74, they recommend offering mammogram screening every other year. Third, they recommend discontinuing breast cancer screening for women age 75 or older, or for those with a life expectancy of 10 years or less. Fourth, for all age groups they say that clinicians should not use clinical breast examination to screen for breast cancer. (Annals of Internal Medicine, April 9, 2019)
|
Gene variants linked to habitual alcohol use
 Photo by Mitch Mirkin (06/13/2019)
Researchers with the VA Connecticut and Boston health care systems found five new locations on the human genome related to habitual alcohol use. Using VA’s Million Veteran Program, the researchers studied the genomes of 126,936 European American Veterans and 17,029 African American Veterans. They found habitual alcohol use—which could lead to alcohol dependence—was linked to gene variants at specific locations on the genome for both groups. One gene, ADH1B, is already known to influence alcohol dependence. Five other gene locations (the most significant of which is called CRHR1) also showed a link to increased habitual alcohol use. These five gene locations have not previously been associated with alcohol use. The results provide new insight into how genetics could affect harmful alcohol use, say the researchers. (Biological Psychiatry, April 8, 2019)
|
Lipid testing boosts statin adherence
 Photo: ©iStock/PongMoji (06/13/2019)
Routine lipid testing can lead to Veterans taking their statin medication more regularly, found a study by Michael E. DeBakey VA Medical Center researchers. The study looked at data on patients receiving care through VA for atherosclerotic cardiovascular disease. Researchers looked at medication refill data to see whether patients were taking prescribed statins. Patients with at least one lipid panel over a one-year period had a 66% chance of adhering to their medication, while those without a lipid panel had a 61% chance. Among new statin users, 68% adhered to their medication when they had a lipid panel within 4–12 weeks of beginning treatment. For those without a lipid panel, adherence was 59%. While the difference is modest, routine statin testing can significantly increase patient’s statin adherence, according to the researchers. (American Journal of Medicine, May 16, 2019)
|
Study: Almost all VA patients would benefit from gene tests to guide drug choice
 Photo: ©iStock/Nicolas_ (06/13/2019)
Almost all Veterans would benefit from genetic testing to see how they would react to various medications, according to a study of data from nearly 8 million Veterans. Specific gene variants affect how people respond to different drugs. The researchers looked at pharmacy and demographic data on 7.7 million Veterans who used VA pharmacies over a six-year period. They projected, based on the Veterans’ demographics, that 99% would have at least one gene variant that could affect their response to commonly used drugs. Common prescriptions in VA that could be affected by gene variation included simvastatin (sold as Zocor) for high cholesterol, tramadol (sold as Ultram) for pain, and warfarin (sold as Coumadin) for high blood pressure. Genetic testing could influence prescribing decisions for many Veterans, concluded the researchers. (JAMA Network Open, June 5, 2019)
|
New insight into how cancer spreads
 Illustration: ©iStock/Mohammed Haneefa Nizmudeen (06/04/2019)
An international study led by a researcher at the VA San Diego Healthcare System yielded new insight into how cancer spreads. The study focused on a protein known as Caveolin-1, or Cav-1, which scientists have found plays a role in cancer cell migration from a primary tumor into other areas of the body. The new study tested whether a particular part of this protein, called the caveolin scaffolding domain, or CSD, is critical in this process. The team engineered cancer cell lines into three categories. One over-expressed the entire Cav-1 protein. The second over-expressed the protein but without a working CSD. The third over-expressed green fluorescent protein, as a control. The researchers found that cancer cell migration was inhibited in the first group of cells, but increased in the second group, the cells without the CSD. The finding supports their theory that Cav-1 thwarts cell migration through its CSD. They write, “Modulating the CSD and targeting specific proteins may offer potential new therapies in the treatment of cancer metastasis.” Besides VA and a few other U.S. institutions, the work involved collaborators in Japan, Scotland, and Pakistan. (Cell Cycle, online May 22, 2019)
|
CPAP machines and insomnia
 Photo for illustrative purposes only. ©iStock/grandriver (06/04/2019)
Many people with sleep apnea—a potentially dangerous condition in which breathing repeatedly stops and starts during sleep—use a continuous positive airway (CPAP) device, which pumps air through the nose. VA researchers in Pittsburgh and colleagues looked at how CPAP therapy affected insomnia among patients with Type 2 diabetes and sleep apnea. Not surprisingly, they found that greater use of CPAP was associated with improvements in insomnia overall. Specifically, the therapy helped with difficulty staying asleep, and with early waking. However, CPAP use did not appear to help difficulty falling asleep. The researchers say it’s important to delve into the specific type of insomnia patients experience, and to understand the potential pros and limitations of CPAP for each type. (American Thoracic Society meeting, May 20, 2019)
|
Overuse of antibiotics in dental care
 Photo: iStock/sturti (06/04/2019)
A study led by investigators at VA’s Center of Innovation for Complex Chronic Healthcare found that the great majority of preventive antibiotic prescriptions written by dentists in the U.S. are not in accord with clinical guidelines, and are unnecessary. The team analyzed more than 168,000 dental visits involving more than 91,000 U.S. patients using commercial dental health plans. Per current guidelines, only patients with cardiac conditions who are at high risk for endocarditis, in which germs from other parts of the body, such as the mouth, spread to the heart, should receive prophylactic antibiotic treatment before invasive dental procedures. The study found that dentists, on the whole, operated well outside the guideline, and that 8 in 10 preventive antibiotic prescriptions were unnecessary. The researchers called the finding “worrisome,” in light of the ongoing crisis stemming from antibiotic overuse and the proliferation of drug-resistant bacteria. Though their data were from 2011–2015, and they note the situation has been “slowly improving,” they still called for better antibiotic stewardship in dentistry. (JAMA Network Open, May 3, 2019)
|
Rural Veterans have higher per-capita opioid use
 Photo: iStock/sassy1902 (06/04/2019)
Rural Veterans receive over 30% more opioids than their urban counterparts, found a study by VA’s Iowa-based Center for Comprehensive Access and Delivery Research and Evaluation. Using national data, the team examined how opioid prescribing varies by region in VA, and whether there are differences based on rural vs. urban status. They used a measure called “morphine milligram equivalents.” The average per-person use for VA patients in 2016 was 1,038 MME. The lowest use was in the Northeast: 894 MME. The highest was in the West, at 1,368 MME. Urban residents averaged 988 MME, compared with 1,306 for those in rural areas. Most of the difference was explained by more long-term opioid use by rural Veterans. Short-term use of the pain medications was similar. The researchers say the reasons for the disparity need to be studied further. It’s possible, they say, that rural Veterans don’t have equal access to non-drug pain treatment for chronic pain. (Military Medicine, May 21, 2019)
|
Tinnitus frequently occurs with mental health disorders
 Photo for illustrative purposes only. ©iStock/Ridofranz (05/29/2019)
A study of VA health care users found that nearly 4% met the diagnostic criteria for tinnitus, the perception of ringing, buzzing, or other noises in the ears. The prevalence estimate is based on a random, representative sample of more than 600,00 Veterans who received care in VA between 2011 and 2016. The study found that tinnitus was often co-diagnosed with hearing loss and traumatic brain injury. Tinnitus was also associated with mental health diagnoses, including anxiety, depression, and substance use disorders. While the study wasn’t designed to show cause-and-effect relationships between tinnitus and mental health, the researchers did stress the need for coordinated care between the two areas. A team at VA’s National Center for Rehabilitative Auditory Research led the study. (American Journal of Audiology, April 22, 2019)
|
Pinpointing genetic targets for meth addiction
 Photo: ©iStock/JTSorrell (05/29/2019)
Researchers at the Portland VA Medical Center and Oregon Health & Science University are working to understand genetic risk for methamphetamine addiction. In a recent experiment, they used mice that were genetically bred to crave methamphetamine. The researchers first identified two proteins that appear at higher-than-normal levels in the brains of those animals. One is a receptor for glutamate, the most abundant neurotransmitter in the brain, and is known as mGluR5. The other is a scaffolding protein known as Homer2a/b. There are no known drugs that target the latter protein, but there are several that target mGluR5. The next step was to test drugs known to bind to mGluR5 and make it less active. Those drugs, however, appeared to have little effect on the mice’s meth appetite. The researchers concluded that targeting mGluR5 may not be an adequate strategy, and that scientists will need to better understand the role of Homer2a/b in addiction. (International Behavioural and Neural Genetics Society meeting, May 2019)
|
Alert to curb antibiotic overuse
 Photo: ©iStock/busracavus (05/29/2019)
Researchers at the VA Western New York Healthcare System developed a new strategy for reducing inappropriate use of antibiotics. While antibiotics are critical life-saving drugs, their overuse has fueled drug-resistant strains of bacteria. Focusing on outpatient care, which accounts for the majority of antibiotic use, the researchers found that 4 in 10 patients among their sample of more than 1,000 Veterans received an inappropriate prescription. The drug that accounted for the most unnecessary prescriptions was azithromycin. More than half of the prescriptions for this antibiotic were deemed unnecessary. Respiratory infections were the most common conditions for which the drug was used inappropriately. This drug along with three others accounted for 80% of inappropriate prescriptions. The researchers designed an electronic alert, triggered when providers sign a prescription, that allows for real-time intervention to adjust the prescription before the patient leaves the office. They say focusing on the four drugs they identified, to start, will allow for maximum impact. They also recommend patient education to lessen the pressure that prescribers sometimes feel to “appease” the patient with an antibiotic. (American Journal of Infection Control, online March 9, 2019)
|
When to change the PTSD treatment plan
 Photo for illustrative purposes only. ©iStock/Wavebreakmedia (05/29/2019)
VA uses two main psychotherapies to treat PTSD—prolonged exposure, and cognitive processing therapy—and they are usually delivered in 8 to 12 weekly sessions. But a new study suggests that Veterans not seeing “meaningful” improvement after eight sessions are unlikely to do so in the remaining weeks of therapy. That’s the main finding from a study led by VA authors in Ann Arbor and Atlanta. The researchers examined the records of more than 2,200 Veterans. All of them had completed at least eight sessions of one evidence-based, trauma-focused psychotherapy or the other, as well as two self-report assessments, in which they answered questions about their PTSD symptoms. Those who reported at least 20% symptom reduction by session eight were twice as likely to go on to achieve “meaningful change”—defined by the researchers as a 50% reduction—in further sessions, compared with all those who continued treatment. For those not seeing meaningful change after eight weeks, the researchers recommend that clinicians consider changing the type or intensity of treatment. (Behavior Therapy, online May 18, 2019)
|
Men, women respond differently to 'acceptance and commitment therapy'
 Photo for illustrative purposes only. ©iStock/electravk (05/23/2019)
Men and women Veterans may respond differently to acceptance and commitment therapy (ACT) for emotional distress, according to a VA San Diego Healthcare System study. In ACT, patients are taught not to avoid negative emotions and experiences and learn abilities to help them act in a way that is in line with their values. ACT led to a greater decrease in PTSD symptom severity in women compared to present-centered therapy, whereas the two therapies had similar results in men. A similar trend was seen in changes in general emotional distress, although to a lesser extent than in PTSD. Women were more likely than men to recommend the treatment to a friend. The results underscore that gender differences in coping skills and reactions to stress should be taken into consideration when prescribing psychotherapy, according to the researchers. If future research confirms that women respond better to ACT, it could be important guidance for how to treat women Veterans with PTSD, they say. (Women’s Health Issues, May 3, 2019)
|
H. pylori treatment may raise risk of autoimmune disease
 Photo: ©iStock/iLexx (05/23/2019)
Drug treatment for H. pylori infection was linked to an increased risk of autoimmune disease, in a study including a VA Ann Arbor Healthcare System researcher. H. pylori is a type of bacteria that infects the digestive tract. It can cause ulcers and stomach cancer. About two-thirds of the world’s population has the bacteria in their bodies; most people don’t experience problems. Working with data on nearly 80,000 Taiwanese patients, the researchers found that patients treated to eradicate H. pylori infection had a significant increase in risk for autoimmune disease, including irritable bowel disease. The increased risk was not the result of general antibiotic treatment, since patients treated with antibiotics for urinary tract infections had lower autoimmune risk than H. pylori patients. The results suggest that H. pylori colonization could have immune system benefits, say the researchers. The study was published in the journal Clinical Gastroenterology and Hepatology last year, and more recently presented at a meeting. (Digestive Disease Week, May 21, 2019)
|
Brain injuries in women after intimate partner violence
 Photo: ©iStock/lolostock (05/23/2019)
A team including a VA Boston Healthcare System researcher summarized the research available on traumatic brain injuries (TBIs) in women as a result of intimate partner violence. They found that intimate partner violence-related TBIs are common, and women in these circumstances often have repetitive TBIs. These injuries are linked with a range of mental health problems, such as anxiety and depression, and with structural and functional brain damage. The authors make several recommendations for future research and clinical practice to address this issue, including using trauma screening tools and risk assessment. (Journal of Aggression, Maltreatment, & Trauma, March 12, 2019)
|
Residents and attending physicians provide similar care
 Photo: ©iStock/digitalskillet (05/15/2019)
Resident physicians and attending physicians provide equal quality of care in VA hospitals, found a VA Portland Health Care System study. Residents are doctors who are under the supervision of a more experienced attending physician. Researchers studied data on diabetes quality of care for more than 76,000 patients in 10 VA facilities across the country. Of those patients, 25% were cared for by a resident, while 75% were cared for by an attending physician. Quality-of-care measures were similar between both groups. While attending physicians have more experience, the results show that residents provide an important role in caring for patients, often caring for new patients and those from vulnerable populations. (JAMA Internal Medicine, April 1, 2019)
|
Study: Fewer hospitalizations for diabetes patients using both VA and Medicare
 Photo: ©iStock/EXTREME-PHOTOGRAPHER (05/15/2019)
Diabetes patients who used only VA medical care or Medicare rather than both systems together were more likely to have been hospitalized, in a study by researchers from the VA Greater Los Angeles and New Jersey health care systems. Researchers looked at data from 2007-2010 on more than 200,000 Medicare-eligible Veterans with diabetes. Patients who used both VA and Medicare for either primary or supplementary care were less likely to have a hospitalization during the study period. The study population was primarily older and had multiple complications related to diabetes. The results suggest that hospitalized older patients with diabetes may be so medically complex that they benefit from having more providers involved in their care, say the researchers. This need may outweigh the risk of care fragmentation that comes with using two different health care systems. (Medical Care, April 29, 2019)
|
Brain study ties proteins to ‘cognitive trajectory’ in aging
 Photo: ©iStock/malgorzata tatarynowicz (05/15/2019)
A group including Atlanta VA Medical Center researchers has identified protein markers in the brain that affect aging-related cognitive decline. The researchers followed 143 patients for up to 14 years to track whether they had any cognitive decline as they aged. Upon patients’ death, the researchers studied the donated brains. They found 579 proteins to be associated with cognitive trajectory. Specifically, patients who showed greater cognitive stability had increased levels of proteins involved with mitochondrial activities or synaptic function. These findings show markers that affect cognitive decline that have not been previously considered in cognitive status and Alzheimer’s disease diagnoses. The results suggest promising targets for future research on how cognitive ability changes as people age, say the researchers. (Nature Communications, April 8, 2019)
|
Tinnitus characteristics do not affect impact
 Photo for illustrative purposes only. ©iStock/Westbury (05/08/2019)
Perceived loudness and pitch do not change the impact of tinnitus, according to a VA Portland Health Care System study. Tinnitus is a sound—such as ringing or buzzing—in the ears when no outside sound is present. It is the No. 1 disability affecting Veterans. Researchers surveyed 223 participants on how they perceived tinnitus. They found that how loud the sound seemed to participants and the pitch of the noise was not related to how bothersome the tinnitus was. The results suggest that how patients react to tinnitus has a greater impact on their quality of life than how they perceive the sound, in terms of loudness, pitch, or other sound qualities. (American Journal of Audiology, April 22, 2019)
|
Algorithm for identifying PTSD in electronic health records
 Photo: ©iStock/Laurence Dutton (05/08/2019)
Researchers with VA’s Million Veteran Program have designed a computer algorithm to identify PTSD in electronic health records. Although PTSD may be noted in a patient’s electronic health record, researchers would need to read individual records to pick out patients with the condition for studies. The algorithm searches records for diagnoses and symptoms to classify patients as likely PTSD, possible PTSD, and likely not PTSD. The algorithm had high accuracy when compared with manual chart review. The algorithm could be useful for research and quality improvement endeavors within VA, say the researchers. A quick way to identify thousands of cases using electronic health records would help recruiting for large genome-wide association studies of PTSD. (Journal of Traumatic Stress, April 2019)
|
Osteoporosis drug treatment studies show both effectiveness and risk
 Photo for illustrative purposes only. ©iStock/Steve Debenport (05/08/2019)
Minneapolis VA Health Care System researchers reviewed the existing evidence on long-term drug therapy to prevent fractures in patients with osteoporosis. They surveyed 35 trials and 13 observational studies of various osteoporosis drugs. The literature shows that long-term treatment with alendronate acid or zoledronic acid, two drugs known as bisphosphonates, reduces fracture risk in women with osteoporosis. Long-term bisphosphonate treatment may increase risk for rare adverse events, but continuing this treatment beyond three to five years may reduce the risk of vertebral fractures. Another osteoporosis treatment, long-term hormone therapy, reduces hip fracture risks but has serious side effects, according to the literature. One limitation of the review is that the researchers did not find any studies involving male patients. (Annals of Internal Medicine, April 23, 2019)
|
Evidence lacking on use of massage for pain
 Photo: ©iStock/skynesher (05/01/2019)
A literature review by West Los Angeles VA Medical Center researchers found some evidence that massage is beneficial for pain, but the evidence was weak. The literature search turned up 32 high-quality systematic reviews on massage and pain. These studies showed potential benefits of massage for a wide variety of pain, including low back, neck, and cancer pain. However, the evidence was low-strength (meaning researchers were unable to confidently draw conclusions). Factors affecting the usefulness of massage included style, provider, duration, and other treatments used. Too few studies and not enough details are available to draw conclusions about the usefulness of massage for treating pain, according to the researchers. (Journal of Alternative and Complementary Medicine, March 20, 2019)
|
Treating alcohol problems: Does patient motivation matter?
 Photo for illustrative purposes only: ©iStock/sturti (05/01/2019)
Whether a Veteran receives alcohol use disorder treatment voluntarily or involuntarily does not affect treatment outcome, found a St. Cloud VA Health Care System study. Researchers looked at 120 Veterans being treated for alcohol use disorder in a residential rehabilitation treatment program. Half were admitted under recommendation by a court order. The others were admitted voluntarily. The researchers found no differences between groups in how long participants remained sober after they were discharged. The results show that patients’ motivation for treatment may not be a good predictor of treatment outcomes, say the researchers. (Journal of Addictions Nursing, Jan./March 2019)
|
Use of cardiac stress tests varies widely in VA
 Photo: ©iStock/SerafinoMozzo (05/01/2019)
The use of cardiac stress tests for ischemic heart disease patients varies widely across VA facilities, found a Michael E. DeBakey VA Medical Center study. Researchers studied treatment data on nearly 1 million Veterans with ischemic heart disease. The use of cardiac stress tests—such as treadmill exercise and stress echocardiography—varied by as much as 40%, depending on where treatment was received. Use ranged from 2 to 32 tests per 100 patients at different VA medical centers. The cause of this variation is not yet known. The results could suggest that some facilities are overusing this type of test, say the researchers. (JACC. Cardiovascular and Imaging, April 10, 2019)
|
Families give high marks to polytrauma care
 Photo: ©iStock/spxChrome (04/25/2019)
A majority of caregivers were satisfied with the inpatient care their loved ones received from VA, in a study of caregivers of Veterans in a VA Polytrauma Rehabilitation Center. Of the 524 caregivers surveyed, 75% were mostly or very satisfied with their loved ones’ inpatient care. Higher satisfaction was linked with greater caregiver social support, receipt of training from VA, and perceptions of being valued by VA. The authors say the results suggest that “supporting a strong social network for caregivers, providing caregiver training, and employing practices that communicate that family caregiving is valued by providers and healthcare organizations are promising avenues for improving caregiver satisfaction.” (PLoS One, March 15, 2019)
|
Stress inoculation training shows promise for PTSD
 Photo for illustrative purposes only. ©iStock/asiseeit (04/25/2019)
Stress inoculation training can reduce PTSD and depression symptoms in patients with PTSD and traumatic brain injury, found a VA Northern California Health Care System study. Stress inoculation training is a psychotherapy that teaches patients to prepare themselves in advance to handle stressful events. In the study of 56 Veterans, the majority had significant reductions in PTSD and depression symptoms, better perceived stress tolerance, and improved social and occupational functioning. Eighty-eight percent followed through with recommended follow-up treatment. Stress inoculation training could be a useful treatment for patients who do not want to participate in trauma-focused therapies such as prolonged exposure, according to the researchers. (Psychological Trauma, March 21, 2019)
|
Brain thickness measure linked to better attention
 Illustration: ©iStock/Lars Neumann (04/25/2019)
Cortical thickness is linked with sustained attention, according to a study by VA Boston Healthcare System researchers. The cortex is the outer layer of the brain, and is divided into different sections related to various functions. The researchers took high-resolution MRI scans of the brains of 125 participants. The participants then took performance tests to measure how well they could maintain attention. Better attention was linked to more thickness in the visual, somatomotor, frontal, and parietal cortices of the brain, especially in the right hemisphere. Different regions of the cortex also connect and work together to form networks for specific functions. Several networks of brain regions—including two known to be linked to attention—were thicker in participants with better sustained attention. The results show that structural MRI could help explain differences in cognition, say the researchers. (Human Brain Mapping, April 13, 2019)
|
Mixed reports from women Veterans on their family-planning experiences
 Photo for illustrative purposes only. ©iStock/PeopleImages (04/24/2019)
Women Veterans had both negative and positive experiences with family planning in the military and VA, in a study by VA Puget Sound and Pittsburgh health care system researchers. Researchers interviewed 32 women Veterans about their family planning care. Nearly all described negative experiences in military or VA health care. These included perceived gender-based discrimination and pressure to choose certain contraceptive methods, judgment of reproductive choices, and lack of continuity with providers. Some women also reported positive family planning experiences in VA. These included feeling respected, receiving comprehensive information about options, and having their perspectives and concerns considered. Women preferred counseling that included providers initiating and validating family planning discussions. Establishing trust and avoiding judgment, asking women’s individual preferences, and engaging them as equal decision-making partners were also important. The results provide key insights that could improve family planning care in VA, say the researchers. (Women’s Health Issues, April 10, 2019)
|
Weight management boosts quality of life in serious mental illness
 Photo: ©iStock/emesilva (04/24/2019)
Both in-person and web-based weight management programs improved quality of life for patients with serious mental illness, in a study by Baltimore VA Medical Center researchers. Patients with serious mental illness are often at greater risk for obesity. Researchers analyzed outcomes for patients participating in the in-person MOVE! weight management program or the online version, WebMOVE. Participants in the in-person program showed decreases in loneliness, compared with normal care, after six months. Those in WebMOVE had increases in weight-related self-esteem after six months. Both groups had significant increases in health-related quality of life, compared with patients in usual care. The results show that both in-person and web-based weight management counseling can promote “holistic” recovery for patients with serious mental illness, according to the researchers. (Society of Behavioral Medicine Annual Meeting, March 7, 2019
|
Researchers grow axons in lab
 Photo: ©iStock/Henrik5000w (04/24/2019)
A team including a Corporal Michael J. Crescenz VA Medical Center researcher have found a way to create brain axons in the lab. Axons are long, slender fibers projecting from neurons that conduct electrical impulses. Brain damage to the white matter often leads to permanent neurological problems because axons are not known to regenerate much. The researchers used stem cells to generate cortical neurons. Using a technique called axon stretch growth, they were able to grow axon tracts at a rate of one millimeter per day. The technique could potentially make it possible to transplant axons into the brain after injury, say the researchers. (Tissue Engineering Part A, March 29, 2019
|
Parkinson’s patients more likely to get recommended care with new model
 Photo: ©iStock/noipornpan (04/11/2019)
A new method of disease management led to improved care processes for Parkinson’s patients, in a study by VA Greater Los Angeles Healthcare System researchers. The study recruited 328 Veterans with Parkinson’s disease at five VA medical centers in California. Half were treated using a nurse-led chronic model called CHAPS. The rest received usual care. The CHAPS group had substantially higher adherence to quality of care indicators, such as assessment of symptoms, counseling, and palliative care. The only patient-centered difference was improvements on a depression screen in the CHAPS group. While this care model shows potential to improve Parkinson’s disease treatment, more refinement is needed to improve patient-centered outcomes, say the researchers. (Neurology, March 22, 2019)
|
Molecular delivery system takes arthritis drugs directly to joints
 Photo: ©iStock/Tharakorn (04/11/2019)
Baltimore VA Medical Center researchers developed a technique to deliver arthritis medication directly to the joints. Rheumatoid arthritis drugs can cause bad reactions when healthy organs are exposed. The researchers developed a molecular substance (a peptide ligand called ART-2) that could home in on inflamed joints. A molecular structure called a liposome is coated in ART-2, with the arthritis drug inside. When injected into the body, the drugs go directly to inflamed joints, meaning that other organs are not exposed. When given to rats, the therapy was more effective at stopping arthritis than injection of the same drug without the ART-2. This type of treatment could have many advantages over conventional arthritis therapy, according to the researchers. (Nanomedicine (London), April 2, 2019)
|
Racial mortality disparities in VA
 Photo: ©iStock/Andresr (04/11/2019)
VA has reduced many racial disparities in mortality, but differences in risk of death based on race still exist in some areas, found a VA Portland Health Care System study. Racial and ethnic health disparities have been a major problem in U.S. health care, both in the private sector and in VA. A literature review found that black and white Veterans receiving care through VA have similar overall rates of mortality. This could be due to VA’s commitment to equal access to care, according to the researchers. However, black Veterans did have higher mortality from certain conditions: chronic kidney disease, colon cancer, diabetes, HIV, rectal cancer, and stroke. American Indian and Alaska Native Veterans undergoing noncardiac major surgery had higher mortality rates than other groups. Some studies also showed Hispanic Veterans with HIV or traumatic brain injury having higher mortality. Because most studies compare black and white Veterans, more research is needed on health care disparities for other racial and ethnic groups, say the researchers. (American Journal of Public Health, March 2018)
|
Post-9/11 Veterans less likely to delay mental health care
 (Photo for illustrative purposes only. DoD/Navy Petty Officer 1st Class Daniel Barker) (04/05/2019)
Post-9/11 Veterans were less likely than others to delay treatment for common psychiatric conditions, according to a study by VA Puget Sound Health Care System researchers. In a study of almost 15,000 people, post-9/11 Veterans were less likely to delay treatment for PTSD and depression than pre-9/11 Veterans or civilians. No differences in treatment time existed between groups for alcohol use disorder. Post-9/11 Veterans with health care coverage from VA in the past year tended to seek out depression treatment earlier than post-9/11 Veterans without VA coverage, pre-9/11 Veterans, and civilians. The results may reflect efforts to engage recent Veterans in mental health care, say the researchers. (Psychiatric Services, March 7, 2019)
|
Tailored medical homes provide better experience to homeless Vets
 Photo: ©iStock/Solange_Z (04/05/2019)
Patient-centered medical homes offer a better care experience to homeless Veterans compared with standard primary care, found a study of more than 11,000 patients. In 2012, select VA facilities implemented a homeless-tailored medical home model, called Homeless Patient Aligned Care Teams. Researchers surveyed patients enrolled in H-PACTs, along with those receiving standard care at facilities both with and without H-PACTs. H-PACT patients were more likely than standard-care patients at the same facility to report positive experiences in five domains: access, communication, office staff, provider ratings, and comprehensiveness. Standard-care patients at facilities with H-PACT programs were more likely to report positive experiences with communication and self-management support, compared with patients at facilities without H-PACT. The lessons learned from the program can be applied throughout the VA system to improve care, according to the researchers. (Medical Care, April 2019)
|
Sedative prevents neuron cell growth after TBI
 Photo: ©iStock/Henrik5000w (04/05/2019)
The sedative diazepam prevented neurogenesis after a traumatic brain injury, in a mouse study by Portland VA Health Care System and Oregon Health & Science University researchers. The growth of new neuron cells in the hippocampus increases significantly after TBI. This can be positive and lead to recovery. It can also be negative and lead to conditions such as epilepsy if the cells do not form correctly. The researchers found that diazepam almost completely prevented the TBI-induced increase in hippocampal neurogenesis in brain-injured mice. While limiting this cell growth could lead to some cognitive impairment, it also prevented aberrant cell growth that causes problems after TBI. According to the researchers, more study is needed on how benzodiazepines such as diazepam could help or hinder recovery from TBI. (Journal of Neurotrauma, Feb. 22, 2019)
|
Increased cleaning time may not improve hospital room disinfection
 Photo by Mitch Mirkin (03/27/2019)
More time spent cleaning patient rooms in a hospital may not improve disinfection, found a Central Texas Veterans Healthcare System study. Researchers measured the infectious bacteria count on five room surfaces in a VA medical center—bedrail, tray table, call button, toilet seat, and bathroom handrail—after cleaning in between patients. For some rooms, cleaning time was limited to 25 minutes, while for others cleaning time was unlimited. Longer time spent cleaning did not lead to fewer infectious organisms on surfaces. The results suggest that time spent cleaning beyond 25 minutes may not be necessary to properly disinfect a hospital room, as long as appropriate disinfectants are used and staff is properly trained, say the researchers. (Infection Control and Hospital Epidemiology, March 25, 2019)
|
The link between TBI and dementia
 Photo: ©iStock/gorodenko (03/27/2019)
Portland VA Health Care System researchers examined the existing evidence on the link between traumatic brain injury and dementia. Evidence suggest that dementia rates are similar between Veterans and non-Veterans age 65 and older. Multiple studies link TBI with increased risk of dementia in both Veterans and the general population. In Veterans, studies suggest that dementia risk grows progressively larger with higher levels of TBI severity. The researchers identified several evidence gaps where more study is needed. Not many studies have directly compared dementia rates in Veterans and non-Veterans. More research is also needed into the link between TBI and early-onset dementia, as well as into the mechanisms of how TBI raises dementia risk. (VA Evidence Synthesis Program, February 2019)
|
Gene variant interacts with stress to accelerate aging
 Photo: ©iStock/zmeel (03/27/2019)
Psychological stress was linked with advanced cellular aging in people with a specific gene variant, in a VA Boston Healthcare System study. Researchers looked at the genotypes of 309 Veterans to see how variants of the longevity gene klotho affected biomarkers of epigenetic age. Epigenetic age refers to how much DNA methylation (a process in which methyl molecules attach to DNA molecules, which can hamper DNA transcription) has occurred, and can be used as a biomarker of how much cells have aged. In some people, epigenetic age can exceed chronological age, which can predict higher mortality risk. They found that a specific form of the gene (rs9315202) interacted with PTSD, sleep disturbances, and pain to predict accelerated epigenetic age. This gene variant also interacted with PTSD to predict inflammation and lower white-matter neural integrity. A different form of the same gene (rs9527025) predicted a slowed epigenetic age. The results suggest that enhancement of the protein produced by the klotho gene could be a treatment target for patients with this gene variant, say the researchers. (Brain, Behavior, and Immunity, March 11, 2019)
|
Higher rates of insomnia drug overprescribing in women Veterans
 Photo: ©iStock/Martin Dimitrov (03/20/2019)
Women are more likely than men to be inappropriately prescribed the insomnia drug zolpidem (sold as Ambien) within VA, found a Bedford VA Medical Center study. Researchers looked at prescribing data for more than 500,000 Veterans taking zolpidem. They found that 30 percent of female Veterans taking the drug received an inappropriately high dose of zolpidem, compared with only 0.1 percent of male Veterans. Nearly 19 percent of those women had a prescription to both zolpidem and benzodiazepine, while 14 percent of men did. Benzodiazepine is another insomnia drug that is also used to treat other conditions such as anxiety and seizures. Drug interactions between zolpidem and benzodiazepine are linked with increased hospitalizations. Younger women and those with substance use disorders were more likely to receive too-high doses of zolpidem. Women with anxiety or schizophrenia and men with cancer, anxiety, or schizophrenia were more likely to have overlapping prescriptions. Guidelines recommend lower doses of zolpidem for women than men because of metabolism differences, but many women may still be prescribed similar doses to men. The results show that more attention is needed to gender-specific dosing, say the researchers. (American Journal of Managed Care, March 1, 2019)
|
Study finds low adherence to hormone therapy guidelines
 Photo for illustrative purposes only.©iStock/Highwaystarz-Photography (03/20/2019)
Adherence to prescribing guidelines for systemic hormone therapy for menopausal symptoms was low among VA providers, in a VA Greater Los Angeles Healthcare System study. Systemic hormone therapy with estrogen is effective in treating menopausal symptoms such as hot flashes and insomnia. Researchers looked at prescribing in four VA facilities across three states to see how well dosage guidelines were followed. Average guideline adherence was 58 percent. Adherence was highest with new prescriptions, at 74 percent. An inappropriately high dose was used in new prescriptions more than half the time. Most renewals were at a high dose, and only 16 percent had a documented rationale for the dosing. Among 116 prescriptions for systemic estrogen, progesterone was not prescribed in eight cases. Failure to co-prescribe progesterone puts women at increased risk for endometrial cancer. Intervention is urgently needed to improve guideline adherence, say the researchers. They also suggest similar studies should be done in community settings to see how widespread the problem is. (Journal of Healthcare Quality, March/April 2019)
|
Women’s health care expenses rise after death of a spouse
 Photo for illustrative purposes only. ©iStock/Tinpixels (03/20/2019)
Bereavement is linked with increased health care spending for women, according to a study by Boston VA Healthcare System researchers and colleagues. The researchers looked at Medicare spending of older adults for the two years before an after their partners’ death. Women increased their health care spending by an average of $625 per quarter after the death of a spouse. There was no significant increase for males who survived their spouses. The increase for women may be because they pay more attention to their own health once they are no longer acting as caregivers for their spouses, according to the researchers. More study is needed to find out why men and women have different patterns of health care spending after the death of a spouse, they say. (PharmacoEconomics, March 13, 2019)
|
Long-term posttraumatic stress tied to changes in brain structure
 Photo: ©iStock/Utah778 (03/13/2019)
Posttraumatic stress symptoms can persist decades after trauma exposure and are linked to lower hippocampal volume, according to a study featuring VA San Diego Healthcare System researchers. The study assessed PTSD symptoms in 247 men at two times: when each man was an average age of 38, and again when they were an average age of 62. Participants were Veterans who served during the Vietnam era and had experienced trauma before the first assessment. At the first time point, 8 percent of participants met criteria for presumptive PTSD. At the second time point, 6 percent did, showing that PTSD symptoms remained mostly stable over the 24-year period. Posttraumatic stress symptoms at both times were linked to lower volume of the hippocampus and other brain regions. Participants who had worse symptoms at time 2 had smaller hippocampal volume than they had at time 1. The study confirms what other research has shown, that posttraumatic stress symptoms are present years after trauma, even in the absence of a PTSD diagnosis. The results show that this symptom persistence is highly related to changes in brain structure, say the researchers. (Brain Imaging and Behavior, March 4, 2019)
|
TBI and PTSD increase tinnitus risk
 Photo for illustrative purposes only. ©iStock/Westbury (03/13/2019)
Traumatic brain injury and PTSD increase the risk for tinnitus, found a VA San Diego Healthcare System study. Tinnitus refers to hearing sound—such as ringing in the ears—when no external sound is present. Researchers assessed the hearing of 2,600 Marines before and after combat deployment. They found that both PTSD and TBI, particularly blast TBI, were linked to worsening tinnitus. Tinnitus progression also increased with hearing loss. Pre-deployment tinnitus was also likely to continue or worsen after deployment. Screening for PTSD, TBI, and hearing loss may allow for more focused treatment for tinnitus, say the researchers. (Military Medicine, Feb. 22, 2019)
|
Study sheds light on pesticides-Alzheimer’s link
 Photo: ©iStock/SVproduction (03/13/2019)
A team including two VA researchers have found a possible mechanism for how exposure to pesticides increases the risk of Alzheimer’s disease. Occupational exposure to organophosphate pesticides—such as experienced by agricultural workers—has been shown to increase the risk of Alzheimer’s disease. The researchers exposed rats to the chemical chlorpyrifos to simulate this pesticide exposure. Exposure resulted in dysregulation of microglial cells (a type of cell involved in the immune defense of the brain and spinal cord). Exposed rats showed accelerated neurodegeneration. The neurodegeneration was more severe in male rats, and only male rats showed cognitive impairment over 20 months. The results suggest that future treatments to preserve or restore the microglia could help prevent Alzheimer’s disease in people exposed to pesticides, according to the researchers. (NPG Aging and Mechanism of Disease, Jan. 22, 2019)
|
Testosterone replacement with exercise boosts muscle mass after spinal injury
 Photo: ©iStock/vadimguzhva (03/08/2019)
Low-dose testosterone replacement therapy paired with resistance training can lead to improved muscle mass and health in spinal-cord-injured patients, according to a Hunter Holmes McGuire VA Medical Center study. Loss of muscle mass is often a problem in patients with spinal cord injury. Patients underwent twice-weekly resistance training for 16 weeks, using ankle weights and electrical stimulation to activate the paralyzed muscles in their legs. They were also given testosterone replacement therapy via a patch. Patients receiving both testosterone and resistance training had improved body lean mass, muscle mass, and knee extensor strength. The patients also showed trends in less body fat, increased metabolic rate, glucose effectiveness, and inflammatory response. The results suggest that low-dose testosterone replacement therapy could ease the negative muscle and metabolic effects of spinal cord injury. (Journal of Neurotrauma, Feb. 22, 2019)
|
Cheese may increase prostate cancer risk for men with gene variant
 Photo: ©iStock/lechatnoir (03/08/2019)
The amount of cheese eaten may interact with specific gene variants to greatly increase the risk of prostate cancer, found a VA Portland Health Care System study. Researchers studied the genomes of 187 patients with prostate cancer and 306 controls without cancer. They looked at how 31 different dietary factors interacted with six genes known to be related to prostate cancer risk. They found that, for patients with a specific variant of one of the genes, each additional daily serving of cheese increased the risk of prostate cancer 16-fold. Past research has linked dairy to prostate cancer risk. In the new study, prostate cancer risk decreased by 37 percent per daily serving of fruits in the same group. The results suggest that patients’ diet and genetic variation can interact to affect their risk of prostate cancer, say the researchers. (12th Annual Multi-Institutional Prostate Cancer Program Retreat, March 3, 2019)
|
Understanding a cause of aortic aneurysm
 Illustration: ©iStock/mr.suphachai praserdumrongchai (03/08/2019)
A team including a researcher from the Harry S. Truman Memorial Veterans’ Hospital used a mouse model to explore the underlying causes of abdominal aortic aneurysm. An aortic aneurysm is when the aorta (the largest artery in the body, which carries blood from the heart to the rest of the body) becomes enlarged. This can cause it to rupture, leading to death. The researchers found that a deficiency of a protein called IL12p40 can lead to aortic aneurysm. It does this by leading to a build-up of M2 macrophages—white blood cells that decrease inflammation. This can lead to aortic stiffness and damage to the cellular matrix. The results suggest that, for aortic health, balance is needed between M2 macrophages and M1 macrophages—white blood cells that promote inflammation. (Arteriosclerosis, Thrombosis, and Vascular Biology, February 2019)
|
Sleep habits predict mortality
 Photo for illustrative purposes only. ©iStock/monkeybusinessimages (02/28/2019)
Sleep quality and duration are useful in predicting mortality, according to a study including a Minneapolis VA Health Care System researcher. Researchers looked at health data on more than 8,000 older adults, covering an average of 13 years. Using machine learning programs, they found that a multidimensional set of sleep factors was a significant predictor for all-cause and cardiovascular mortality. The most predictive sleep characteristics were time spent in bed, time to bed, wake-up time, and napping habits. Sleep was less predictive of all-cause mortality than factors such as demographics, physical health, or medication but more predictive than health behaviors such as smoking or drinking alcohol. The results suggest that developing comprehensive tools to measure sleep quality and habits could help predict mortality risk, say the researchers. They add that such tools could also aid in working with patients to improve their sleep habits. (Journal of Gerontology, Feb. 18, 2019)
|
For those with chronic illness, brief cognitive behavioral therapy reduces suicidal thought
 Photo for illustrative purposes only. ©iStock/asiseeit (02/28/2019)
Brief cognitive behavioral therapy (bCBT) can reduce suicidal thoughts, found a Michael E. DeBakey VA Medical Center study. Cognitive behavioral therapy is a psychotherapy that focuses on changing thoughts and behaviors that contribute to emotional distress. Patients with congestive heart failure or chronic obstructive pulmonary disease who also had depression and anxiety symptoms received four months of bCBT. Those who received bCBT were less likely to have suicidal thoughts after treatment, compared with patients who received usual care. They were also less likely to have suicidal thoughts four, eight, and 12 months after treatment. The results suggest that bCBT delivered in primary care can reduce suicidal ideation, even when the therapy does not directly target suicide. (General Hospital Psychiatry, Feb. 8, 2019)
|
Loved ones’ support helps keep Veterans in PTSD treatment
 Photo: ©iStock/PeopleImages (02/28/2019)
Support of loved ones is important to keeping Veterans from dropping out of PTSD treatment, found a Minneapolis VA Health Care System study. Researchers interviewed Veterans undergoing prolonged exposure therapy or cognitive processing therapy—two forms of psychotherapy considered the gold standard for PTSD care—at four VA medical centers. They found that Veterans whose loved ones encouraged them to participate in treatment and face distress were twice as likely to remain in PTSD treatment, compared with those without such support. The researchers concluded that providers should routinely assess how much support for treatment Veterans are getting at home. (Journal of Consulting and Clinical Psychology, March 2019)
|
Early palliative care may help avert unhelpful chemotherapy
 Photo: ©iStock/Pornpak Khunatorn (02/20/2019)
Early palliative care led to less receipt of unhelpful chemotherapy in patients with advanced lung cancer, in a study by VA Portland Health Care System researchers. Chemotherapy is not recommended for patients with advanced lung cancer because it is unlikely to be helpful. However, many patients continue to receive it anyway. Researchers studied more than 23,000 patients with late-stage lung cancer over a seven-year period. Of those, 37 percent received palliative care within 90 days of cancer diagnosis. Forty-five percent of the total group received chemotherapy. Thirty-four percent of patients who received early palliative care also received chemotherapy, compared with 51 percent who did not receive early palliative care. Those who received early palliative care also had lower rates of high-intensity chemotherapy. According to the researchers, early palliative care may optimize patient selection for chemotherapy. This could lead to less use of high-intensity therapy, promoting a focus on quality of life in accordance with patients’ performance, preferences, and care goals, they say. (Journal of Thoracic Oncology, February 2019)
|
Educational tool helps patient understand electronic health records
 Photo for illustrative purposes only. ©iStock/shapecharge (02/20/2019)
A resource called NoteAid led to better patient understanding of medical notes within their electronic health records, found a study headed by a Bedford VA Medical Center researcher. NoteAid is a freely available Web-based tool to help patients learn more about a diseases and conditions mentioned in their electronic health records. The system identifies medical concepts within doctor notes and provides links to lay definitions and resources. Patients given access to NoteAid scored higher on a test of comprehension for medical notes within their records, compared with a baseline group and patients given a passive educational resource. The results show that tools such as NoteAid can help patients better understand their own electronic health records. (Journal of Medical Internet Research, Jan. 16, 2019)
|
Androgen deprivation therapy may increase depression risk
 Photo: ©iStock/Luso (02/20/2019)
Androgen deprivation therapy was linked to an increased risk of depression in men with prostate cancer, in a VA San Diego Health Care System study. Prostate cancer cells require androgen hormones (such as testosterone) to grow. Reducing the level of these hormones can prevent the cancer cells from growing. Researchers looked at nearly 40,000 Veterans with prostate cancer who were treated with radiation therapy. Those also treated with androgen deprivation therapy had higher rates of new depression diagnoses and outpatient psychiatric services, compared with those not given the therapy. This group did not have higher rates of inpatient psychiatric use or suicide. The results may provide further evidence for the long-term risks of androgen deprivation therapy, say the researchers. (Cancer, Feb. 12, 2019)
|
Rat study: Brain injury can cause PTSD without psychological stressors
 Photo: ©iStock/fotografixx (02/14/2019)
A mouse study by James J. Peters VA Medical Center researchers found that PTSD can occur after a traumatic brain injury even without a corresponding psychological trauma. PTSD and TBI often occur together in Veterans, but it is difficult to separate their effects. The researchers exposed rats to repetitive low-level blasts while the rodents were under anesthesia. The rats showed anxiety and PTSD-like behavior for at least nine months after the exposure, even though they had been spared significant psychological stress because of the anesthesia. Exposing the rats to predator scent stress months after the blast exposure also caused a PTSD response. This showed the researchers that mild TBI may make the brain more sensitive to future psychological stress. The researchers also found that a specific experimental compound reversed PTSD-related behaviors in the blast-exposed mice, suggesting that it could one day be used to treat such injuries in humans. (Neuropharmacology, February 2019)
|
‘Next-step’ depression treatment medications are cost-effective
 Photo: ©iStock/asiseeit (02/14/2019)
Adding a second drug to standard depression treatment is cost-effective, according to a VA Palo Alto Health Care System study. Researchers compared three common alternate treatments for depression: standard antidepressant therapy plus aripiprazole, standard therapy plus bupropion, and switching to bupropion from a different antidepressant. Aripiprazole, sold as Abilify and other brands, is commonly used to treat schizophrenia and bipolar disorder. Bupropion, sold as Wellbutrin or Zyban, is an antidepressant and smoking-cessation aid. Health care costs were similar between treatment groups. The aripiprazole group had the highest depression remission rate. The group that supplemented treatment with bupropion had a higher remission rate than the bupropion-only group. The results show that augmenting standard depression therapy with a “next-step” treatment is cost-effective and could be useful, say the researchers. (Journal of Clinical Psychiatry, Dec. 18, 2018)
|
Many patients taking PPIs concerned about adverse effects
 Photo for illustrative purposes only. ©iStock/LumiNola (02/14/2019)
Concern about proton pump inhibitors is common and leads to attempts to discontinue the medication, found a VA Ann Arbor Healthcare System study. Researchers surveyed 755 patients with gastroesophageal reflux disease who took PPIs. PPIs—brands such as Prilosec, Prevacid, and Nexium—are a class of drugs that reduces stomach acid production. Thirty-three percent of patients were slightly concerned, 32 percent were somewhat concerned, and 14 percent were extremely concerned about adverse effects of PPIs. Of the 39 percent of patients who attempted to stop taking their PPI, 83 percent did so without a doctor’s recommendation. Patients more concerned about adverse effects were more likely to stop taking their PPIs. The results show that doctors should proactively discuss the risks and benefits of PPIs with patients to avoid unwise care decisions, say the researchers. (American Journal of Gastroenterology, February 2019)
|
Harassment of women Veterans by male Veterans common at VA medical centers
 Photo for illustrative purposes only. ©iStock/Zinkevych (02/06/2019)
Harassment of women Veterans by male Veterans at VA medical centers is prevalent, found a VA Greater Los Angeles Health Care System study. Researchers surveyed more than 1,000 women Veterans who used VA health care at any one of 12 facilities. One in four women said they experienced inappropriate or unwanted comments or behavior from male Veterans on VA grounds. The negative interactions included catcalls, sexual remarks, and denigration of Veteran status. Reports of harassment were more common among women with histories of military sexual trauma; other trauma exposure; anxiety, depression, or PTSD; and poorer health. Not surprisingly, women experiencing harassment were significantly less likely to feel welcome at VA and were more likely to not feel safe. Importantly, they were also more likely to delay or miss care. More efforts are needed to make VA health care facilities more inclusive, welcoming, and respectful of women Veterans, say the researchers. (Women’s Health Issues, Jan. 24, 2019)
|
Mechanism behind COPD lung damage
 Photo: ©iStock/wwing (02/06/2019)
Researchers with the Birmingham VA Medical Center and colleagues have shown a possible mechanism for how lung damage occurs in chronic obstructive pulmonary disease (COPD). The researchers showed that inflammatory cells in the lung produce specific proteins that can damage specific critical structural proteins in lung tissue. Particles related to a type of white blood cell bind to and cause damage to the extracellular matrix of the lungs. The neutrophils were found in the lungs of patients with COPD, but not healthy patients. The finding points to a number of approaches for therapies to reduce the progression of lung damage in Veterans with COPD, according to the researchers. (Cell, Jan. 10, 2018)
|
Melamine promotes kidney stone formation
 Photo: ©iStock/Xsandra (02/06/2019)
Researchers with the Washington DC VA Medical Center explored how melamine can contribute to the formation of kidney stones. Melamine is a type of plastic that can sometimes find its way into the body through products such as plastic tableware. The researchers showed that melamine can promote the forming of crystals of calcium phosphate and calcium oxalate—two substances that commonly make up kidney stones—through chemical reactions. The results will add to the knowledge of how kidney stones form and help scientists understand how melamine acts as an environmental toxin, say the researchers. (Scientific Reports, Jan. 29, 2019)
|
Neuropathy drives balance problems in HIV
 Photo: ©iStock/memorisz (02/01/2019)
Neuropathy (nerve damage) can cause balance problems in older people with HIV, according to a study by VA San Diego Healthcare System researchers. Looking at more than 3,000 patients, the researchers found that patients with HIV were more than twice as likely than HIV-negative patients to have had balance problems within the last 10 years. In both groups, patients with diagnosed chronic distal sensory polyneuropathy (cDSPN)—loss of feeling in the toes and feet—had more balance problems than those without. The results show that balance problems caused by neuropathy were more frequent in HIV-positive patients. Older patients with HIV should be assessed for cDSPN to prevent falls, say the researchers. (Journal of Acquired Immune Deficiency Syndromes, Jan. 3, 2019)
|
Chronic hypoxia a risk factor for suicide
 Illustration: ©iStock/yodiyim (02/01/2019)
Chronic hypoxia is a risk factor for suicide, found a White River Junction VA Medical Center study. Hypoxia is when the body does not get enough oxygen. The researchers looked at data on more than 9 million patients, a little over 22,000 of whom died by suicide. They assessed three causes of chronic hypoxia: altitude, smoking, and chronic obstructive pulmonary disease (COPD). Patients who had at least one of the three hypoxia conditions had a significantly increased risk of suicide. Current smokers had nearly two-times greater odds of dying by suicide than those who never smoked. Suicide risk increased as the elevation where a person lives increased. Having multiple hypoxia conditions greatly raised odds of suicide. Patients with all three conditions were nearly four times more likely to die by suicide than patients with no conditions. Patients with these risk factors may need specialized treatments to prevent suicide, say the researchers. (Psychiatry Research, Jan. 12, 2019)
|
Compounds emerge as potent tools against toxoplasmosis and malaria
 Photo by Michael Moody (02/01/2019)
VA Portland Health Care System researchers identified highly effective chemical compounds for fighting toxoplasmosis and malaria. Toxoplasmosis is a disease that can cause vision loss, neurological problems, and death. It is caused by the microscopic parasite Toxoplasma gondii. The researchers tested chemical compounds called endochin-like quinolones (ELQs). They found that the ELQs can stop T. gondii proliferation, even when the parasite is drug-resistant. These compounds may also be effective against malaria, which is caused by a parasite similar to T. gondii. Understanding the chemical interactions involved with these compounds could lead to safer and more effective treatment for toxoplasmosis and malaria. (ACS Infectious Diseases, Nov. 9, 2018)
|
Therapeutic horseback riding can lower PTSD symptoms
 Photo: ©iStock/DragonImages (01/24/2019)
Therapeutic horseback riding could effectively lower PTSD symptoms in Veterans, found a study by Harry S. Truman Memorial Veterans’ Hospital researchers and colleagues. After three weeks of a horseback riding program, participants had a 67 percent greater chance of having lower PTSD symptoms, compared to a waitlisted group. The likelihood of lower symptoms was 88 percent greater after six weeks. The results show that longer participation leads to better results in self-efficacy and emotion regulation. The study also identified several steps that could make therapeutic horseback riding programs more effective, such as providing transportation to the riding center and child care during classes. (Military Medical Research, Jan. 19, 2018)
|
Research limited on electrical brain modulation for PTSD
 Photo by Kimberly DiDonato-Ferro (01/24/2019)
Evidence is limited on the effectiveness of neuromodulation strategies to treat PTSD, according to a review led by a VA Greater Los Angeles Healthcare System researcher. In neuromodulation, electric currents or fields are applied to the head to influence brain circuits. The researchers looked for published studies on multiple techniques: electroconvulsive therapy, repetitive transcranial magnetic stimulation, transcranial direct current stimulation, vagus nerve stimulation, trigeminal nerve stimulation, and deep brain stimulation. While these techniques have had some success in treating other neurological disorders—such as depression and schizophrenia—not much evidence has been gathered related to PTSD. More studies are needed to improve the understanding of how neurocircuitry affects PTSD, say the researchers. (Progress in Neuro-psychopharmacology & Biological Psychiatry, Jan. 11, 2019)
|
Rates of wrong-site spinal surgery in VA
 Photo: ©iStock/Morsa Images (01/24/2019)
The VA National Center for Patient Safety investigated the rates of wrong-site spinal surgery in the Veterans Health Administration. Surgery on the wrong region of the spinal cord is one of the most commonly reported surgical mistakes. The researchers found 32 cases of wrong-site spinal surgery over an 18-year period in the VHA. This equates to an error in 2.66 of every 10,000 spinal surgeries, a rate comparable to that seen nationally outside VA. The most common cause was a problem with the X-ray, such as image quality. Error rates in spinal surgery were steady during the 18-year study period, even though error rates in other types of surgeries declined. New methods to optimize X-ray image quality and interpretation may be needed to correct this problem, say the researchers. (Clinical Spine Surgery, Jan. 11, 2019)
|
ADHD drug may help in Parkinson’s
 Photo: ©iStock/MarsBars (01/24/2019)
The medication atomoxetine shows potential for treating executive dysfunction caused by Parkinson’s disease, found a Durham VA Health Care System review. Atomoxetine (sold as Strattera) is commonly used to treat ADHD. Executive functioning refers to cognitive processes involved in planning, organizing, and completing tasks. Several studies showed that atomoxetine improves markers of executive dysfunction—such as impulsivity, risk-taking, and global cognition—in Parkinson’s patients. The drug was well-tolerated in most studies, with a few reports of gastrointestinal problems or insomnia. The results show that atomoxetine should continue to be explored to treat Parkinson’s disease, according to the researchers. (Journal of Clinical Psychopharmacology, December 2018)
|
Chronic kidney disease care varies widely in VA system
 Photo: ©iStock/Natali_Mis (01/16/2019)
Chronic kidney disease treatment in VA facilities varied widely and was often suboptimal, found a study including Michael E. DeBakey VA Medical Center researchers. The study looked at nearly 300,000 patients with both CKD and diabetes receiving care in 130 VA facilities. They found that rates of laboratory test ordering and nephrology referral scheduling varied widely. Only 13 percent of patients met all outcomes measuring recommended care for chronic kidney disease. The results show that further efforts are needed to standardize CKD care within VA, say the researchers. They did note in an interview with the health website Healio.com that “these rates are similar [to, if not better than those of] other health care systems.” (Clinical Journal of the American Society of Nephrology, Dec. 7, 2018)
|
Hybrid treatment proves effective for Veterans with PTSD and TBI
 Photo: ©iStock/Steve Debenport (01/16/2019)
A new hybrid treatment called SMART-CPT led to improvement in PTSD symptoms and cognitive functioning in patients with PTSD and traumatic brain injury, in a VA San Diego Healthcare System study. Researchers combined two treatments to create SMART-CPT. Cognitive Symptom Management and Rehabilitation Therapy (CogSMART) aims to improve memory and function through brain training—such as list memorization and problem-solving drills—after a brain injury. Cognitive processing therapy (CPT)—a widely used PTSD treatment—is talk therapy that helps patients change their thinking about traumatic events. In the study, Veterans with PTSD and TBI were given either CPT only or SMART-CPT. Patients in both groups had lower PTSD and postconcussive symptoms after treatment. Those in SMART-CPT also had additional improvements in attention/working memory, verbal learning/memory, and novel problem-solving. The results show that SMART-CPT can have benefits beyond CPT alone. (Journal of Neurology, Neurosurgery, and Psychiatry, Dec. 15, 2018)
|
Improving prediction of Alzheimer’s disease
 Illustration: ©iStock/tampatra (01/16/2019)
Changing the criteria for mild cognitive impairment diagnosis to include two separate memory tests allows for better prediction of future Alzheimer’s disease, according to a study including a VA San Diego Healthcare System researcher. The study looked at patients diagnosed with MCI by Alzheimer’s Disease Neuroimaging Initiative (ADNI) criteria who also took a second memory test, the Rey Auditory Verbal Learning Test (AVLT). Patients who showed MCI on both memory tests had consistently higher levels of biomarkers for Alzheimer’s disease, compared with patients diagnosed with MCI by the ADNI but not the AVLT, and cognitively normal patients. Catching Alzheimer’s early gives patients more time to prepare, and medications are more effective in early stages of the disease. Using a single MCI test often yields false positives or negatives, according to the researchers. They concluded that changing the requirement for MCI diagnosis to include two different memory tests could improve prediction of progression to Alzheimer’s disease. (Brain Imaging and Behavior, Dec. 4, 2018)
|
Racial disparities in electroconvulsive therapy
 Illustration: National Institute of Mental Health (01/14/2019)
Racial disparities exist in the use of electroconvulsive therapy to treat depression in older adults, found a study including a Houston VA health Care System researcher. ECT involves applying electrical current to the brain to treat mood disorders. It has proven effective in treating major depressive disorder when medication does not work. The researchers looked at nearly 700,000 patients older than 65 in a national health care database. They found that black and Hispanic patients were nearly half as likely to receive ECT, compared with white patients. While the research team acknowledges that patient preference may have played some role, they assert that efforts are needed in any case to ensure that minority groups have equal access to care. (American Journal of Geriatric Psychiatry, Nov. 29, 2018)
|
Barriers to medication treatment for opioid use disorder
 Photo: ©iStock/Charles Wollertz (01/14/2019)
VA Palo Alto Health Care System researchers explored the barriers to using medication to treat opioid use disorder within VA. Evidence shows that medications such as methadone, buprenorphine, and naltrexone care be effective at treating opioid use disorder. However, only 21 percent of patients with the disorder in VA residential treatment are on these medications. According to patient and staff surveys, barriers to this type of treatment include program philosophy against medication use, lack of coordination with other treatment settings, and perceived low patient interest. Having prescribers on staff, education and support for patients and staff, and support from leadership would help facilitate medication treatment, according to survey responses. (Journal of Studies on Alcohol and Drugs, November 2018)
|
Survey: Most Vets OK with curbing gun access during times of high suicide risk
 Photo: ©iStock/GummyBone (01/14/2019)
Veterans receiving mental health care were in favor of voluntary programs to reduce firearm access during high-risk periods for suicide, in a VA Ann Arbor Health Care System survey. Veterans in mental health care have high rates of firearm-related suicide. Of Veterans surveyed receiving mental health care at one VA facility, 93 percent were in favor of health system interventions to limit firearm access. Of those, 75 percent were in favor of substantially limiting firearm access during times of crisis. While Veterans with household firearms were less likely to be in favor of interventions, 50 percent of the group that owns firearms still said they would participate in an intervention to limit firearm access during high-risk periods. The results suggest that VA and other health systems should consider more intensive efforts to voluntarily limit firearm access during high-risk periods, say the researchers. (General Hospital Psychiatry, Nov.-Dec. 2018)
|
Risk factors for transition from suicidal thoughts to attempts
 Photo for illustrative purposes only. ©iStock/Geber86 (01/03/2019)
A team co-led by a VA San Diego Healthcare System researcher identified characteristics that differed between service members who contemplated suicide and those who went on to make a suicide attempt. As part of the Army STARRS study, researchers surveyed more than 10,000 soldiers. They found that, compared with soldiers without suicidal thoughts, those with suicidal thoughts had higher rates of interpersonal violence, relationship problems, major depressive disorder, PTSD, and substance use disorder. Soldiers with combat trauma in the past 12 months, intermittent explosive disorder, or any college education were less likely to have suicidal thoughts. Of those with suicidal thoughts in the past 30 days, those with PTSD had higher risk of suicide attempt. Those with intermittent explosive disorder or some college education were less likely to have attempted suicide. The results show that PTSD, intermittent explosive disorder, and education should be considered when studying what makes suicidal ideation transition into suicide attempts. (Depression and Anxiety, Dec. 14, 2018)
|
Carpal tunnel syndrome treatment varies widely in VA
 Photo: ©iStock/PeopleImages (01/03/2019)
Nonsurgical therapy use for carpal tunnel syndrome varies widely within the Veterans Health Administration, according to a study by VA Ann Arbor and Palo Alto researchers. Of nearly 80,000 patients diagnosed with carpal tunnel syndrome, 8 percent had surgery. Across different facilities, between 0 and 93 percent of surgical patients received physical therapy, occupational therapy, or an orthotic. Between 1 and 67 percent of nonsurgical patients received these types of therapy. Between 0 and 100 percent of surgical patients had electrodiagnostic studies (such as X-rays or CT scans), while between 0 and 55 percent of nonsurgical patients had diagnostic scans. The results suggest that clinical practice guidelines are needed to improve the uniformity and efficiency of carpal tunnel care, say the researchers. (Journal of Hand Surgery, Dec. 19, 2018)
|
Probing the evidence for probiotics
 Illustration: ©iStock/wildpixel (01/03/2019)
Evidence suggests that several probiotics are effective to treat various conditions, found a study by an Edward Hines, Jr. VA Hospital researcher and colleagues. Probiotics are live bacteria and yeast that promote a healthy microorganism balance in the digestive tract. While many probiotics are on the market, evidence is lacking on their effectiveness. Researchers reviewed the current medical literature and consulted experts in the field about which probiotics have been shown to be effective. They found enough evidence to suggest that 22 different types of probiotics are effective at treating different conditions. Some probiotics had strong evidence for treatment of conditions such as antibiotic-associated diarrhea, pediatric acute diarrhea, and inflammatory bowel disease. The researchers stress that it is important to pick the correct strain, formulation, and dose of a probiotic to match a specific disease. (PLoS One, Dec. 26, 2018)
|
Intimate relationships may buffer against suicide
 Photo for illustrative purposes only. ©iStock/ljubaphoto (12/26/2018)
Strong intimate relationships could help protect service members from suicide, according to a VA Ann Arbor Health Care System study. Researchers surveyed 712 National Guard members after they returned home from deployment. The found that lower relationship satisfaction and more depressive symptoms at six months after deployment were linked to greater risk of suicide 12 months after deployment. Couple satisfaction was related to suicide risk for service members with PTSD, depression, and anxiety. The results show that the strength of an intimate relationship could serve as a buffer against suicide for patients who have these conditions, say the researchers. (Suicide and Life-Threatening Behavior, Dec. 3, 2018)
|
Molecular brain damage after blast exposure
 Illustration ©iStock/kh_art (12/26/2018)
A team including researchers from the Bedford VA Medical Center in Massachusetts have shown molecular changes in brain cells that occur after a mild traumatic brain injury. The researchers used a mouse model to simulate exposure to low-intensity blasts, analogous to those experienced by many service members. They found changes in interactions within cells for more than 2,000 different proteins. The brain cells showed mitochondrial dysfunction, as well as other structural damage. This damage negatively affected cell growth, development, and other functions. Understanding what molecular changes occur after mild traumatic brain injury could help scientists better identify and treat brain injuries. (Journal of Neurotrauma, Nov. 28, 2018)
|
Adding fish oil to a statin did not lead to better cardiovascular health in Veteran study
 Photo: ©iStock/solidcolours (12/26/2018)
Adding fish oil to statin treatment did not improve cardiovascular outcomes in a Fargo VA Health Care System database study that included nearly 1,000 patients. Statins are the standard drugs prescribed for high cholesterol. Past research has shown that fish oil could help prevent major coronary events in patients with high cholesterol. The researchers looked at data for Veterans prescribed either a statin alone or statins and fish oil together. They did not find any difference between the group in number of cardiovascular events—such as heart attack or stroke—or in rates of any-cause death. The results suggest that adding fish oil to statin treatment does not lower the risk of cardiovascular problems. (Federal Practitioner, October 2018)
|
Lowering of blood pressure medication linked to fewer falls in long-term care
 Photo: iStock/Toa55 (12/20/2018)
Deintensification, or lowering, of blood pressure medication could lead to fewer falls in older adults in nursing homes, found a study by researchers from several VA facilities. Researchers looked at data on more than 2,000 VA nursing home residents whose records suggested evidence of overly aggressive blood pressure treatment. Eleven percent of patients had had their medication lowered prior to the study. Those whose medication levels were lowered had a significantly lower risk of recurrent falls than other patients. The results suggest that steps should be taken to deintensify overly aggressive treatment for high blood pressure, say the researchers. (Health Services Research, December 2018)
|
Lab study suggests heart benefits from widely used diabetes drug
 Photo: iStock/dra_schwartz (12/20/2018)
An international lab study that included a VA San Diego Healthcare System researcher showed that congenital heart disease (CHD) and obesity can lead to heart failure, but treatment with metformin, a widely used diabetes drug, can prevent the condition. CHD is the most frequent birth defect worldwide. Researchers found that the combination of CHD and a high-fat diet in mice led to heart failure. Giving mice the drug metformin prevented this heart dysfunction. Early treatment with metformin may prevent or delay the onset of heart failure in patients with CHD, say the researchers. (Molecular Metabolism, Nov. 15, 2018)
|
Prolonged exposure therapy, medication equally effective at treating PTSD in new study
 Photo: iStock/KatarzynaBialasiewicz (12/20/2018)
PTSD treatment with prolonged exposure therapy and with the anti-anxiety drug sertraline (sold as Zoloft) showed similar effectiveness, in a study including several VA researchers. Researchers treated 223 Veterans with PTSD with one of three treatments: prolonged exposure therapy plus a placebo, prolonged exposure therapy plus sertraline, or sertraline plus a medication management program. After 24 weeks, patients in all three groups had significantly decreased PTSD symptoms. No significant symptom differences existed between groups. Prolonged exposure therapy, a type of psychotherapy, is a preferred PTSD treatment within VA. The researchers expected that therapy and sertraline together would prove the most effective. The results suggest that adding medication to prolonged exposure therapy does not further improve PTSD symptoms, according to the researchers, although they say more study is necessary. (JAMA Psychiatry, Dec. 5, 2018)
|
Robotic heart procedure shown to be safe and effective
 Photo: ©iStock/3alexd (12/12/2018)
Robotic percutaneous coronary intervention is as safe and effective as manual PCI, found a study including VA San Diego Healthcare System researchers. In PCI, surgeons use a catheter to place a stent in blood vessels in the heart. Manual PCI procedures can expose the surgeon to radiation from the X-ray machine, as well as other occupational hazards. Using a robotic platform can protect surgeons from these hazards. To see how well robotic PCI works compared with manual procedures, researchers looked at outcomes from 108 robotic and 226 manual PCIs. They found no differences between the procedures in adverse cardiovascular events after six and 12 months. The results show that robotic PCI can be similarly effective to manual PCI while offering protection to the surgeons. (Catheterizations and Cardiovascular Interventions, Nov. 19, 2018)
|
Two DNA sites linked to PTSD risk
 Photo: ©iStock/Gio_tto (12/12/2018)
A team including a VA San Diego Healthcare System researcher identified two genome sites that may influence a person’s risk for PTSD. While trauma exposure often leads to PTSD, not everyone who experiences trauma develops PTSD. To explore why that is, researchers looked at the genomes of trauma-exposed people with and without PTSD. They found that those with PTSD had more methylation at two specific genome sites: NRG1 and NGS. Methylation is when a chemical compound (methyl) attaches to the DNA molecule. It can change how the DNA segment acts. Future research should focus on whether this DNA activity existed prior to trauma, making it a risk factor for PTSD, or whether PTSD causes the activity, say the researchers. (Epigenomics, Nov. 20, 2018)
|
Cisplatin superior to cetuximab for cancer treatment
 Illustration: ©iStock/Nerthuz (12/12/2018)
The drug cisplatin was superior to cetuximab in treating head and neck cancer along with radiation therapy, in a study by researchers from the Michael J Crescenz and James J. Peters VA medical centers. Both cisplatin and cetuximab are commonly given along with radiation therapy to treat head and neck squamous cell carcinoma. The researchers looked at 4,520 cancer patients over a period of three years. They found that those on cetuximab had significantly inferior overall survival, compared with patients taking cisplatin. The results suggest that cisplatin is the most appropriate drug partner for radiation therapy, say the researchers. (Cancer, Oct. 20, 2018)
|
Large genome study leads to better understanding of high blood pressure
 Photo by Jeff Bowen (12/04/2018)
A large international genetic study that included several VA researchers has identified more than 500 new gene locations that affect blood pressure. The project is the largest genetic study of blood pressure to date, involving more than 1 million participants. It included data from VA’s Million Veteran Program. By comparing participants’ genetic data, researchers identified 535 new locations on the human genome that influence blood pressure. The researchers calculate that the new findings increase the knowledge of inheritable blood pressure traits by 27 percent. They call the findings “an important step forward” in understanding how genes affect blood pressure. (Nature Genetics, October 2018)
|
Program improved staff interactions with residents
 Photo for illustrative purposes only. ©iStock/monkeybusinessimages (12/04/2018)
A training program improved interactions between staff and VA community living center residents, in a study by researchers at several VA facilities. The intervention centered on observations, huddles, and a focus on the positive. Researchers surveyed 62 residents and 308 staff members after the staff behavioral change program. Results showed increased communication and decreased negative staff intervention with residents after the training. Staff members credited the program with helping them to understand the importance of engagement and improving the quality of their interactions with residents. (Gerontologist, July 13, 2018)
|
White matter damage could explain chronic headaches after TBI
 Photo: ©iStock/wenht (12/04/2018)
Researchers with the VA San Diego Healthcare System have identified white matter abnormalities in the brains of patients with mild traumatic brain injury that may help explain their chronic headaches. The study used brain imaging data from 12 patients with TBI and chronic headache, compared with healthy controls. The TBI patients had abnormalities of the white matter in two brain tracts: the left superior longitudinal fasciculus, and the right anterior thalamic radiation. These tracts link different parts of the brain. This disruption of communication within the brain could be partly responsible for chronic headaches often experienced by patients with TBI, say the researchers. (Molecular Pain, Oct. 16, 2018)
|
Mouse study: Aspirin may slow multiple sclerosis
 Photo by Jerry Daliege (11/29/2018)
Low-dose aspirin could suppress multiple sclerosis symptoms and slow the disease, according to a mouse study by Jesse Brown VA Medical Center researchers. Mice with a condition similar to MS were given small doses of aspirin orally. Mice given aspirin show reduced symptoms for both relapsing-remitting and chronic forms of the disease. The aspirin also seems to have prevented destruction to the myelin sheath in the spinal cord caused by destructive T-cells. The researchers found that aspirin reversed the depletion of regulatory T-cells that occurs in MS, which may have helped stop other T-cells from attacking nerve fibers. While more study is needed, the results suggest that low-dose aspirin regimens could help patients with MS, say the researchers. (Science Signaling, Nov. 27, 2018)
|
Rural, urban ICUs perform similarly in VA system
 Photo: ©iStock/PeopleImages (11/29/2018)
Rural intensive care units (ICUs) in VA facilities perform similarly to their urban counterparts, found an Iowa City VA Health Care System study. Researchers looked at data on nearly 10,000 rural patients and almost 66,000 urban patients. They found that patients treated at rural ICUs had similar mortality rates, despite rural locations having lower-complexity facilities. Rural patients were less likely to have respiratory illnesses and more likely to have sepsis than urban patients, and they had higher illness severity scores. Rural patients also had fewer inter-hospital transfers and shorter ICU length of stay. The results indicate that being part of a national health care system may have benefits for rural facilities that should be explored outside the VA system, according to the researchers. (Journal of Critical Care, Oct. 19, 2018)
|
Study explains gene mutation’s link to ALS
 Photo: ©iStock/imaginima (11/29/2018)
Researchers at the VA Lexington Medical Center and University of Kentucky have shown how a gene mutation may contribute to the development of amyotrophic lateral sclerosis (ALS). Mutation to a gene called fused in sarcoma (FUS) are known to contribute to some cases of inherited ALS. The researchers showed that this mutation can suppress protein translation and interfere with how RNA functions in the body. The mutated proteins generated by the FUS gene disrupt an RNA quality-control pathway, which damages neuronal maintenance and function. Because this mutation suppresses how proteins are translated within cells and disrupts how RNA regulates cell activity, it likely contributes to the motor cell death seen in ALS. According to the researchers, the results will add to the understanding of both how this specific mutation can lead to inherited ALS, and more generally how ALS develops. (Proceedings of the National Academy of Sciences, Nov. 19, 2018)
|
Patients more likely to use psychotropic medication in suicide attempts when they have a prescription
 Photo: ©iStock/DNY59 (11/21/2018)
People at high risk for suicide who had a psychotropic medication prescription were more likely to use that type of drug in suicide attempts than those without a prescription, found a study including a Rocky Mountain Regional VA Medical Center researcher. The study looked at health insurance data for nearly 23,000 people who had attempted suicide. Those who had prescription access to a psychotropic drug were 1.7 times more likely to use that drug to attempt suicide than those without a prescription. People with antipsychotic or mood stabilizer prescriptions had the highest odds of using their prescription drug in a suicide attempt. Antianxiety drugs were the most common class of drugs used, regardless of prescription status, accounting for 59 percent of overdose attempts. The results show that people at risk for suicide with psychotropic prescriptions should be targeted for safety interventions, say the researchers. (Journal of Clinical Psychiatry, Nov. 6, 2018)
|
High cholesterol linked to lower risk of death in chronic kidney disease patients
 Photo: ©iStock/lbodvar (11/21/2018)
High cholesterol was linked to lower risk of death in chronic kidney disease patients, but higher risk of death in other patients, in a VA Long Beach Healthcare System study. Researchers looked at data on more than 2 million Veterans. They found that, in patients with chronic kidney disease, patients with cholesterol levels higher than 200 mg/dL had lower risk of all-cause death. However, patients without chronic kidney disease had a higher risk of death from cardiovascular conditions when their cholesterol was above 200 mg/dL. More research is needed to explore the seemingly paradoxical relationship between chronic kidney disease and cholesterol, according to the researchers. (American Heart Association Scientific Sessions, Nov. 10, 2018)
|
Reasons for trauma-focused therapy drop-out
 Photo: ©iStock/asiseeit (11/21/2018)
Minneapolis VA Healthcare System researchers explored why some Veterans with PTSD drop out of prolonged exposure and cognitive processing therapy, the two main forms of psychotherapy that VA uses to treat the condition. About one-third of Veterans who begin prolonged exposure and cognitive processing therapy do not complete treatment. Researchers interviewed 60 patients who completed treatment and 68 who did not to look for differences. They found differences between the groups in the strength of the working relationship between patient and therapist, patients’ ability to cope with increased distress, and internal motivation. Treatment buy-in, logistical factors such as transportation, and beliefs about treatment did not appear to influence the drop-out rate. (Annual Meeting of the International Society for Traumatic Stress Studies, Nov. 9, 2018)
|
Diabetes prevention program equally effective online and in person
 Photo: ©iStock/Wand_Prapan (11/14/2018)
Diabetes prevention programs delivered in person and online can be similarly effective for both older and younger Veterans, found a VA Ann Arbor Healthcare System study. Researchers looked at data from 378 Veterans enrolled in a weight management program either in-person or online. Over 70 percent of participants completed eight or more sessions within six months. A higher percentage of the online group completed at least eight sessions. Both online and in-person groups saw similar weight loss. Weight loss was the same for both younger participants and participants 65 or older. The results show that online programs may be an good way for diabetes prevention programs to reach older adults, say the researchers. (Diabetes Care, Oct. 30, 2018)
|
Benzodiazepine use linked to greater hospitalization, suicide risk in those with PTSD
 Photo: ©iStock/happyphoton (11/14/2018)
Patients with PTSD who were prescribed benzodiazepines, such as Valium or Xanax, had higher health care utilization and suicide risk than similar patients not given the drugs, in a study by VA Salt Lake City Health Care System researchers. They looked at data on more than 240,000 Veterans with PTSD. About 7 percent of those were prescribed benzodiazepines during the 14 years examined in the study. Patients prescribed benzodiazepines had more hospitalizations, as well as outpatient and mental health visits, than those not on the drug. Benzodiazepines users had a significantly greater risk of death from suicide, and were more likely to have suicide attempts or suicidal thoughts. The study strengthens the evidence against use of the drugs in Veterans with PTSD, according to the researchers. (Journal of Clinical Psychiatry, Oct. 23, 2018)
|
Household paints likely to contain rash-causing allergen
 Photo: ©iStock/gece33 (11/14/2018)
Household paints frequently contain isothiazolinones, despite claims on safety data sheets, according to a study featuring Minneapolis VA Medical Center researchers. Isothiazolinones are commonly used as preservatives in household products, but can cause allergic reactions. The researchers tested 47 common paints. All 47 contained at least one isothiazolinone. Concentration varied based on the type of isothiazolinone present. Isothiazolinones were present even in paint specifically advertised as being preservative-free. Safety data sheets, which are supposed to disclose potential allergens, were inaccurate and insufficient to warn against possible contact dermatitis, say the researchers. (Dermatitis, Oct. 20, 2018)
|
Omega-3 fatty acids boost neurological health after stroke in mice
 Photo: ©iStock/BlackJack3D (11/07/2018)
Omega-3 fatty acids were shown to improve neurological health after stroke, in a mouse study by VA Pittsburgh Health Care System researchers. The researchers gave mice food supplements of omega-3 polyunsaturated fatty acids, including from fish oil, for 35 days after a stroke. Mice given omega-3 had better cognitive function and neurovascular healing than those not on the supplements. Omega-3 was not as effective at improving cognitive function in older animals as in younger animals, although older animals did improve some. The results suggest that omega-3 fatty acid could be a promising therapy after stroke, say the researchers. (Neurobiology of Disease, Sept. 12, 2018)
|
Battlefield acupuncture effective in both groups and individually
 Photo by Robert Turtil (11/07/2018)
Battlefield acupuncture was effective in treating back pain in both group and individual settings, in a West Haven VA Medical Center study. In battlefield acupuncture, needles are placed in specific sites in the ear to influence the nervous system. The researchers treated 284 Veterans with back pain in either a group or individual setting, for a total of close to 800 treatment sessions. Patients self-reported a decrease in pain after 82 percent of treatments. Patients reported no change after 10 percent of treatments, and reported increased pain after 8 percent of the sessions. Both group and individual treatment had similar rates of effectiveness. The results confirm that battlefield acupuncture could be a useful treatment to relieve pain, whether administered in a group or individually. (Medical Acupuncture, Oct. 1, 2018)
|
Study reveals how lungs protect against damage from cigarette smoke
 ©iStock/bagi1998 (11/07/2018)
A study by VA Pittsburgh Healthcare System researchers explored mechanisms that protect the lungs from oxidants and how smoking can damage these processes. The researchers looked at two parts of the lungs’ defense system: an enzyme called GPx3 and a hormone receptor called PPAR-gamma. They found that GPx3 expression was decreased in the lungs of patients with chronic obstructive pulmonary disease (COPD). The study showed that PPAR-gamma responds to oxidative stress from cigarette smoke by increasing GPx3 production, which helps protect the lungs from damage. However, the researchers also found that cigarette smoke makes the relationship between GPx3 and PPAR-gamma less effective. They believe that the results could be useful in the development of more effective treatments for COPD. (Free Radical Biology and Medicine, October 2018)
|
Small molecule has potential as non-opioid pain drug
 Photo: ©iStock/kasto80 (11/02/2018)
A team featuring several VA researchers have discovered a non-narcotic drug that has potential to reduce neuropathic pain. The team designed and synthesized a small molecule that disrupts protein exchange in calcium channels in nerves. Calcium channels control the flow of molecules between nerve membranes, and have been shown to affect how pain is perceived. The channel targeted by the new molecule is important for the release of pain neurotransmitters in the spinal cord. When given to rodents, the molecule lowered their neuropathic pain response. This discovery has potential to be developed into a non-opioid pain medication, according to the researchers. (Proceedings of the National Academy of Sciences, Oct. 24, 2018)
|
Brain stimulation technique no better than sham version in depression study
 Brain illustration: ©iStock/cosmin4000 (11/02/2018)
In a trial sponsored by VA’s Cooperative Studies Program, Veterans receiving repetitive transcranial magnetic stimulation for major depression did not show greater signs of remission than those not undergoing the treatment. In TMS, an electromagnetic coil is placed on the head to stimulate a specific brain region. The researchers treated 164 Veterans with treatment-resistant major depression with either TMS or sham treatment. Of those receiving TMS, 41 percent saw remission of depressive symptoms. In the sham group, 37 percent saw remission. The difference was not statistically significant, say the researchers. The results do not support previous studies in civilians showing TMS to be effective for major depression. In fact, the FDA has approved TMS to treat depression that doesn’t respond to other treatments. The VA researchers believe the difference could be that Veterans often have multiple mental health conditions, making treatment more complex. They point to the fact that patients in the TMS group without PTSD were more likely that those with PTSD to achieve remission in the study. The researchers also note that the remission rate for both the TMS and sham groups was higher than seen in previous studies. They say this could be because Veterans had higher expectations of recovery and because their medications and other treatments were closely monitored. (JAMA Psychiatry, Sept. 1, 2018)
|
Study explores alcohol counseling for Vets in non-VA care
 Photo for illustrative purposes only. ©iStock/PeopleImages (11/02/2018)
Veterans were more likely than non-Veterans to be screened by doctors for heavy drinking, found a study by VA Pittsburgh and Puget Sound health care system researchers. While past research has shown that Veterans receiving care through VA have high rates of alcohol screening and intervention, less than 50 percent of Veterans in the U.S. use VA health care. The researchers looked at data on more than 92,000 people who had visited a non-VA doctor for a routine checkup within the last two years, 14 percent of whom were Veterans. The Veterans were more likely to be screened for alcohol quantity and heavy episodic drinking than non-Veterans. They were also more likely to receive advice about alcohol’s harmful effects. However, Veterans were not more likely to receive advice to reduce or abstain from drinking. The results point to some gaps in the delivery of recommended alcohol-related care, especially for vulnerable populations such as women Veterans, say the researchers. (Journal of Substance Abuse Treatment, Sept. 8, 2018)
|
Food environment can alter weight management effectiveness in men
 Photo for illustrative purposes only. ©iStock/gilaxia (10/25/2018)
The food environment in people’s neighborhoods slightly affects how effective VA’s MOVE! weight management program is, at least among men, found a study by VA Great Lakes Health Care System researchers and their colleagues. MOVE! is a VA program designed to help Veterans eat healthier, be more physically active, and achieve weight loss goals. Researchers studied data on MOVE! patients and community locations for a seven-year period. They found that the program was slightly less effective for men living near fast food restaurants or convenience stores. The food environment did not change the program’s effectiveness among women. The results highlight the importance of considering environmental and community factors in weight loss, say the researchers. (Health Services Research, Sept. 23, 2018)
|
More research needed on stem cell therapy for diabetic foot ulcers
 Photo: ©iStock/Hotaik Sung (10/25/2018)
Studies suggest that stem cell therapy could be an effective treatment for diabetic foot ulcers, but more research is needed on best techniques, according to a review by a team including a VA Connecticut Healthcare System researcher. Multiple studies have shown that stem cell therapy for diabetic foot ulcers is both safe and effective. However, studies varied widely on what stem cell type they used and how the treatment was delivered. Many different study designs were used, making it difficult to compare techniques. Because of these differences, the researchers emphasize the need for new studies to reach consensus on the best ways to test and deliver stem cell therapy for this condition. (Stem Cell Research & Therapy, July 11, 2018)
|
Studies teases out impact on kidneys of intensive blood pressure lowering
 Photo: ©iStock/Tashi-Delek (10/25/2018)
Two studies featuring several VA researchers found that intensive blood pressure lowering led to a decline in estimated glomerular filtration rate (eGFR), but not other signs of kidney damage. Doctors commonly use eGFR as a measure of kidney function. Previous research has suggested that intensive blood pressure control can lead to kidney injury. One study (ACCORD-BP) examined blood pressure risk in patients with diabetes. The other (SPRINT) looked at patients with high blood pressure who also had chronic kidney disease. Each study checked eGFR levels, as well as other biomarkers of kidney damage, in different groups of patients undergoing intensive blood pressure lowering treatment. Both found that intensive blood pressure lowering was linked with reductions in eGFR. However, neither study detected increases of biomarkers in the urine that usually indicate kidney damage. Both studies concluded that declines in eGFR may reflect hemodynamic changes—changes to blood flow—rather than actual kidney injury. (American Journal of Kidney Disease, Sept. 28, 2018)
|
PTSD not tied to asthma in Veteran study
 Photo for illustrative purposes only. ©iStock/Chalffy (10/17/2018)
PTSD was not linked to bronchodilator response, a marker of asthma, in a VA New Jersey Health Care System study. Past research has suggested that PTSD may be linked to symptoms of asthma in combat Veterans. To test this association, researchers looked at the breathing and PTSD symptoms of 188 Veterans of Iraq or Afghanistan. They found that responses to a bronchodilator—a drug that opens the airways, used to treat asthma—were not different between participants with and without PTSD symptoms. The researchers specifically looked at three symptoms of PTSD—re-experiencing, avoidance, and arousal—and did not find any link between any symptom and participants’ breathing. (Canadian Institute for Veteran and Military Health Research, Oct. 16, 2018)
|
The role of fatty acids in diabetic neuropathy
 Photo: ©iStock/JanIngeskogheim (10/17/2018)
Unsaturated fatty acids have potential for treating diabetic neuropathy, according to a review by a VA Iowa City Health Care System researcher. Diabetic neuropathy refers to nerve damage caused by diabetes. Multiple studies show that a diet high in saturated fat slows nerve function in rodents. Other studies with rodents suggest that unsaturated fats like omega-6 or omega-3 fatty acids could improve or even reverse vascular and neural problems. Studies show that resolvins, a type of unsaturated fatty acid, can promote neuron cell growth in diabetic mice. Omega-3 polyunsaturated fatty acids derived from fish oil have anti-inflammatory properties and could help with diabetic neuropathy, says the researcher. Clinical trials would be needed to test whether these substances would help people with diabetes. (Current Diabetes Reports, Aug. 25, 2018)
|
3D modeling of brain cells reveals protein changes linked to Alzheimer’s
 Photo: ©iStock/Henrik5000w (10/17/2018)
Researchers from the Edith Nourse Rogers Memorial Veterans Hospital in Bedford, Massachusetts, found protein alterations in neurons of Alzheimer’s disease patients by using a new technique. Studying neurons in a two-dimensional slide under a microscope, the usual way they are analyzed, does not give a full picture. The researchers created “neuro-spheroids,” 3D neuron cultures, using stem cells derived from patients’ blood cells. Using this technique, they found a number of alterations to proteins in the neurons of Alzheimer’s patients that would lead to dysfunction. When compared with postmortem brain tissue taken from Alzheimer’s patients, the 3D neurons showed similar dysfunction. The results show this type of 3D modeling could help find Alzheimer’s disease markers. The identified proteins could have important implications for the progression of the disease, say the researchers. (Journal of Proteomics, June 30, 2018)
|
Nursing home quality of care linked to cost
 Photo: ©iStock/LPETTET (10/10/2018)
Higher quality of nursing home care was linked to higher cost, in a study of 132 VA community living centers. Researchers looked at data from two years for all community living centers in the VA system. They measured quality of care by looking at rates of adverse health events (such as falls). Fewer adverse events were linked to higher predicted cost, suggesting that greater resources allocated to quality lead to better care. However, higher costs were not driven by higher nurse staffing levels. According to the researchers, more studies are needed to determine what precisely drives the relationship between quality and cost. (PLoS One, Sept. 19, 2018)
|
Evidence lacking on outcomes of genetic testing for statin resistance
 Photo: ©iStock/jxfzsy (10/10/2018)
Information is lacking on patient outcomes for statin-associated muscle symptoms (SAMS) after testing for the SLCO1B1 gene, according to a VA Boston Healthcare System literature review. SAMS refers to muscle pain and weakness sometimes caused by statin medication used to treat cardiovascular disease. Previous studies have shown that people with the SLCO1B1 gene are more likely to get SAMS. The researchers looked at 37 studies for evidence that testing for SLCO1B1 could lead to treatment changes and improved cholesterol levels in statin-intolerant patients. They found very few reports of patient outcomes after SLCO1B1 testing. More studies are needed to explore whether this type of genomic testing can lead to improvements in care, say the researchers. (Clinical Pharmacology and Therapeutics, Aug. 23, 2018)
|
Study suggests adverse health impact on sexual minorities from religious freedom law
 Photo: ©iStock/JacobStudio (10/10/2018)
A team including a VA researcher found that “unhealthy days” increased for Indiana residents identifying as sexual minorities after that state passed a religious freedom restoration act (RFRA). Statewide religious freedom restoration laws aim to protect the free exercise of religion by ensuring that any government interference must be for “compelling” interests, and must employ the “least restrictive means” possible. Some legal scholars have argued that RFRAs could potentially expose sexual minorities to more discrimination. And past research has shown that stigma and discrimination could worsen physical and mental health for sexual minority individuals. The researchers surveyed sexual-minority individuals in 21 states with RFRAs in 2015. They found the number of people reporting more than 14 “unhealthy days” per month increased quarterly in Indiana following the passing of an RFRA there. Unhealthy days did not increase for heterosexual people. This trend did not occur in other states. Indiana was the only state to pass and enact an RFRA in the time frame of the study. Other states already had RFRAs in place or had passed an RFRA but not put it into practice. Indiana also differed from other states in that its law applies to cases between private parties, not just those involving government. (American Journal of Orthopsychiatry, Sept. 24, 2018)
|
Telehealth a viable way to improve antimicrobial stewardship
 Photo: ©iStock/vm (10/04/2018)
A pilot telehealth program shows promise in improving infectious disease control at rural medical centers, according to a Louis Stokes Cleveland VA Medical Center study. Staff at two rural VA medical centers used videoconferencing to work with infectious disease physicians at other facilities. These videoconference antimicrobial stewardship teams (VASTs) held weekly meetings to discuss ways to combat antimicrobial resistance on a patient-by-patient basis. After a year of the program, one site accepted VAST recommendations in 73 percent of cases presented, and the other accepted 65 percent of the recommendations. Participants felt that the sessions improved their antimicrobial stewardship efforts and patient care. (Infection Control and Hospital Epidemiology, Sept. 6, 2018)
|
Mental health disorders linked with more unintended pregnancy
 Photo: ©iStock/Vasyl Dolmatov (10/04/2018)
Women Veterans with mental health disorders are more likely to have experienced unintended pregnancy than those without, found a study by VA Pittsburgh Health Care System researchers and colleagues. They surveyed almost 3,000 women Veterans by phone. Sixty percent of women with at least one mental health disorder reported having an unintended pregnancy, while 51 percent of women without a mental health disorder said they had had an unintended pregnancy. Mental health disorders were linked to a greater number of unintended pregnancies. Multiple mental health disorders were also connected to a greater number of unintended pregnancies. More research is needed on how to improve reproductive health outcomes for women with mental health disorders, say the researchers. (Journal of General Internal Medicine, Sept. 5, 2018)
|
Opioids not linked to better sleep for chronic pain patients
 Photo for illustrative purposes only. ©iStock fergusowen (10/04/2018)
Opioid use did not improve insomnia or fatigue for patients with chronic pain, in a Minneapolis VA Health Care System study. Insomnia is a common problem related to chronic pain. Researchers studied data on medication dosage and sleep disturbance for patients taking opioids or non-opioid medication for chronic pain. Over a year of treatment, neither group showed improvements in insomnia or fatigue despite improvements in pain severity. Medication dosage increased over the course of the trial. Patients with chronic pain commonly take extra opioid medication to sleep, but this increase did not lead to improved sleep. The results suggest that patients should be encouraged to used evidence-based behavioral sleep interventions to manage their insomnia, according to the researchers. (International Association for the Study of Pain, Sept. 13, 2018)
|
Early nonadherence to diabetes drugs leads to more heart attacks and strokes
 Photo: ©iStock/Wavebreakmedia (09/27/2018)
Patients who did not adhere early on to their medication treatment for type 2 diabetes were more likely to have poor health outcomes, found a study by VA Mid South Health Care Network researchers and their colleagues. Researchers looked at data for more than 159,000 Veterans with type 2 diabetes over an 11-year period. They measured patients’ adherence to oral diabetes medication by how often patients filled prescriptions in the first year of treatment. Patients who did not take their medication as prescribed were 14 percent more likely to have a heart attack in the five years after starting treatment, compared with those who took their medication. Those not regularly taking their medication were 22 percent more likely to have a stroke. The less compliant patients were to their medication regimen, the higher their chances were of having a heart attack or stroke. Those not adhering to treatment were also more likely to have died. The results underscore the need to help patients understand the importance of taking their oral antidiabetes medication regularly, say the researchers. (Diabetes Medicine, July 6, 2018)
|
Blood test could predict effectiveness of NSAID treatment in Alzheimer’s patients
 Photo by Derrick Morin (09/27/2018)
Blood tests could identify which Alzheimer’s disease patients will respond to non-steroid anti-inflammatory drug (NSAID) therapy, according to a study including a VA San Diego Healthcare System study. Previous research has shown the potential of NSAIDs to improve outcomes in Alzheimer’s patients because the disease has been linked to inflammation. An earlier study treated Alzheimer’s patients with two NSAIDs, rofecoxib and naproxen. In it, some patients improved and some declined in both groups as well as in controls. For the new study, researchers tested blood samples from these patients for four specific proteins that have been identified as inflammation biomarkers. They found that they could identify which patients in the rofecoxib group had cognitive improvements with 98 percent accuracy. They also predicted improvements in the naproxen group with 97 percent accuracy. The results show that a precision-medicine approach could identify which treatments will be most effective for specific patients with Alzheimer’s, according to the researchers. (Journal of Alzheimer’s Disease, Sept. 4, 2018)
|
Benzodiazepine prescribing higher than evidence warrants in older adults
 Photo for illustrative purposes only. ©iStock/BraunS (09/27/2018)
Prescribing of benzodiazepines may be higher than appropriate in older adults, according to a study that included several VA researchers. The team looked at use of the drugs across various health systems, not just in VA. Benzodiazepines are sedative drugs commonly prescribed for conditions such as insomnia, anxiety disorders, and behavioral and psychological symptoms of dementia. However, evidence suggest that these drugs could be dangerous for elderly patients. The researchers looked at 31 studies on the effects of benzodiazepines in patients over age 50 with the above three conditions. They found 21 studies that demonstrated improved insomnia outcomes. Only one study showed a benefit of the drugs for patients with anxiety disorder. They also found only a single study that showed improvements in behavioral disturbances in patients with dementia. The results suggest that benzodiazepine prescribing in older adults is higher than what is supported by evidence, according to the researchers. Studies are needed on how to reduce use of this type of drug in older patients, they say. (Harvard Review of Psychiatry, Sept/Oct 2018)
|
Brain peptide implicated in migraine pain
 Photo for illustrative purposes only. ©iStock/laflor (09/20/2018)
VA and University of Iowa researchers may have identified one of the sources of migraine pain. Researchers injected mice with calcitonin gene-relate peptide (CGRP), a substance naturally found in the brain that is believed to be related to nerve hypersensitivity and photosensitivity in migraine. They found that CGRP caused spontaneous pain in the mice, regardless of whether they were in light or darkness. When the researchers gave the mice an antibody that blocks CGRP receptors, the pain went away. They also found that the nonsteroidal anti-inflammatory drug meloxicam did not block the effects of CGRP. The antimigraine drug sumatriptan partially blocked CGRP response in male mice, but not females. (Pain, Sept. 1, 2018)
|
Suicide risk common in patients with anxiety
 Photo for illustrative purposes only. ©iStock/PeopleImages (09/20/2018)
A high number of patients with anxiety could be at risk for suicide, found a Syracuse VA Medical Center study. Researchers surveyed 182 primary care patients who had anxiety symptoms but were not in psychotherapy specialty care. Forty percent had elevated suicide risk, based on a standard assessment. Suicide risk was more common in patients who also had depression (51 percent) than in those who had anxiety alone (27 percent). The severity of anxiety symptoms did not affect patients’ suicide risk. The results suggest that primary care providers should assess suicide risk in patients with anxiety, even when patients are not seeking mental health treatment or when their anxiety symptoms do not rise to the level of an anxiety disorder, say the researchers. (Family Practice, Sept. 14, 2018)
|
Oxytocin fails to boost social cognition in schizophrenia trial
 Illustration: ©iStock/goa_novi (09/20/2018)
Oxytocin did not improve social cognition in patients with schizophrenia, in a study by VA San Diego Healthcare System researchers and their colleagues. Social cognition refers to how a person deals with other people, including aspects like social knowledge and emotional processing. People with schizophrenia often have impaired social cognition. The researchers prescribed schizophrenic patients oxytocin—a drug that has been shown to improve social cognition in the general population—over 24 weeks, along with cognitive-behavioral training. Patients taking oxytocin showed no improvements in social cognition over the course of the study, compared with patients taking placebo. The results add to growing literature suggesting that oxytocin may not be effective in this population. (Psychological Medicine, Sept. 6, 2018)
|
Herbicide-related COPD rates differ between self-report and lung tests
 U.S. Army, via Wikimedia Commons (09/14/2018)
Herbicide exposure during the Vietnam War was linked to self-reported chronic obstructive pulmonary disease (COPD), but the link was not supported by lung tests, in a study by VA's Office of Patient Care Services. Researchers surveyed more than 3,000 Veterans of the U.S. Army Chemical Corps who served in Vietnam. Those who had actively sprayed herbicides during their service were nearly twice as likely to say they had been told by a doctor that they had COPD, compared with non-sprayers. However, when the survey respondents were examined with spirometry—a common test of lung function—people in the spraying group were not more likely to have COPD than the non-spraying group. The difference may be due to physicians diagnosing COPD based on symptoms rather than spirometry, according to the researchers. Spirometry is underutilized by physicians, they say. (American Journal of Industrial Medicine, Aug. 29, 2018)
|
PTSD may disrupt parasympathetic nervous system during sleep
 ©iStock/domoyega (09/14/2018)
Patients with PTSD had blunted parasympathetic nervous system modulation during sleep, found a Durham VA Health Care System study. The parasympathetic nervous system is the part of the nervous system that regulates rest and digestion. Heart-rate variability can be used to assess how well the parasympathetic system is working. Researchers studied the sleep of 62 post-9/11 Veterans and service members. They found that, for those with PTSD, high-frequency heart rate variability was lower during the non-rapid eye movement sleep phase, compared with those without PTSD. Impaired parasympathetic nervous system function increases the risk of cardiovascular events. This parasympathetic modulation could be one reason for the increased rates of cardiovascular disease among Veterans with PTSD, suggest the researchers.
Patients with PTSD had blunted parasympathetic nervous system modulation during sleep, found a Durham VA Health Care System study. The parasympathetic nervous system is the part of the nervous system that regulates rest and digestion. Heart-rate variability can be used to assess how well the parasympathetic system is working. Researchers studied the sleep of 62 post-9/11 Veterans and service members. They found that, for those with PTSD, high-frequency heart rate variability was lower during the non-rapid eye movement sleep phase, compared with those without PTSD. Impaired parasympathetic nervous system function increases the risk of cardiovascular events. This parasympathetic modulation could be one reason for the increased rates of cardiovascular disease among Veterans with PTSD, suggest the researchers. (Sleep, Aug. 29, 2018)
|
Development of a new non-addictive pain drug
 ©iStock/SeventyFour (09/14/2018)
A team including a researcher from the W.G. Hefner VA Medical Center in Salisbury, North Carolina, is working on a pain medication that could potentially work as well as opioids without being addictive. They developed a new compound, AT-121, that works on the mu opioid receptor, a protein that opioids interact with to block pain. AT-121 also activates the nociceptin receptor, which blocks the addictive side effects of opioids. Using non-human primates, the researchers showed that AT-121 gave the same level of pain relief as opioids without the risk of addiction that comes with opioids. The results suggest that this new drug could have potential to both safely and effectively relieve pain, and also treat prescription opioid abuse. More studies will be needed before AT-121 can be tested in humans. (Science Translational Medicine, Aug. 29, 2018)
|
Circadian rhythm disruption linked to cognitive decline in older men
 ©iStock/MladenZivkovic (09/14/2018)
Disruptions in circadian rhythm are linked to greater cognitive decline in older men, according to a study including a Minneapolis VA Health Care System researcher. Circadian rhythm refers to the body's natural sleeping and waking patterns. Over multiple follow-up visits during an average period of three years, the researchers found that men with disrupted rest-activity circadian rhythm had greater cognitive decline, as measured by a standard cognition test, compared with those without disrupted circadian rhythms. Rest-activity circadian rhythm was measured using an accelerometer that recorded any time a patient's wrist moved. Aging is often associated with altered rest-activity circadian rhythm. The results add to growing evidence that age-related disruptions to sleep pattern are connected to cognitive decline, say the researchers. (Journal of the American Geriatric Society, Aug. 23, 2018)
|
Complex relationship between alcohol consumption and psychiatric distress
 Photo for illustrative purposes only. ©iStock/South_agency (09/06/2018)
Hazardous drinking was linked to higher likelihood of psychiatric symptoms, while results of moderate drinking were mixed, in a study by Durham VA Health Care System researchers and colleagues. Previous studies have linked heavy drinking with increased depression and anxiety, but the it is not clear what cause-and-effect relationships, if any, may exist. The researchers collected data on alcohol use and psychiatric conditions for 3,003 Veterans. They found that hazardous drinkers were more likely to have PTSD, depression, and suicidality, compared with moderate drinkers. For men, moderate drinkers were less likely than nondrinkers to have depression and suicidality. However, this relationship disappeared when nondrinkers with past alcohol use disorder were removed from the calculations. Women moderate drinkers had lower rates of PTSD than nondrinkers and light drinkers, even when those with past AUD were removed. More research is needed on the possible protective effects of moderate drinking, say the researchers. Also, patients with a history of AUD may benefit from mental health screening and treatment, they say. (Journal of Studies on Alcohol and Drugs, July 2018)
|
Written exposure therapy effective as PTSD treatment
 Photo: ©iStock/PeopleImages (09/06/2018)
Written exposure therapy (WET) could be as effective as cognitive processing therapy in treating PTSD, according to a VA Boston Healthcare System study. WET involves five weekly sessions in which patients write for 30 minutes in detail about a single traumatic event associated with their PTSD. Cognitive processing therapy (CPT), a common PTSD treatment, involves learning how to evaluate and change upsetting thoughts. WET is shorter than CPT, which usually lasts for 12 sessions and includes homework between each session. Patients in both a WET and CPT group showed similar improvement of PTSD symptoms when assessed 60 weeks later. Both treatments significantly reduced depressive symptoms, although the CPT group did have a more rapid decrease in symptoms. WET takes a similar approach to prolonged exposure therapy, another common psychological PTSD treatment, in that both focus on directly confronting memories of trauma. Prolonged exposure is usually based on talking with a therapist, and generally involves more sessions than WET. The results show that WET could be a short and long-lasting treatment for PTSD. (Depression and Anxiety, Aug. 24, 2018)
|
Study shows two genes may be linked to suicide attempts
 Photo: ©iStock/vchal (09/06/2018)
Durham VA Medical Center researchers have identified two genes that may be related to suicidal behavior. They conducted a genome-wide association study, in which they compared the genomes of a large number of Veterans to look for variations common among those with history of suicidal behavior. The researchers found an association between a gene called KCNMB2 and suicide attempts. This gene plays a key role in neuronal excitability. They also found evidence that may link another gene, ABI3BP, to both suicide attempts and suicidal thoughts. While the results are interesting, the researchers caution that they are preliminary and need replication in further studies. (Psychiatry Research, July 17, 2018)
|
Group treatment program curbs intimate partner violence
 Photo: ©iStock/RomoloTavani (08/29/2018)
The Strength at Home program can successfully reduce intimate partner violence use, found a study by Central Texas and Boston VA health care system researchers. SAH is a 12-week cognitive-behavioral and trauma-informed group treatment designed to reduce and end IPV use among military and Veteran populations. The pilot program is part of a national program within VA to help Veterans who use or experience IPV. It was implemented at 10 VA medical centers over a year. Seventy percent of sites successfully launched the program in the first year. Results from 51 Veterans who participated in the program showed a significant reduction in the number who exhibited violence toward a partner. The participants also showed reduced PTSD symptoms. While the pilot program showed overall successful implementation, more work is needed to reduce the time between initial training and the start of group treatment, according to the researchers. (BMC Health Services Research, July 24, 2018)
|
Repeated ketamine infusions may ease PTSD and depression
 Photo: ©iStock/stevecoleimages (08/29/2018)
Repeated ketamine infusions may improve PTSD and depression symptoms, according to a Minneapolis VA Health Care System study. Researchers gave 15 people with both PTSD and major depressive disorder six intravenous infusions of ketamine—a medication used mainly for anesthesia—over two weeks. Eighty percent had remission of PTSD symptoms immediately after treatment. The remission lasted a median of 41 days. For major depressive disorder, 93 percent experienced remission of symptoms, which lasted a median of 20 days. The results suggest that repeated ketamine treatments are safe and may be an effective treatment for people with both PTSD and major depressive disorder, say the researchers. (Journal of Clinical Psychiatry, May/June 2018)
|
Review study: Mind-body treatments show promise for PTSD
 Photo for illustrative purposes only. ©iStock/jacoblund (08/29/2018)
Studies show that mind-body treatments are promising for treating PTSD, found a literature review by VA Boston Healthcare System researchers. The researchers looked at 22 randomized controlled trials on mind-body techniques. Nine mindfulness and six yoga studies showed significant improvements in PTSD symptoms, compared with control groups. Seven studies showed large symptom improvements from relaxation interventions, even though relaxation was used as the control condition in these studies. While many studies on mind-body interventions have methodology weaknesses, the researchers found increased scientific rigor in recent studies. The results overall show increasing evidence on the benefits of mindfulness, yoga, and relaxation for PTSD. (Journal of Clinical Psychology, May 10, 2018)
|
Depression drives nursing home placement in older women
 Photo for illustrative purposes only. ©iStock/KatarzynaBialasiewicz (08/23/2018)
More severe depression symptoms led to higher rates of nursing home placement in women, found a study by San Francisco and Minneapolis VA health care systems. Researchers looked at data for more than 9,000 older women over a 20-year period. They found that women with low or moderate depressive symptom burden were twice as likely to move from community living to a nursing home, compared with women with minimal burden. Those with high burden were three times as likely. Antidepressant use only slightly affected this relationship. The results show the importance of improving recognition, monitoring, and treatment of depression early to reduce or delay nursing home placement, say the researchers. (Journal of the American Geriatric Society, Aug. 9, 2018)
|
Postconcussive symptoms predict opioid prescriptions
 Photo: ©iStock/VladimirSorokin (08/23/2018)
Traumatic brain injury symptoms predicted opioid prescriptions for chronic pain for Veterans, in a San Francisco VA Health Care System study. Opioids are not recommended for patients with neuropsychological impairment from traumatic brain injury. However, clinical guidelines are not always adhered to in actual practice. Researchers studied the records of 53,124 Iraq and Afghanistan Veterans with chronic pain diagnoses from VA providers during a nine-year period. Self-reported severe and very severe postconcussive symptoms predicted starting long-term or short-term opioid use for chronic pain. The results indicate a need to educate prescribers and make non-opioid pain management options more available for Veterans, according to the researchers. (Brain Injury, July 9, 2018)
|
Mild ozone exposure can cause breathing problems
 Photo for illustrative purposes only. ©iStock/Wavebreakmedia (08/23/2018)
Low-level ozone exposure causes breathing problems and lung damage in older people, according to a study led by a San Francisco VA Medical Center researcher. Ozone, a gas commonly found in the upper atmosphere, is considered a pollutant when present in lower levels of the atmosphere. Researchers exposed healthy adults to low concentrations of ozone for three hours, with intermittent exercise. Tests showed worse lung function after exposure to ozone, with higher ozone concentration linked to worse function. This decreased lung function was still noticeable 22 hours later. The results show that ozone can decrease lung function and cause airway injury and inflammation in older adults. The U.S. Environmental Protection Agency suggests regularly checking air-quality reports for levels of ozone and other irritants, especially for people with conditions such as asthma. (American Journal of Respiratory and Critical Care Medicine, May 15, 2018)
|
New approach to target drug treatment to painful joints
 Photo: ©iStock/solidcolours (08/15/2018)
Baltimore VA Medical Center researchers have designed a method that could more effectively deliver drugs directly to the joints to treat rheumatoid arthritis. Arthritis medications can cause damage to other organs because they affect the whole body rather than just the joints. Researchers used a liposome (a sphere of molecules surrounding another material, such as a medication) containing the peptide ART-1 to target medication to joint cells. A peptide is a chain of amino acids. ART-1 has been shown to bind to the endothelial cells in joints. Researchers injected this compound into rats with arthritis. They found that the injection containing ART-1 suppressed the disease better than a control that did not have ART-1. The ART-1 liposome also appeared to be safer than liposomes not directed by the peptide, which interacted with more parts of the body than the joints. The results show that ART-1 could be used to home in on the joints to treat rheumatoid arthritis. (Journal of Controlled Release, Aug. 4, 2018)
|
Patient perspectives on opioids
 Photo for illustrative purposes only. ©iStock/ClarkandCompany (08/15/2018)
Iowa City VA Healthcare System researchers interviewed 19 hospitalized Veterans about their chronic pain to get their perspective on opioids and other care. Patients were not asked about opioids specifically. Most patients brought up opioids themselves. Interviewees expressed views that other patients were the problem, meaning they thought opioid access was limited because other people were misusing opioids. They had empathy for providers, whom they saw as working under prescribing constraints. Most also viewed opioids as a last resort for treating pain. The results show that engaging hospitalized patients in conversations about opioids and alternative pain management would be useful, and that providers would benefit from increased awareness of chronic pain, say the researchers. (Pain Medicine, July 17, 2018)
|
Sailing therapy helpful in substance use disorders
 Photo: ©iStock/LeoPatrizi (08/15/2018)
Sailing adventure therapy may be a positive and calming activity for Veterans with substance use disorder, according to a George E. Wahlen VA Medical Center study. Twenty-two Veterans participated in the pilot study. In the therapy, participants sailed on a reservoir with an instructor for three hours, including instructional time. Each participant went to three sessions, once per month. They manned various positions on the sail boat, helped rig the sails, and watched out for other boats. After each trip, they took turns describing what the experience had been like for them personally and were encouraged to share whether they had learned anything about themselves from the experience. The activity did not increase anxiety or negatively affect the participants. Results show that this therapy may increase psychological flexibility and enhance treatment response, based on questionnaires given after the therapy. The results suggest that sailing adventure therapy could be a low-risk intervention for Veterans with substance use disorder, according to the researchers. (Complementary Therapies in Medicine, October 2018)
|
Urine biomarkers may warn of kidney damage from ventilation
 Photo: ©iStock/Natali_Mis (08/08/2018)
Novel urine biomarkers could give an early warning on kidney injury caused by mechanical ventilation, say VA San Diego Health Care System and University of California San Diego researchers. Previous research has linked mechanical ventilation to acute kidney injury. This link may be due to damage to the lungs and circulatory system, or blood flow changes to the kidney. Low-tidal volume—when less air is taken into the lungs with each breath—could help prevent this kidney injury. Several biomarkers (such as mitochondrial byproducts) have recently been found to show kidney dysfunction before permanent injury. By testing for these biomarkers in the urine, clinicians may be able to time when ventilation needs to be adjusted to prevent kidney injury, according to the researchers. (Nephron, July 11, 2018)
|
Battlefield acupuncture may reduce opioid use after surgery
 Photo by Robert Turtil, for illustrative purposes only. (08/08/2018)
Battlefield acupuncture may reduce the need for opioid use after surgery, found a John D. Dingell VA Medical Center study. In battlefield acupuncture, needles are placed in and around the ear to influence how the central nervous system processes pain. In a study of 39 patients, those who had this treatment after general surgery had significantly lower opioid use in the following 24 hours, compared to those not given acupuncture. Patients in the acupuncture group also had 15 percent less post-operative nausea and vomiting. Previous studies have shown that this type of acupuncture can reduce the stress response after surgery, aiding in recovery. The results suggest that battlefield acupuncture could be a low-cost, effective, safe, and easy to implement means of reducing post-operative pain, say the researchers. (2018 World Congress on Regional Anesthesia & Pain Medicine, April 19, 2018)
|
Health care performance measures may not be accurate for older patients
 Photo for illustrative purposes only. ©iStock/FatCamera (08/08/2018)
Standard measures of health care quality may not accurately rate care for higher risk patients, according to a VA Greater Los Angeles Healthcare System study. Measures based on processes of care—such as breast cancer screenings—are frequently used to compare health care performance. To see whether these measures are biased against older and sicker patients, researchers looked at national data on mortality risk from a 14-year period. They found that providers serving high-risk patients rated significantly worse (67 percent performance score) than for low-risk patients (74 percent). Clinicians may choose not to use recommended processes based on limited prognosis, patient preference, or potential adverse effects when patients are older and have more illnesses. The resulting poor performance scores may lead to financial penalties or excessive administrative work. The results suggest that process of care ratings may not be the best fit to evaluate all situations. (Journal of the American Geriatric Society, Aug. 6, 2018)
|
Lab study suggests novel RNA treatment could improve brain function after TBI
 Photo: ©iStock/Ivcandy (08/01/2018)
James A. Haley Veterans Hospital and University of South Florida researchers showed that injections of a type of RNA could improve brain function after a traumatic brain injury, in rats. The researchers injected injured rats with cell structures called exosomes, which they got from stem cells in human fat tissue. The exosomes contain MALAT1, a type of RNA (a form of genetic material). The rats injected with exosomes showed significant recovery of function of motor behavior, as well as a reduction in cortical brain injury. Analysis of the brain and spleen showed that MALAT1 could ease brain inflammation at a genomic level. The spleen is involved in protective substances such as white blood cells entering the blood stream after injury. The results show that using exosomes containing MALAT1 has "tremendous" potential for treatment of TBI, say the researchers. (Journal of Neuroinflammation, July 12, 2018)
|
Algorithm can identify urine-test results showing cannabis use
 Photo: ©iStock/courtneyk (08/01/2018)
VA Portland Health Care System researchers have developed an algorithm to identify cannabis urine drug test results in electronic health records. Although VA does not prescribe cannabis, in accordance with federal law, many states now allow medical cannabis use. Many patients are now using medical cannabis, particularly for chronic pain. While it may be important for doctors to know of this use, how the results of drug tests are reported varies widely. The researchers created a computer algorithm to identify the results of urine tests within the VA electronic health records. They tested the algorithm on a sample of VA patients who were prescribed long-term opioid therapy for chronic pain. The algorithm correctly identified cannabis-positive results for 99 percent of patients who used cannabis. It identified cannabis-negative results with 100 percent accuracy. The findings suggest that this algorithm is an effective way to identify urine test results for cannabis use within the electronic health record, despite inconsistent reporting practices. (Journal of Medical Systems, July 24, 2018)
|
VA emergency departments vary widely in opioid prescribing
 Photo: ©iStock/dusanpetkovic (08/01/2018)
Opioid prescribing rates vary widely in VA emergency departments (EDs), found a study by the VA Pharmacy Benefits Management program. The researchers looked at data on opioid prescribing for pain in 118 VA EDs between January and March 2017. The percentage of patients prescribed an opioid ranged from 1 percent to 24 percent, depending on facility. For individual clinicians, opioid prescribing rate varied between 0.2 percent and 57 percent. While nationwide interventions to promote safe opioid prescribing have resulted in lower overall opioid prescriptions in VA since 2011, much variation still remains based on geographic area and individual behavior. Targeting interventions for providers may be more effective than general prescribing guidelines at changing how opioids are prescribed in VA EDs, say the researchers. (Journal of General Internal Medicine, July 23, 2018)
|
Availability of non-VA health care lacking for rural Veterans, despite Veterans Choice Act
 Photo: ©iStock/davidperks (07/27/2018)
The Veterans Choice Act may not significantly improve rural Veterans' access to health care due to a shortage of non-VA providers, according to an Iowa City VA Medical Center study. Under the Veterans Choice Act, VA will pay for medical care from non-VA providers for Veterans who live more than 40 miles from a VA facility. Pending legislation is set to expand on the Veterans Choice Act and replace it. To see how the existing act or future versions could affect Veterans' access to care, researchers looked at data on both where rural Veterans live and what health care is available in those areas. They found that 16 percent of rural Veterans live in an area with primary care shortages, and 70 percent in mental health care shortage areas. Most rural Veterans lived in counties that lacked specialized care such as cardiologists and neurologists. In fact, VA played a greater role in delivering health care in areas where Veterans were eligible for the Veterans Choice Act, compared with less rural areas. The results show that programs such as telehealth are needed to supplement non-VA health care in rural areas, which may be lacking, say the researchers. (BMC Health Care Services, May 29, 2018)
|
Mouse study questions whether tau protein leads to brain degeneration after TBI
 Photo: ©iStock/D-Keine (07/27/2018)
A mouse study suggests that the build-up of a protein in the brain is not a cause of traumatic encephalopathy following a traumatic brain injury, counter to evidence from previous studies. James A. Haley Veterans Hospital researchers and their colleagues studied the build-up of tau proteins in the brain matter of mice after traumatic brain injury. Other research has documented increased tau protein in patients with chronic traumatic encephalopathy, a degenerative brain disease linked to dementia. Researchers on the new study found modest increases in tau protein in the brain after both a single and repetitive mild TBI. However, in both cases the protein was reabsorbed by the brain within 12 months after injury, with no evidence of excess build-up. Moreover, increased tau protein in the brain was not linked to worse cognitive performance in the mice. The results may mean that while there may be short-term tau protein build-up after TBI, this condition is not likely to directly cause post-TBI cognitive problems. (Journal of Neurotrauma, June 11, 2018)
|
Acquired stuttering after TBI and PTSD could be linked to medications
 Photo: ©iStock/Ivan-balvan (07/27/2018)
Veterans with both traumatic brain injury and PTSD were more likely to be diagnosed with acquired stuttering, and the condition could be linked to medications they were prescribed, found a South Texas Veterans Health Care System study. Researchers looked at data on more than 300,000 Iraq and Afghanistan Veterans. They found that 235 were diagnosed with acquired stuttering after their deployment. Of those, 43 percent had both TBI and PTSD. These patients had a greater likelihood of stuttering than those with only one or neither condition. Furthermore, over 66 percent of patients with stuttering were prescribed a medication that affects speech fluency, such as antidepressants and antiepileptic drugs. Based on the results, the researchers suggest that clinicians treating Veterans with complex conditions should consider the impact of medications on speech fluency. (Military Medicine, April 18, 2018)
|
Mantram meditation more effective than present-centered therapy at reducing PTSD symptoms
 Photo for illustrative purposes only. ©iStock/laflor (07/19/2018)
Mantram therapy was more effective than present-centered therapy at reducing PTSD symptoms, in a VA San Diego and New England Health Care System study. Patients with PTSD underwent eight weekly one-hour session of either mantram or present-centered therapy. In mantram meditation therapy, patients repeat a word or phrase with spiritual meaning to slow down thoughts and focus attention. Present-centered therapy focuses on currently stressful events and problem-solving skills. Those in the mantram group had significantly lower scores on a PTSD symptom scale after treatment and two months later. The mantram group also had lower self-reported PTSD symptoms and less insomnia. The results show that non-trauma focused complementary approaches such as mantram therapy can help alleviate PTSD symptoms, say the researchers. (American Journal of Psychiatry, June 20, 2018)
|
Intensive management outpatient program has similar cost to usual care
 Photo: ©iStock/Sasha_Suzi (07/19/2018)
High-risk patients received more outpatient care with no increase in total cost from an intensive management program, found a study at five VA medical centers. More than 2,000 patients with an average of seven chronic conditions were given either intensive outpatient management or usual care for one year. Intensive management involves care coordination, goals assessment, health coaching, medication reconciliation, and home visits through an interdisciplinary team. Those in the intensive management had an average of $2,164 lower inpatient costs than the usual care group. The intensive management had an average of $2,636 more in outpatient costs. Average total costs were similar for both groups. The results show that intensive management has potential, but room exists to improve the program and make it more efficient, according to the researchers. (Annals of Internal Medicine, June 19, 2018)
|
Possible mechanism behind TBI-related sleep-wake disturbances
 Photo: ©iStock/theasis (07/19/2018)
Researchers with the VA Portland Health Care System may have demonstrated how traumatic brain injury affects the sleep-wake pattern of the brain, using a mouse model. TBI often causes sleep-wake disturbances, such as excessive daytime sleepiness. Researchers have hypothesized that this is because of damage to neurons that make orexin, a hormone that regulates sleep. By studying the brains of mice with TBI, the researchers found that decreased density of the amino acid glutamate—which helps neurons function—could be responsible for problems with the orexin neurons. They also found that giving the mice branched-chain amino acid supplements through their food helped restore glutamate density and orexin neuron function. The results open up a path to potential therapy for sleep-wake disturbances caused by TBI. (Sleep, March 1, 2018)
|
Study shows safety of brain stimulation together with exposure therapy for PTSD
 Image courtesy of Dr. Albert Leung (07/11/2018)
Transcranial magnetic stimulation (TMS) along with prolonged exposure therapy may be beneficial for patients with PTSD, according to a Ralph H. Johnson VA Medical Center study. Eight patients with PTSD undergoing prolonged exposure therapy received either weekly repetitive TMS for five weeks or a control adjunct treatment. In TMS, a magnet is applied to the outside of the head to affect the electrical fields in the brain. Patients in the TMS group showed a trend toward improvement of PTSD symptoms, although the change was not statistically significant. The study demonstrates that TMS is safe to be delivered to PTSD patients while they are receiving prolonged exposure therapy. Larger studies are needed to see if this technique can be an effective treatment, say the researchers. (Journal of Electroconvulsive Therapy, June 26, 2018)
|
Movement-based therapies yield multiple benefits for patients with chronic conditions
 Photo by Robert Turtil (07/11/2018)
Patients saw improvements in a number of areas as a result of movement-based therapies, in a VA New England Healthcare System study. Researchers surveyed a focus group of 31 patients enrolled in yoga and qi gong programs for chronic conditions at two VA medical centers. The participants described improved physical and mental health, reduced opiate and psychotropic use, enhanced emotional well-being, and better social relationships as a result of the treatment. They attributed these changes to physical improvements, development of coping skills, and increased self-awareness. The researchers suggest health care providers consider referring patients with chronic conditions to movement-based complementary and integrative health therapies alongside usual care. (Chronic Illness, Jan. 1, 2018)
|
New drug-resistant form of E. coli rapidly spreading
 Photo: ©iStock/Dr_Microbe (07/11/2018)
A team including a Minneapolis VA Healthcare System researcher tracked the spread of a new drug-resistant strain of E. coli. The team gathered data on more than 6,000 E. coli infections at nine hospitals, including at the Minneapolis VA Medical Center. Twenty-one percent of the infections were resistant to fluoroquinolones, a common antibiotic. The most common strain of drug-resistant strain of E. coli was H30. The prevalence of this strain—which has been known since the 1990s—did not increase from the study years of 2016 to 2016. The second most common type of E. coli was ST1193. This strain is newer than H30, and its prevalence increased sevenfold between 2016 and 2017. It is more likely to occur in younger patients. The results show that the ST1193 of drug-resistant E. coli is on the rise, say the researchers, and more studies are needed on how to limit its spread. (Clinical Infectious Diseases, June 29, 2018)
|
Irregular discharges tied to higher suicide risk
 Photo for illustrative purposes only. ©Stock/Tempura (07/05/2018)
Patients are at an increased suicide risk after irregular hospital discharges, according to VA researchers in New England and Ann Arbor. Irregular hospital discharges include a patient leaving the hospital against medical advice and other unplanned discharges. The researchers looked at data on more than 5 million inpatient discharges from VA facilities between 2001 and 2014. About 2 percent were irregular. Patients with an irregular discharge from a general medical ward had three times higher risk of suicide than those discharged normally a year after their discharge. Patients with an irregular discharge from psychiatric care did not have higher suicide risk based on discharge type. The findings give important information on patient populations that may need to be targeted for suicide prevention, say the researchers. (Psychiatric Services, June 1, 2018)
|
Dialysis patients have lower mortality in VA vs. non-VA centers
 Photo: ©iStock/porpeller (07/05/2018)
Patients who initiated dialysis at VA facilities had lower mortality than patients who used non-VA dialysis centers, found a study of nearly 70,000 VA patients. Researchers looked at Veterans with end-stage kidney disease who began dialysis between 2007 and 2014. Ten percent used VA dialysis centers. Those in VA facilities were 13 percent less likely to die in the 12 months after they began dialysis. Along with that, patients in VA facilities were more likely than those in outside centers to be hospitalized at some point in the following year. The researchers suggest that the better outcomes may relate to VA's integrated health care system. Most VA dialysis centers are located within larger VA facilities. VA's integrated system may mean that patients are receiving more intense care addressing their health problems and have an easier transfer to hospital admission, say the researchers. (Clinical Journal of the American Society of Nephrology, June 14, 2018)
|
ICU telemedicine lowers hospital transfers
 Photo: ©iStock/Donghero (07/05/2018)
Intensive-care unit (ICU) telemedicine was linked to decreased interhospital transfers in an Iowa City VA Health Care System study. In ICU telemedicine, intensivist doctors can provide remote care to patients at regional facilities that may lack specialized personnel. The researchers looked at data for more than 550,000 admissions at 306 VA ICUs during a five-year period. Transfers to other hospitals decreased by 42 percent in hospitals with telemedicine programs, compared with a decrease of 7 percent in non-telemedicine hospitals during the same time period. The results may show that telemedicine allows hospitals to better evaluate when patients may effectively be treated locally, say the researchers. While ICU telemedicine did not reduce mortality in the study, past research suggests that limiting interhospital transfers lowers costs and improves patient, family, and staff satisfaction. (Chest, June 5, 2018)
|
Electrical signal change may explain link between combat exposure and psychiatric disorders
 Photo by Jerry Daliege (06/27/2018)
Increased error-related negativity (ERN) may help explain why combat exposure increases the risk of psychiatric disorders, found a Jesse Brown VA Medical Center and University of Illinois at Chicago study. ERN refers to a change in electrical signals in the brain as a result of making a mistake in a motor or cognitive task. Past research has linked it to various psychiatric disorders, such as anxiety and alcohol use disorders. In a study of 62 Veterans, the researchers used electroencephalography to show that those with greater combat exposure had greater ERN. This effect held true even after adjusting for anxiety and PTSD symptoms. The level of ERN was not associated with other life stressors before or after deployment, suggesting that this effect is specific to combat exposure. The results suggest that ERN may be one mechanism for how combat exposure increases the risk of psychiatric disorders, say the researchers, and could be a valuable screening tool for psychiatric disorder risk. (International Journal of Psychopsychology, July 2018)
|
Increased travel reimbursement leads to more VA health care use
 Photo: ©iStock/KarenMassier (06/27/2018)
Increased reimbursement for travel led to more VA outpatient use, found a VA Salt Lake City Health Care System study. A recent VA policy change increased how much Veterans can be reimbursed for travel expenses to receive VA health care. To study the effects of this change, researchers looked at data for 110,007 Veterans nationwide. They found that the number of VA outpatient visits increased by more than 30 percent after the rule change. The greatest increase was in Veterans living in rural areas. The number of non-VA outpatient care visits for rural Veterans also significantly decreased. A 2014 policy allows eligible Veterans to use their VA-provided health care at non-VA facilities. The results indicate how health care utilization may be affected by future policy changes. (Medical Care, July 2018)
|
Mental health service use remains stable after PTSD disability rating
 Photo: ©iStock/amesy (06/27/2018)
Use of VA mental health services largely remains stable after receipt of a service-connected disability for PTSD, according to a study by VA researchers in Ann Arbor and Boston. Some concern exists that Veterans will stop using mental health services after receiving service-connected disability benefits for PTSD, but actual usage patterns are not well-understood. Researchers looked at mental health service utilization for more than 22,000 Veterans one year before and after they received service-connected disability ratings for PTSD. They found that use remained stable for 80 percent of patients. Nine percent increased their use, and 11 percent decreased their use. While disability rating largely did not alter mental health service usage patterns, the researchers did find generally low utilization of these services. Opportunities exist to enhance outreach for Veterans with PTSD-related disability benefits, they conclude. (Health Services Research, April 17, 2018)
|
Review: Childhood sexual abuse can lead to sexual dysfunction in women
 Photo: ©iStock/chameleonseye (06/21/2018)
A review by Doris Miller VA Medical Center and University of Texas at Austin researchers confirmed that women with childhood sexual abuse histories had higher rates of sexual dysfunction, compared with women without a history of abuse. Lack of positive emotions related to sexuality appears to be the most relevant factor in sexual dysfunction. Lack of positive emotions was more common than direct negative emotions connected to sexuality. Studies show that mindfulness-based sex therapy and expressive writing treatments are effective for this group. More studies are needed on exactly how childhood sexual abuse can lead to sexual dysfunction, say the researchers. (Sexual Medical Reviews, April 2018)
|
If taller people are 'smarter,’ why is that? Brain study offers insight
 Photo for illustrative purposes only. ©iStock/XiXinXing (06/21/2018)
Cortical surface area may explain the connection between height and cognitive ability, found a study including a VA San Diego Healthcare System researcher. Previous studies have shown that greater height is correlated with greater general cognitive ability. But the reason for this relationship is not well-understood. The researchers looked at data from 515 participants of the Vietnam Era Twin Study of Aging. General cognitive ability was based on the Armed Forces Qualification Test, a measure similar to IQ. The researchers found that cortical surface area (brain size, taking into account the folds and layers of brain matter) is positively linked to cognitive ability. Taller people tend to have larger brains, and larger brains are linked to higher cognitive ability. Cortical thickness (total thickness of all brain layers) was not linked to cognitive ability. (Brain Structure & Function, May 11, 2018)
|
Suicidal behavior common with schizophrenia and bipolar disorder
 Photo: ©iStock/efks (06/21/2018)
A recent study confirmed that suicidal behavior is common among Veterans with schizophrenia or bipolar disorder. Researchers from the Bruce W. Carter VA Medical Center and VA Connecticut Healthcare System collected data on 3,942 Veterans with schizophrenia and 5,414 with bipolar disorder. They found that 70 percent of Veterans with schizophrenia had a history of suicidal thoughts or behavior. Of those with bipolar disorder, 82 percent had a history of suicidal thoughts or behavior. Veterans with more than one psychiatric condition were at the highest risk of suicide. The results underscore the need for continuous monitoring for suicidal behavior in patients with severe mental illness. (Journal of Psychiatric Research, April 21, 2018)
|
Homeless Veterans are more satisfied with specially tailored care teams
 Photo for illustrative purposes only. ©iStock/seb_ra (06/14/2018)
Homeless Veterans at VHA facilities with tailored primary care teams had better care experiences than non-homeless Veterans, according to a National Center on Homelessness Among Veterans study. Researchers surveyed more than 340,000 Veterans receiving care through VHA nationwide. About 4 percent were homeless. In facilities without homeless-tailored teams, homeless patients had more negative and fewer positive experiences than non-homeless patients. In facilities with Homeless Patient Aligned Care Teams (HPACTs), this pattern was reversed. HPACTs appear to offer homeless Veterans a better primary care experience than that received by non-homeless Veterans. (Medical Care, May 12, 2018)
|
Fluorouracil cream may lower treatment cost for those at high risk for skin cancer
 Photo: ©iStock/kali9 (06/14/2018)
Treating patients at high risk for two skin cancer conditions with topical fluorouracil cream can provide cost savings, found a VA Palo Alto Health Care System study. Previous research shows that fluorouracil reduces incidence of keratinocyte carcinoma (nonmelanoma skin cancer) and actinic keratosis (a precancerous skin condition). Patients at high risk for the conditions applied either the fluorouracil or a placebo cream to their faces and ears for four weeks. After one year, those not using fluorouracil had more treatment visits for squamous cell carcinoma than those using it. Over three years, patients using fluorouracil had average treatment costs of $771 less per patient. (Journal of the American Academy of Dermatology, March 2, 2018)
|
Photodynamic therapy may effectively treat bladder cancer
 Photo: ©iStock/wildpixel (06/14/2018)
A group including a VA Northern California Health Care System researcher showed that a photodynamic therapy technique could effectively treat bladder cancer. In photodynamic therapy, medication that is activated by light and heat is injected into the body. The cancer site can then be exposed to light, which allows the cancer cells to be closely targeted. This process has significantly fewer side effects than treatments such as chemotherapy. The researchers used the drug 17AAG to target bladder cancer in animal models. They combined 17AAG with the organic compound nanoporphyrin. 17AAG is not very water-soluble. Combining it with nanoporphyrin allows it to be absorbed by cells more easily. The results show that the NP-AAG was effectively accumulated in cancer cells. A single intravenous injection followed by multiple light treatments over seven days effectively eradicated the tumors. This technique could dramatically improve bladder cancer management with minimal toxicity, say the researchers. (Nanomedicine, April 2018)
|
Gender-tailored alcohol screening improves detection among women
 Photo: ©iStock/kieferpix (06/06/2018)
Gender-tailored binge-drinking screens may improve detection of women's unhealthy alcohol use, according to a study by researchers from several VA systems. Women and men have different patterns of alcohol consumption. But the usual screens for binge drinking are based on men's drinking patterns. Researchers adjusted the AUDIT-C assessment to specifically address women's drinking patterns. In a survey of more than 1,000 women Veterans, 6 percent screened positive for unhealthy alcohol use on the standard assessment. When a gender-tailored binge-drinking question was added (asking how often participants had four or more drinks on one occasion, as opposed to six or more on the unaltered AUDIT-C), 10 percent screened positive. When researchers lowered the threshold score for what was considered unhealthy alcohol use, 21 percent of women screened positive. Using both the tailored question and lowered threshold, 25 percent screened positive for unhealthy alcohol use. Using gender-tailored screening could improve alcohol screening in women, say the researchers. (American Journal of Addictions, March 2018)
|
Longer ‘dwell time’ linked to fewer PTSD symptoms
 Photo by Petty Officer 1st Class Holly L. Herline/USN (06/06/2018)
Longer time home between deployments, or “dwell time,” is linked to fewer long-term PTSD symptoms in Veterans, found a Central Texas Veterans Health Care System study. Researchers looked at data for 278 Veterans of Iraq and Afghanistan three years after discharge. They found that those with time between deployments less than 12 months had the highest long-term PTSD symptoms. Consistent with other studies, combat exposure was linked to more PTSD symptoms. Average length of deployment and number of deployments did not significantly affect long-term PTSD symptoms; intensity of combat exposure had a much bigger effect than either. The researchers conclude that “in addition to combat exposure, time between deployments warrants clinical attention as an important deployment characteristic for predicting long-term PTSD symptoms.” (Journal of Clinical Psychology, April 2018)
|
Acceptance and commitment therapy prior to surgery may help pain outcomes
 Photo: ©iStock/kupicoo (06/06/2018)
Acceptance and commitment therapy led to a quicker end to pain and opioid use after surgery, in an Iowa City VA Medical Center study of 88 patients. High levels of pain, anxiety, and depressive symptoms before surgery put patients at elevated risk of chronic pain and prolonged opioid use following surgery. Patients scheduled for orthopedic surgery attended a one-day acceptance and commitment therapy workshop prior to surgery. The workshop focused on pain acceptance and values-based behavior. Three months following surgery, patients who attended the workshop achieved pain reduction and opioid cessation sooner than those who had treatment as usual. The benefits of the therapy were greatest for patients with post-operative complications. The results suggest that pre-operative pain management may help prevent chronic pain after surgery. (Journal of Pain, May 16, 2018)
|
Cannabis use disorder linked to self-injury
 Photo: ©iStock/digihelion (06/01/2018)
Cannabis use disorder was linked to greater odds of self-injury, in a study by Durham VA Medical Center and Central Texas VA Health Care System researchers. The researchers interviewed 292 Iraq and Afghanistan Veterans. Of those, 13 percent had engaged in either suicidal or non-suicidal self-injury. Fourteen percent of Veterans interviewed had cannabis use disorder—defined as continued use of marijuana despite impairment and dependence. Participants with cannabis use disorder had three times higher odds of any type of self-injury, compared to those without the disorder. The odds of non-suicidal self-injury were higher than the odds of suicide attempts for participants with cannabis use disorder. While the results may show that cannabis use disorder increases the risk of self-injury, the basis for this link is not yet clear, caution the researchers. (Suicide and Life-Threatening Behavior, April 9, 2018
|
New insight to guide dialysis decisions
 Photo: ©iStock/porpelle (06/01/2018)
For patients with chronic kidney disease, the level of kidney function at which dialysis improves survival varies by age, according to a study by VA Palo Alto Health Care System and Stanford University researchers. Using data from more than 70,000 Veterans with chronic kidney disease, the researchers compared survival rates of patients on dialysis with those of patients treated without dialysis. They looked at patients' eGFR levels when they were on dialysis. eGFR is a measure of waste products in the blood, and is used to test kidney function. Higher scores mean better kidney function. For patients 75 or older, risk of death was lower than with medical management for eGFR levels of 6-9 or lower. For those age 65-74, risk of death was lower at eGFR below 6. For those younger than 65, the eGFR level at which dialysis improved survival compared with medical management was 6-9. The results show that age should be taken into consideration when deciding to put patients on dialysis. (Journal of the American Society of Nephrology, May 22, 2018
|
Alcohol-related treatment low in hepatitis C patients
 Photo: Mitch Mirkin (06/01/2018)
Many patients with hepatitis C do not receive recommended alcohol-related care, found VA Puget Sound Health Care System researchers. Alcohol use increases the risks associated with hepatitis C. More than 30,000 VA patients with both hepatitis C and unhealthy alcohol use were studied over a four-year period. Seventy-two percent had a brief alcohol intervention, 13 percent pad specialty addiction treatment, and only 3 percent had drug treatment for problematic alcohol use. For those with alcohol use disorder, 27 percent used specialty addiction treatment and 6 percent used drug treatment. Strategies are needed to increase alcohol-related care and pharmacotherapy for alcohol use disorder in patient with hepatitis C, say the researchers. (Drug and Alcohol Dependence, May 8, 2018
|
Review study: Exercise helps lungs even in those with chronic lung disease
 Photo for illustrative purposes only: ©iStock/kali9 (05/17/2018)
Studies show that whole-body exercise training improves pulmonary function in adults with chronic lung disease, according to a VA New Jersey Health Care System review. The general consensus was that exercise does not stimulate and improve lung function in this population. The researchers looked at 21 randomized controlled trials to see if this assumption was supported by evidence. They found that exercise training resulted in small but significant improvements in measures of pulmonary function for patients with chronic lung disease. The findings suggest that pulmonary treatment should include exercise to improve lung function, in addition to care to reduce symptom burden. (Archives of Physical Medicine and Rehabilitation, April 17, 2018)
|
Frequent hospital urine cultures lead to unnecessary antibiotic use
 Photo: ©iStock/sercan samanci (05/17/2018)
Patients with a urine culture taken on the first day of hospital admission receive more days of antibiotics and have longer hospital stays than patients who do not have a urine culture, found a Michael E. DeBakey VA Medical Center study. The researchers looked at data for nearly 90,000 patients in 230 U.S. hospitals admitted for any reason. They found that patients who had their urine tested for bacterial infection had more days of inpatient antibiotic use. Those tested had an average of 2.1 percent longer hospital length of stay. Positive urine cultures often lead providers to give patients antibiotics even when they do not need them. In many cases, antibiotics are not necessary even when bacteria is found in the urine if the patient does not have symptoms of an infection. Unnecessary antibiotic use contributes to antibiotic resistance and is a threat to public health, write the researchers. Steps should be taken to limit unnecessary urine cultures, they say. (Infection Control and Hospital Eipdemiology, May 2018)
|
Therapeutic horseback riding may reduce PTSD symptoms
 Photo for illustrative purposes only: ©iStock/debibishop (05/17/2018)
A therapeutic horseback riding program reduced PTSD symptoms in a small study of 29 Veterans. The study team included a Harry S. Truman Memorial Veterans' Hospital researcher. Half the Veterans took a six-week horseback riding program, while the others were put on a wait-list. Those who rode had a 67 percent likelihood of a lower PTSD symptom score after three weeks. The likelihood increased to 88 percent after six weeks. Participants showed improvement in self-efficacy and emotion regulation. The results show that therapeutic horseback riding may be an effective way to alleviate PTSD symptoms for some Veterans. (Military Medical Research, Jan. 19, 2018)
|
Possible biological effect of cognitive behavioral therapy
 Photo: ©iStock/Evgeny Gromov (05/11/2018)
Researchers with the South Texas Veterans Health Care System and University of Texas Health Science Center at San Antonio may have identified a biological explanation for how psychotherapies improve stress-related psychiatric illness. Cognitive behavioral therapies have been shown to improve symptoms in PTSD and depression, but the mechanism is unknown. Researchers used a drug to block activity in the ventral medial prefrontal cortex of rats. Fear extinction therapy, which usually reverses stress-induced cognitive dysfunction in rats, did not work when rats were on the drug. The study also showed that chronic stress decreased this brain region’s response to stimulation. This tells the researchers that activity in the prefrontal cortex may underlie the benefits of cognitive behavioral therapy. The results support the idea that modulating activity in the prefrontal cortex, for example, through a medication, could boost the effectiveness of cognitive behavioral therapies for PTSD and other mental disorders. (Journal of Neuroscience, Feb. 7, 2018)
|
PTSD from military sexual trauma, versus other causes, may have stronger link to suicidal thoughts
 Photo: ©iStock/kitzcorner (05/11/2018)
Female Veterans with PTSD as a result of military sexual trauma were twice as likely to have suicidal thoughts as those with PTSD from any other cause, found a Denver VA Medical Center study. Researchers surveyed more than 300 female Veterans who had experienced military sexual trauma. Of those, 29 percent said they have current suicidal thoughts, and 72 percent said military sexual trauma was the source of their PTSD symptoms. Women who identified military sexual trauma as the source of their PTSD were at least three times as likely to have suicidal thoughts as those who said their PTSD was specifically related to combat or deployment. The study shows the importance of addressing PTSD specifically related to military sexual trauma, say the researchers. (Suicide and Life-Threatening Behavior, April 20, 2018)
|
Stimulant use increases mortality risk for HIV-infected men
 Photo: ©iStock/tinors (05/11/2018)
Stimulant use increases mortality risk for HIV-infected men
Stimulant use increases mortality risk for men with HIV, but cannabis use does not, according to the Veterans Aging Cohort Study. Researchers surveyed more than 3,000 men with HIV. At baseline, 15 percent of participants used cannabis, or marijuana; and 24 percent used stimulants, such as cocaine and methamphetamines. Cannabis was not linked to increased mortality risk based on the VACS Index, a measure of the risk of all-cause mortality. Those using stimulants, however, scored five points higher on the risk scale, compared with cannabis and alcohol users. Participants who used stimulants were also more likely to have unhealthy alcohol and opioid use. This was not true for those who used cannabis. The results suggest that efforts to reduce stimulant use in this population may reduce mortality. The researchers do note that demographic factors—such as age, race, and education—seem to impact mortality risk more than alcohol, cannabis, or stimulant use. (AIDS and Behavior, April 2018)
|
Pulsed xenon ultraviolet leads to better disinfection
 Photo courtesy of www.xenex.com (05/03/2018)
Pulsed xenon ultraviolet devices disinfect more effectively than manual cleaning, found a study by researchers at multiple VA centers. The devices use bulbs that contain xenon, a gas, to emit short bursts of high-energy ultraviolet light. Researchers tested surfaces in two hospital rooms cleaned using pulsed xenon ultraviolet and two cleaned with manual disinfection. Staphylococcus aureus counts were reduced by 75 percent in the UV rooms, compared with pre-cleaning counts. Aerobic bacteria colony counts were reduced by 84 percent in the UV rooms. Manual disinfection reduced bacteria counts only by 25 to 30 percent. The researchers recommend that this technology be integrated into daily hospital operations. (American Journal of Infection Control, April 11, 2018)
|
Caloric restriction changes liver metabolism, shows primate study
 ©iStock/Duka82 (05/03/2018)
Restricting calories may delay the onset of age-related disorders and extend the lifespan by changing how the liver metabolizes various molecules, according to a study led by a William S. Middleton Memorial Veterans Hospital researcher. Caloric restriction has been shown to ward off disease and extend life in many species. To look for a possible molecular explanation, the researchers put male rhesus monkeys on a diet that was 30 percent lighter in calories than a standard diet, for two years. They then took liver biopsies and conducted high-resolution molecular profiling of the tissue. The team found that caloric restriction changes gene expression relating to liver metabolism. Their report describes the changes in detail, with a focus on RNA processing. They say the work represents a “comprehensive, integrated account of the molecules and pathways recruited by [caloric restriction] that may underlie the longevity benefits.” (Cell Metabolism, March 6, 2018)
|
Researchers report technical breakthrough for brain-computer systems
 Adapted from JN article (05/03/2018)
A team that included researchers from the Providence VA Medical Center showed how “local field potentials”— the total electrical current flowing to a small section of nervous tissue in the brain—may be a more robust, stable signal for brain-computer systems than neuronal action potentials, which represent the activity of individual brain cells. The study involved one person with ALS and another with locked-in syndrome due to a stroke. In locked-in syndrome, the person is mentally engaged but unable to speak or move his or her limbs. The two participants were able to type messages and emails for 138 and 76 days, respectively, without needing re-calibration of their brain-computer systems. Past studies in which the decoding of brain signals was based on neuronal action potentials had required far more frequent re-calibration. The researchers say they have achieved a “new benchmark” for stability, using local field potentials. “This study is a step towards a reliable and robust [brain-computer interface] that will allow people with [locked-in syndrome] to communicate independently and, therefore, provide greater and more extensive interactions with their friends, family, and caregivers.” (Journal of Neurophysiology, April 25, 2018)
|
Up to nine months between doctor's visits do not worsen viral load for HIV patients
 Photo: ©iStock/NanoStockk (04/25/2018)
Gaps up to nine months between HIV primary care visits do not worsen viral load, found a study including a Michael E. DeBakey VA Medical Center researcher. Current guidelines say that HIV patients should visit their doctors every six months for viral monitoring. Looking at more than 6,000 patients with HIV, researchers found that patients who went up to nine months between doctor's visits did not have significant increases in viral load. Patients with visit gaps greater than 12 months were much more likely to have lost viral suppression. The results show that primary care visit intervals between six and nine months may be appropriate for HIV patients, say the researchers. (AIDS Patient Care and STDs, April 2018)
|
Probiotic reduces S. aureus infection odds in GI tract
 Photo: ©iStock/RomaRiolen (04/25/2018)
Probiotics can reduce Staphylococcus aureus infection in the gastrointestinal tract, according to a William S. Middleton VA Medical Center study. Patients with S. aureus infection were given either the probiotic Lactobacillus rhamnosus HN001 or a placebo for four weeks. Those taking the probiotic had 83 percent reduced odds of S. aureus presence in their GI tract after treatment, compared with the placebo group. However, those with S. aureus infection somewhere other than the GI tract only had 15 percent lower S. aureus colonization. The results show that oral L. rhamnosus could be a useful treatment for S. aureus infection in the GI tract. (BMC Infectious Disease, March 14, 2018)
|
Possible explanation for how melatonin promotes sleep
 Photo: ©iStock/jhorrocks (04/25/2018)
Researchers at the Harry S Truman Memorial VA Hospital have identified a possible mechanism that explains how melatonin promotes sleep. Melatonin, sold in supplement form, is widely prescribed nowadays as a sleep aid, but how exactly it works is unclear. Researchers studied how the brains of mice responded to melatonin. They found that orexin neurons in the brain expressed MT1, a melatonin receptor protein. When the researchers infused melatonin into the brain, the mice showed increased REM sleep and reduced wakefulness. Melatonin infusion inhibited orexin neurons. The results show that melatonin may act via the MT1 receptors to inhibit orexin neurons and promote sleep. The researchers point out that while the finding helps explain an existing treatment, it also may lead to new ones. (Journal of Pineal Research, April 14, 2018)
|
Certain psychotropic drugs increase risk of QT prolongation in PTSD patients
 Photo: ©iStock/evryka23 (04/25/2018)
Certain drugs used to treat PTSD could lead to dangerous heart conditions, found researchers from several VA systems. Several psychotropic drugs used to treat depression and sometimes given for PTSD have recently been linked to QT prolongation. QT prolongation is an abnormal heart rhythm that can cause fainting, seizures, and even sudden death. The researchers looked at administrative data of VA patients with PTSD. They found that patients on the antipsychotic drug ziprasidone (sold under the brand name Geodon, among others) and the anti-anxiety drug buspirone (sold as Buspar) had increased risk of QT prolongation, while those on the SSRI antidepressants citalopram (sold as Celexa and other brands) and fluoxetine (Prozac and other brands) did not. The researchers also found that patients with QT prolongation had a higher risk of death than those without. They recommend that prescribers and patients consider these risks when deciding on treatments for PTSD. (Annals of Pharmacotherapy, April 1, 2018)
|
Telemental health useful for women Veterans
 Photo for illustrative purposes only. ©iStock/RapidEye (04/19/2018)
Telemental health is seen as a good fit to address the needs of women Veterans, according to a survey by the VA Center for the Study of Healthcare Innovation, Implementation and Policy. Researchers interviewed 40 VA leadership and clinical employees. Respondents believed that telemental health could increase access to care, especially for rural women and those with other barriers to care. Telemedicine was seen as particularly useful for women with responsibilities related to child care, spousal care, and elder care. The findings could help guide gender-tailored expansion of telemedicine. (Women's Health Issues, March-April 2018)
|
Self-report survey data improves violence risk prediction in soldiers
 Photo for illustrative purposes only. ©iStock/Wavebreakmedia (04/19/2018)
Data from the Army STARRS New Soldier Survey can improve the accuracy of interpersonal violence risk prediction, found a study that included a VA Eastern Colorado Health Care System researcher. The survey was given to more than 21,000 Army recruits. When using both survey and administrative data, researchers were able to predict soldiers’ involvement in physical or sexual violence with greater accuracy than with administrative data alone. The greatest change was in predicting whether women soldiers would be victims of sexual violence. Overall accuracy increased to 29 percent, up from 18 percent with administrative data only. The researchers believe that the increased accuracy might offset the survey costs. (BMC Psychiatry, April 3, 2018)
|
Blood cancer patients with cognitive impairment may have worse survival
 Photo: ©iStock/Dr._Microbe (04/19/2018)
Cognitive impairment was linked to worse survival rates in patients with blood cancers, in a study that included VA Boston Healthcare System researchers. They looked at 341 elderly patients with leukemia, myeloma, or lymphoma. Of those, 127 had executive dysfunction and 62 had impaired working memory. Those with impaired working memory had lower median survival, regardless of treatment type. Executive dysfunction was linked with worse survival only for those undergoing intensive treatment. While age is the main cause of cognitive impairment, some cancer-fighting drugs may further impair cognition. Other cancer treatments, as well, may worsen existing health conditions. The results show that targeted interventions are needed for cancer patients with cognitive impairment, say the researchers. (JAMA Oncology, March 1, 2018)
|
Increased exercise may improve cognitive function shortly after breast cancer surgery
 Photo for illustrative purposes only. ©iStock/Steve Debenport (04/11/2018)
An exercise program improved cognitive functioning in patients diagnosed with breast cancer within the past two years, in a study including a VA San Diego Healthcare System researcher. Increased physical activity has been shown to improve cognition in both healthy and cognitively impaired adults. This study aimed to see how exercise specifically benefitted cancer survivors. Patients within two years post-surgery scored better on a test of processing speed after a 12-week exercise program, compared with those not in the exercise program. However, patients who had surgery more than two years previously did not show faster processing. The results suggest that early implementation of an exercise intervention could have benefits for breast cancer survivors, say the researchers. (Cancer, Jan. 1, 2018)
|
High BMI linked with early, but not later, survival after hospitalization
 Photo for illustrative purposes only. ©iStock/GlobalStock (04/11/2018)
Overweight or obese BMI is linked with improved survival after hospitalization, but only in the short term, found a study by VA Ann Arbor Healthcare System and NYU School of Medicine researchers. The study looked at survival rates for older patients hospitalized for congestive heart failure, pneumonia, and heart attack. Patients with overweight or obese BMI had lower mortality one year after hospitalization. However, after one year these patients did not have better survival rates than those with lower BMI. While previous studies have shown the link between higher BMI and lower risk of death after hospitalization in the short term, less data are available on the effects long-term. While obesity may be protective in the short term, this connection is a source of debate. Obesity may be protective against in-hospital mortality, but still hazardous for longer-term mortality, according to the researchers. (BMC Geriatrics, Feb. 6, 2018)
|
Accepting hepatitis C-positive liver transplants could improve life expectancy
 Photo: ©iStock/Natali_Mis (04/11/2018)
Patient without hepatitis C needing a liver transplant may have increased life expectancy if they are willing to accept a donated liver that is positive for the hepatitis C virus, according to a mathematical model. A team including a researcher from the Michael E. DeBakey VA Medical Center used data from published studies to create a simulated trial. They found that accepting any liver regardless of hepatitis C status resulted in increased life expectancy over waiting for a liver free of the hepatitis C virus. Although infected livers could have adverse outcomes, the virus can now be treated very effectively post-transplant using direct-acting antivirals. (Hepatology, Dec. 9, 2017)
|
Detecting coronary heart disease using genetic data
 Photo: ©iStock/wildpixel (04/04/2018)
A team including an Iowa City VA Healthcare System researcher used machine learning to detect coronary heart disease by combining genetic and epigenetic data. Epigenetics is the study of what causes genes to be expressed—basically, to get translated into proteins or other molecules that effect changes in the body. The program was able to classify heart disease with 78 percent accuracy, in a group of 142 patients. A comparison test using conventional heart disease risk factors—such as age, cholesterol level, and smoking status—was only 65 percent accurate. The results show that using computer algorithms with genetic data could lead to better ways to detect coronary heart disease, say the researchers. (PLoS One, Jan. 2, 2018)
|
‘Autonomy support’ linked to better diabetes control
 Photo: ©iStock/AndreyPopov (04/04/2018)
Autonomy support from family or friends may help people better control their diabetes by relieving diabetes distress, according to a study by the VA Center for Clinical Management Research. Autonomy support is social support that encourages patients to control their own care. Many people with diabetes experience emotional distress from diabetes symptoms, the stress of keeping up with care regimens, and fear of complications from the disease. Studying 308 Veterans with diabetes, researchers found that high diabetes distress was linked to poor glycemic control. Those with greater autonomy support had greater glycemic control than those without. (Diabetes Care, March 29, 2018)
|
Low systolic blood pressure linked to worse outcomes for heart failure patients
 Photo: ©iStock/PeopleImages (04/04/2018)
Low systolic blood pressure is linked to worse outcomes in patients with heart failure with preserved ejection fraction, found Washington DC VA Medical Center researchers. Heart failure with preserved ejection fraction involves increased stiffness of the heart's left ventricle and less relaxation of the ventricle when filling with blood before the next beat. Out of more than 1,800 patients hospitalized with this condition, 10 percent of patients with systolic blood pressure less than 120 mm Hg at discharge died within 30 days, compared with 5 percent of those with systolic blood pressure higher than 120 mm Hg. Those with lower blood pressure also had higher risk of death one year after hospitalization. The researchers conclude that future studies should look at optimal systolic blood pressure treatment goals for patients with this condition. (JAMA Cardiology, Feb. 14, 2018)
|
Site mentoring can improve clinical trial recruitment
 Photo: Christopher Pacheco (03/28/2018)
A site mentoring model improved recruitment for clinical trial participation, in a VA Cooperative Studies Program study. As part of the CONFIRM trial, which studies colorectal cancer, teams with expertise in managing multi-site clinical trials worked one-on-one with low-enrolling CONFIRM sites to identify and overcome barriers to recruitment. Sites being mentored had an average improvement of five participants per month. A majority of sites had improved participant recruitment and participant screening for eligibility three months after the mentoring. The success of this pilot program shows that a site mentoring model could help improve recruitment for future clinical trials, according to the researchers. (Contemporary Clinical Trials Communications, March 2018)
|
Outpatient medical care linked to lower drug use in rural patients
 Photo: ©iStock/JTSorrell (03/28/2018)
Use of outpatient medical care is linked to reductions in illicit drug use over time in rural areas, found a study by Central Arkansas VA Healthcare System researchers and their colleagues. The researchers looked at how outpatient medical care for other issues affected substance use in 710 stimulant users in rural areas of Arkansas, Kentucky, and Ohio. They found that patients with at least one outpatient medical care visit over a three-year period had lower alcohol, crack cocaine, and methamphetamine use over time, compared with patients who did not have any outpatient visits. The findings highlight the importance of medical care contact in addressing unhealthy substance use, say the researchers. (American Journal of Drug and Alcohol Abuse, 2018)
|
Gene variant, mild traumatic brain injury combination lead to greater risk of Alzheimer's
 Photo: ©iStock/yodiyim (03/28/2018)
Mild traumatic brain injury may be connected to lower hippocampal volume in people with a gene variant linked to Alzheimer's disease risk, according to a VA Boston Healthcare System study. Lower volume of the hippocampus (a region of the brain) has been shown to be a sign of Alzheimer's disease. Previous research has shown that severe TBI can lead to hippocampus atrophy, but less evidence of this exists for mild TBI. The researchers looked at the genes of 165 Veterans with at least one mild TBI. They found that a combination of a specific gene variant previously linked to Alzheimer's and mild TBI was a good predictor of hippocampal volume. The results suggest that people with this gene variant are at greater risk for neurodegeneration after exposure to a mild TBI. (Genes, Brain, Behavior, Feb. 2018)
|
Apalutamide could delay metastasis of prostate cancer
 Photo: ©iStock/jamesbenet (03/21/2018)
Patients with prostate cancer taking the drug apalutamide went longer without the cancer metastasizing than those taking placebo, in an international study including a researcher from the VA Portland Health Care System. Patients taking daily apalutamide went a median of 40.5 months before the cancer metastasized (spread to bone or other organs). Those in the placebo group had a median of 16.2 months before metastasis. Three percent more patients in the apalutamide group than in the placebo group had adverse events, such rash, hypothyroidism, and fracture. Janssen Research and Development, the makers of apalutamide, funded the study and were involved in the research. (New England Journal of Medicine, Feb. 8, 2018)
|
Vets with mental health diagnoses have higher risk of respiratory problems
 Photo: USMC (03/21/2018)
Veterans of the wars in Afghanistan and Iraq with mental health diagnoses are more likely to have respiratory problems, found a VA Portland Health Care System study. Researchers looked at data for more than 180,000 Veterans. Fourteen percent had a respiratory condition such as bronchitis, asthma, or COPD. Of those, 77 percent also had a mental health condition diagnosis. Those with a mental health condition were more likely to have a respiratory condition, but the reverse was not true. While the results do not show causation between the two conditions, they show the importance of care coordination for Veterans with multiple conditions, according to the researchers. (Military Medicine, Feb. 6, 2018)
|
Study: Written exposure therapy as effective as cognitive processing therapy
 Photo for illustrative purposes only. ©iStock/Lyashik (03/21/2018)
Written exposure therapy had similar effects to cognitive processing therapy for treating PTSD, found a VA Boston Health Care System study. Cognitive processing therapy is considered the gold
standard for PTSD treatment. Written exposure therapy involves five weekly sessions, compared with 12 sessions in cognitive processing therapy. The researchers assigned 63 patients to written exposure therapy and 63 to cognitive processing therapy. Participants in written exposure therapy had similar improvements in PTSD symptoms as cognitive processing therapy participants after 36 weeks. The findings suggest that written exposure therapy could offer an efficient PTSD treatment for patients unlikely to complete longer-term therapy, say the researchers. (JAMA Psychiatry, March 1, 2018)
|
Cardiac rehabilitation participation lower than recommended
 Photo for illustrative purposes only. ©iStock/juanmonino (03/14/2018)
Cardiac rehabilitation participation after cardiovascular incidents (e.g., heart attack, bypass surgery) is low despite being recommended by guidelines, found a study by VA researchers and colleagues. Rehabilitation includes exercise training, risk factor modification, and psychosocial counseling. The researchers found that 16 percent of Medicare patients and only 10 percent of VA patients participated in cardiac rehabilitation after a cardiovascular event. However, they found wide regional variation in both Medicare and VA, ranging from 1 to 48 percent, depending on the state. The northern Midwest had the highest participation, while the Pacific region had the lowest. The researchers believe that best practices from hospitals with higher participation could improve the rates of rehabilitation at other hospitals. (Circulation, Jan. 5, 2018)
|
Neuropeptide Y may not be good biomarker for PTSD
 Photo by Cpl. Manuel Serrano/USMC (03/14/2018)
Neuropeptide Y levels were not found to indicate PTSD risk, in a Dutch and American study including a VA San Diego Healthcare System researcher. Neuropeptide Y is a neurotransmitter associated with the stress response. Previous research had suggested that high neuropeptide Y levels might protect against PTSD. The researchers looked at neuropeptide Y levels in 3,319 U.S. Marines and Dutch service members both before and after deployment. They did not find any connection between neuropeptide Y levels and level of PTSD symptoms at either time point. The results suggest that neuropeptide Y may not be a useful biomarker for PTSD risk, say the researchers. (Biological Psychology, Feb. 19, 2018)
|
Polytrauma inpatient rehabilitation effective long-term
 Photo courtesy of Tampa VAMC (03/14/2018)
Patients with traumatic brain injury treated at a VA polytrauma rehabilitation center continued to show improved function in the long term, found a VA Palo Alto Health Care System study. Researchers looked at 44 patients admitted to the inpatient rehabilitation unit in 2006. They found that functional gains made between admission and discharge were maintained eight years later. After eight years, more than 50 percent of patients were either competitively employed or continuing their education. All patients were living in a noninstitutionalized setting. The results show that the established Polytrauma System of Care is both effective and durable. (Archives of Physical Medicine and Rehabilitation, February 2018)
|
Evidence lacking on benefits of cranial electrical stimulation
 Image courtesy of study authors (03/08/2018)
A West Los Angeles VA Medical Center review found evidence is lacking on the benefits of cranial electrical stimulation for a number of conditions. In CES, doctors apply low-intensity electrical current to the head using electrodes. Evidence from 26 studies was insufficient to show that CES helped patients with fibromyalgia, headache, neuromusculoskeletal pain, degenerative joint pain, depression, or insomnia. Some studies suggested benefit for patients with anxiety and depression, but the evidence was low-strength. Low-strength evidence suggested that CES does not cause serious side effects. Larger randomized trials of higher quality, better execution, and longer follow-up are needed to show whether CES actually helps for these conditions, say the researchers. (Annals of Internal Medicine, Feb. 13, 2018)
|
Cognitive processing therapy and prolonged exposure therapy equally effective at treating PTSD
 ©iStock/Highwaystarz-Photography (03/08/2018)
Cognitive processing therapy and prolonged exposure therapy are equally effective at treating PTSD, found a study by researchers at the Dwight D. Eisenhower VA Medical Center in Leavenworth, Kansas. Researchers looked at medical charts for 750 Veterans with PTSD who underwent one of the two treatments. Patients who completed either therapy showed significantly lower PTSD symptoms, compared to those who did not complete therapy. There were no significant differences in symptom reduction between the two therapies. Both forms of psychotherapy are widely used in VA, and have been shown in many studies to improve PTSD symptoms. Cognitive processing therapy focuses on teaching patients how to evaluate and change upsetting thoughts related to trauma. Prolonged exposure therapy involves remembering and confronting trauma-related memories rather than avoiding them. This study adds to the existing evidence that either therapy is an effective treatment for PTSD. (Psychological Reports, April 2018)
|
Balanced high fat-diet reduces cardiovascular risk
 Photo:©iStock/Dusan Vidar (03/08/2018)
A balanced high-fat diet reduces cardiovascular risk in obese women, found a study by VA Tennessee Valley Healthcare System researchers and their colleagues. In a balanced high-fat diet, total saturated fat is reduced and total unsaturated fat is increased proportionally. The diet balances the type of fat consumed to one-third saturated, one-third monounsaturated, and one-third polyunsaturated. All the women in the study had lower cardiovascular risk factors after the diet, but European-American women and African-American women responded differently. European-American women saw lower scores in measures related to apolipoprotein B, the main protein involved in LDL cholesterol. African-American women sow reductions related to apolipoprotein A1, the main protein related to HDL cholesterol. The results show that ethnicity and genetics should be considered when planning diet therapy, according to the researchers. (Metabolism, Jan. 27, 2018)
|
Topical fluorouracil reduces risk of some skin cancer and lowers treatment costs
 Photo: ©Stock/artenex (03/08/2018)
Treatment with a fluorouracil cream can lower risk for one form of skin cancer and reduce treatment costs, according to two papers by VA researchers. Both papers were part of the VA Keratinocyte Carcinoma Chemoprevention Trial. Keratinocyte carcinoma refers to two types of non-melanoma skin cancer: cutaneous basal cell carcinoma and squamous cell carcinoma. Keratinocyte carcinoma accounts for about three-quarters of all cancers in the U.S. In the trial, 932 Veterans with a history of skin cancer applied topical fluorouracil—a medication used to treat cancer—to their face and ears twice daily for two to four weeks. The first paper reported that patients treated with fluorouracil had a 75 percent lower risk than those treated with placebo of developing squamous cell carcinoma in the year following treatment. Patients in the fluorouracil group were also significantly less likely to undergo Mohs surgery for either type of cancer. Fluorouracil did not reduce risk of basal cell carcinoma in the first year, or of risk of either cancer after four years. The second paper showed that patients in the fluorouracil group incurred $771 less in treatment costs over a three-year period, compared with the placebo group. Patients treated with fluorouracil had fewer appointments for squamous cell carcinoma. The results show that a topical treatment of fluorouracil substantially reduced surgery for squamous cell carcinoma and provided cost-savings for the VA health care system. (Journal of the American Academy of Dermatology, March 2, 2018)
|
Lab study suggests curcumin could improve memory, mood in Gulf War illness
 Photo:©iStock/onairjiw (02/27/2018)
Curcumin may lead to better cognitive and mood for those with Gulf War illness, according to a rat study by Olin E. Teague Veterans' Medical Center and Texas A&M researchers. Curcumin is a natural antioxidant compound found in turmeric and other plants, and is sometimes sold as an herbal supplement. Rats with simulated Gulf War illness symptoms were treated with either curcumin or a placebo for 30 days. Those in the curcumin group had better cognitive and mood function, based on behavioral tests. They also had better neurogenesis (growth and development of nerve tissue) and lower inflammation than the placebo group. The researchers hypothesize that changes in gene expression caused by curcumin could improve memory and mood symptoms related to Gulf War illness. (Brain, Behavior, and Immunity, Feb. 15, 2018)
|
One-day workshop shows promise for migraine sufferers
 Photo for illustrative purposes only. ©iStock/g-stockstudio (02/27/2018)
A one-day behavioral intervention workshop for Veterans with migraine improved symptoms and pain acceptance, found a Houston VA HSR&D Center for Innovation and Baylor College of Medicine study. Twenty-five Veterans with migraines along with depression or anxiety attended the workshop, which featured education and elements of acceptance and commitment therapy, a type of cognitive behavioral therapy. Participants said that that the workshop helped them better understand their condition and empowered them to better manage their headaches. The training led to greater awareness of how stress can make headaches worse. At a three-month follow-up, participants had significantly improved depressive and anxiety symptoms, general functioning, and headache-related disability. Findings of this small trial suggest that educational workshops could have important benefits for treating migraines, pending replication in a more rigorously designed large-scale study. (Military Medicine, Feb. 6, 2018)
>
|
Steroid drug may help PTSD symptoms
 Photo ©iStock/adventtr (02/27/2018)
The drug dexamethasone improved PTSD symptoms when paired with trauma memory activation, in a VA North Texas Health Care System study. Dexamethasone is a glucocorticoid—a type of steroid involved in glucose metabolism and the immune system. It is commonly used to treat a number of conditions, such as rheumatoid arthritis, allergies, and asthma, because of its anti-inflammatory properties. Fifty-four male Veterans with PTSD received either dexamethasone or placebo. The first group was given the drug while doing a trauma memory reactivation task in four weekly sessions. Those treated with the drug had significantly lower PTSD symptoms at one- and three-month follow-ups. They also had lower symptoms six months later, but the results were no longer significant relative to the placebo group. The drug is thought to facilitate the extinction of fear memories—meaning that the memory is replaced with new learning. Extinction is impaired in people with PTSD. The drug has an “excellent high-dose safety profile,” according to the researchers, although it could have side effects such as increased appetite, insomnia, heartburn, and muscle weakness, and increased blood sugar. One study participant was hospitalized because of leg swelling that possibly resulted from the drug. Further trials are needed to explore the drug’s potential role in PTSD treatment, say the researchers. (Psychiatry, Winter 2017)
|
Non-specialists do as well as specialists at treating sleep apnea
 Photo:©iStock/Nicolesy (02/22/2018)
Patients with obstructive sleep apnea receive similar quality of care from sleep specialist physicians and non-sleep specialists, found a Minneapolis VA Health Care System review. Four studies found that sleep specialist physicians and non-sleep specialists performed equally well at diagnosing obstructive sleep apnea and classifying its severity. Eight other studies showed that patients with both types of providers had similar quality of life, adherence to treatment, and symptom scores. Using dedicated sleep specialist physicians can be expensive and inefficient. The researchers believe that more research is needed on the best and most efficient care models for sleep apnea. (Annals of Internal Medicine, Feb. 6, 2018)
|
Review study finds antipsychotic drug a ‘reasonable treatment’ for PTSD
 Photo:©iStock/Hailshadow (02/22/2018)
A review study by a team at the Durham VA Health Care System concluded that aripiprazole is a reasonable treatment option for PTSD. Aripiprazole, sold as Abilify and other brands, is an atypical antipsychotic mainly used to treat schizophrenia and bipolar disorder. Current VA and Department of Defense guidelines recommend against this class of drugs for PTSD, although in the case of aripiprazole the evidence against its use is considered weak. Looking at six previous studies, the Durham researchers found that patients on aripiprozole showed significant improvements in PTSD symptoms. The drug was well-tolerated, although there were some adverse effects such as anxiety and insomnia. These side effects are themselves symptoms of PTSD, but most study participants experienced fewer symptoms overall. The researchers acknowledge that psychotherapy has been shown to be the best treatment for PTSD, but that since some patients either decline or are unable to participate in talk therapy, other approaches should be explored. Larger studies are needed to better understand how antipsychotics can be used to treat patients with PTSD, say the researchers. (Clinical Neuropharmacology, November/December 2017)
|
Rates of hospital admission after VA outpatient surgery
 Photo:©iStock/Rpsycho (02/22/2018)
As many as 20 percent of VA outpatient surgeries result in hospital admission, according to a VA Boston Healthcare System study. This admission rate is higher than in non-VA settings—which average around 1 to 5 percent—but may be explained by the greater disease burden and higher percentage of men seen in VA, say the researchers. They looked at data from 63,685 surgeries carried out between 2011 and 2013. They found that 66 percent of hospital admissions occurred on the day of surgery. Admission rates ranged from 5 percent in podiatry surgeries to 28 percent in urology. Four percent of admissions were for surgical complications. Regardless of type of surgery, higher procedure complexity and anesthesia risk led to more admissions. The admission rate may appear higher because of planned inpatient stays being miscoded as outpatient procedures that resulted in hospitalizations, noted the researchers. Also, VA providers may also be more likely than private doctors to hold patients for observation or choose to readmit them after a surgery because the patients would not incur an additional cost for this choice. The researchers conclude that most postoperative admissions are likely observational, and not because of problems related to the surgery. (Health Services Research, Jan. 23, 2018)
|
Natural language processing accurate at analyzing bladder cancer reports
 Photo: Wikimedia Commons (02/15/2018)
Natural language processing was successful at identifying details on patients with bladder cancer from medical reports. Researchers analyzed 600 reports on patients with bladder cancer from the VA's Corporate Data Warehouse using a computer engine that looks at language. They used this set of reports to develop and evaluate the computer program. Researchers then applied the natural language processing engine to more than 10,000 other reports. The program was able to accurately detect pathologic characteristics—such as tumor structure, depth, and grade—in 99 percent of patients. This technology could be used to group cancer patients together by similar characteristics for future studies. (Urology, December 2017)
|
Protein related to migraine may not be as important to blood pressure regulation as previously thought
 Photo: ©iStock/laflor (02/15/2018)
A central nervous system protein believed to prevent high blood pressure can possibly be blocked without negative cardiovascular effects, according to an Iowa City VA Medical Center and University of Iowa study. The protein, calcitonin gene-related peptide (CGRP), can cause migraines, but it has also been shown to protect against high blood pressure. Researchers treated mice with gene variations that resulted in increased CGRP receptors with drugs that increase blood pressure. The results suggest that the receptors themselves may provide cardiovascular protection even without directly interacting with CGRP. This could mean that migraine medications that block CGRP activity may not pose a risk of causing high blood pressure, as previously thought. (Journal of Cerebral Blood Flow and Metabolism, Jan. 1, 2018)
|
Insomnia drug may be overprescribed to Veterans
 Photo: ©iStock/OcusFocus (02/15/2018)
Prescription of zolpidem (sold as Ambien and other brands), an insomnia drug, is more widespread than guidelines recommend in Iraq and Afghanistan Veterans, found a study by researchers from several VA systems. Researchers looked at nearly 500,000 Veterans who received VA care in 2013 and 2014. Zolpidem was prescribed to 7.6 percent. The majority of these Veterans had long-term use of zolpidem, averaging 189.3 days. These numbers may reflect high-risk zolpidem prescribing practices that put Iraq and Afghanistan Veterans at risk for adverse effects and poor health outcomes, say the researchers. They believe the findings could serve as a guide to help improve prescribing of the drug. (PLoS ONE, Jan. 23, 2018)
|
Preterm birth more common in six months after deployment
 Photo: ©Stock/Ondroo (02/08/2018)
Women soldiers who gave birth within six months of returning from deployment were more likely to deliver early, according to a study including a VA Palo Alto Health Care System researcher. The rate of preterm birth was nearly double for women who delivered within six month of returning, compared with births at other times. Neither multiple past deployments nor PTSD was linked to preterm birth. The results show a need for increased focus on pregnancy timing for service women, as well as access to pre-deployment reproductive counseling and contraception, say the researchers. (American Journal of Epidemiology, Jan. 12, 2018)
|
Opioid prescription in VA has declined
 Photo: ©Stock/fluxfoto (02/08/2018)
Opioid prescribing has declined in VA in recent years, found an Iowa City VA Healthcare System study. Researchers looked at data on opioid use in VA between 2010 and 2016. Opioid prescriptions peaked in 2012 at 21.2 percent of all VA patients receiving at least one outpatient prescription. The rate then declined annually to 16.1 percent in 2016. The decline is mostly because of less long-term opioid prescribing, as opposed to short or intermediary opioid use. The results show that recent VA opioid initiatives may be succeeding in preventing patients from beginning long-term opioid use. (Journal of General Internal Medicine, Jan. 29, 2018)
iStock-172960226.jpg
|
Transition-related treatment curbs suicidal thoughts, depression in transgender Veterans
 Photo: ©Stock/portishead1 (02/08/2018)
Transgender people who had undergone transition-related medical interventions were less likely to have suicidal thoughts and symptoms of depression, in a study of transgender Veterans. People who had both hormone therapy and surgery on the chest and genitals had significantly lower levels of suicidal thoughts and depression, compared with those who had no medical intervention, hormone therapy only, or hormone therapy and surgery on either the chest or genitals but not both. Results suggest that combined medical treatment to affirm one's gender identity has a protective psychological effect, according to the researchers. VA currently provides certain transition services for transgender Veterans, such as counseling, evaluations, and hormone therapy, but does not provide nor pay for surgery. (Psychological Medicine, Jan. 14, 2018)
|
New scale measures moral injury
 Photo for illustrative purposes only. ©iStock/kieferpix (02/02/2018)
Researchers from multiple VA centers and their colleagues have developed a scale to measure moral injury in Veterans and service members with PTSD. Moral injury includes feelings of guilt, shame, moral concerns, religious struggles, loss of religious faith, loss of meaning or purpose, difficulty forgiving, loss of trust, and self-condemnation. Researchers tested the Moral Injury Symptom Scale-Military Version (MISS-M) with 427 Veterans and service members with PTSD symptoms. They found high correlation between scores on the 45-item MISS-M survey and PTSD symptoms. The MISS-M could be a useful tool to measure moral injury and identify those at risk for PTSD, say the researchers. (Journal of Religion and Health, February 2018)
|
Memory tests are accurate for diagnosing Alzheimer's
 Photo: ©iStock/marrio31 (02/02/2018)
Memory tests are able to differentiate between those with and without Alzheimer's disease, found a review by researchers from several VA systems. In the 47 studies included by the researchers, measures of immediate and delayed memory had high diagnostic accuracy for Alzheimer's. Memory tests had lower accuracy for diagnosing mild cognitive impairment, based on 38 studies. While memory tests and other psychological testing can be useful for diagnosing Alzheimer's and other cognitive deficits, they are not required in the current diagnosis criteria. The researchers suggest that these tests should be emphasized when diagnosing the conditions. (Neuropsychology Review, December 2017)
|
Heart procedures in VA versus community hospitals
 Photo ©iStock/KentWeakley (02/02/2018)
Performing coronary revascularization procedures at community care hospitals that partner with VA, rather than at VA hospitals, has benefits and downsides, according to a study in several VA health care systems. Coronary revascularization refers to procedures to treat artery narrowing or blockage near the heart. The procedures studied were percutaneous coronary intervention and coronary artery bypass graft. One in five elective coronary revascularizations for VA patients was performed at community care sites that were part of the VA Community Care Program. Patients who had percutaneous coronary interventions at community-based medical centers had shorter travel distances than their peers who had the procedure at VA hospitals. However, community care patients had higher mortality and higher costs to the health care system than VA hospital patients. Coronary artery bypass grafts performed at community care hospitals had shorter travel distance, similar mortality, and lower costs than those performed at VA hospitals. The results show that patients should be provided with information to help them pick the health care professionals best for them regardless of location, say the researchers. (JAMA Cardiology, Jan. 3, 2018)
|
Mouse model of PTSD sleep disturbances
 Photo ©iStock/D-Keine (02/02/2018)
Researchers at the Harry S. Truman Memorial Veterans Hospital have found a technique that may let them study sleep disruptions from PTSD by using mice. The researchers exposed mice to soiled cat litter. The smell caused predator odor trauma in the mice, which caused hyperarousal and memory effects related to fear. By studying electrical signals in the mouse brains, researchers concluded that the sleep disturbances caused by predator odor trauma mimic sleep disturbances in humans with PTSD. The results could allow scientists to study PTSD-related sleep disturbances without using human study volunteers. (Sleep, Jan. 13, 2018)
|
'Nanoshuttle' capable of delivering drugs to specific tissue
 Image from Bone Research via Creative Commons (01/25/2018)
A team including a VA San Diego Healthcare System researcher designed "nanoshuttles" capable of delivering cancer drug molecules to specific cells and tissue. The nanoshuttles are tiny silica structures shaped like golf balls and containing gold and iron oxide nanoparticles. Researchers were able to guide these nanoshuttles through simulated blood vessels and human tissue by using an exterior magnetic field. The nanoshuttle is coated with a polymer sensitive to heat and pH, allowing the researchers to control when the payload, a cancer drug, is released. This technique holds great potential to deliver drugs to specific tissue types, say the researchers. (Bone Research, Dec. 20, 2017)
|
Evidence lacking on ways to prevent late-life cognitive decline
 Photo: ©iStock/PeopleImages (01/25/2018)
No proven methods exist to prevent cognitive decline in late life, according to a series of four reviews by Minneapolis VA Health Care System researchers.
A review of studies on multiple over-the-counter supplements did not find evidence that supplements protect against cognitive impairment or dementia. Daily folic acid plus vitamin B12 was linked to memory improvements, but the clinical significance was questionable. Evidence showed that vitamin E had no benefit on cognition. Existing evidence on a variety of other supplements is either low strength or insufficient.
Another review did not find much evidence that short-term physical activity prevented cognitive decline or dementia in older adults. Not enough evidence exists on the effectiveness of aerobics, resistance training, or tai chi. Low-strength evidence did suggest that physical activity, diet, and cognitive training together improved cognitive performance.
A third review did not find evidence to support the use of prescription drugs to protect against cognitive decline. NSAIDs, statins, high blood pressure medications, and cholinesterase inhibitors did not reduce dementia risk or slow cognitive decline. Evidence suggests that estrogen and estrogen-progestin increased the risk of dementia or cognitive impairment. High-dose raloxifene, an osteoporosis drug, decreased mild cognitive impairment but not dementia risk, but the strength of the evidence was low.
The final review did not find sufficient evidence that cognitive training could prevent dementia. Training in a specific area improved performance in that area only—for example, memory training improved memory, but not overall cognition. While cognitive training shows some benefit, not enough evidence exists to say whether these benefits actually prevent or delay cognitive decline or dementia. (Annals of Internal Medicine, Jan. 2, 2018)
|
General satisfaction with VA health care high, but some areas need improvement
 Photo by Mitch Mirkin (01/25/2018)
A diverse, multisite survey found generally high levels of satisfaction with VA health care. Researchers interviewed 1,222 Veterans at multiple VA locations between 2013 and 2015. They found that overall satisfaction with VA care was comparable or better than in other health care systems. No clear patterns in satisfaction were evident based on race or gender. Between 74 and 76 percent of participants said they were "very satisfied" with VA costs, outpatient facilities, and pharmacy services. Satisfaction was lowest with access to care, pain management, and mental health care, with 21 to 24 percent responding they were "less than satisfied." While satisfaction levels with VA health care were generally high, there is room for improvement, conclude the researchers. Since the time of the interviews, VA has made efforts to improve access to care, meaning that the results may not reflect current levels of satisfaction. (Journal of General Internal Medicine, Jan. 8, 2018)
|
VA system barriers could lead to lack of engagement with psychotherapy
 Photo for illustrative purposes only. ©iStock/Vadimguzhva (01/18/2018)
In a study based at one South Central VA Health Care Network clinic, system-level barriers were the most common reason cited by patients who had chosen to not engage with PTSD psychotherapy. Researchers interviewed 24 patients who had been prescribed either cognitive processing or prolonged exposure therapy for PTSD but who did not attend any sessions. Two-thirds of those interviewed mentioned barriers related to the VA system. These included inefficiencies and delays, negative experiences with VA staff and providers, discomfort with the VA environment, and difficulty navigating the VA system. Most Veterans interviewed said they had multiple barriers to treatment engagement. The researchers point out that the study may not provide a full picture of VA consumer satisfaction, since it included only Veterans who had opted out of therapy. But they say the results nonetheless underscore the need for a more patient-centered model of care. (Psychological Services, Dec. 21, 2017)
|
VA and Medicare Part D dual users more likely to take high opioid doses
 Photo: ©iStock/Darwin Brandis (01/18/2018)
Veterans using both VA and Medicare Part D for prescriptions were at a two to three times higher risk of high-dose opioid exposure than those only using one system, according to a study by VA Pittsburgh Healthcare System researchers and their colleagues. They found that 13 percent of patients who filled at least one opioid prescription in 2012 received care from both VA and Medicare Part D. Dual-use patients were more likely to receive high opioid doses and to have long-term high dose use. The researchers acknowledge that the data, which were the latest available at the time of the study, may not reflect the current state of opioid use across VA and Medicare. At the same time, they say that as VA adopts more community care options, the findings may take on even greater relevance. (American Journal of Public Health, February 2018)
|
Chiropractic care improves low back pain for some female Veterans
 Photo: ©iStock/CheshireCat (01/18/2018)
Chiropractic care improved outcomes for some female Veterans with low back pain, in a VA Western New York Healthcare System study. After an average of eight chiropractic treatments, women saw an average of 27 percent improvement in pain, based on a back pain questionnaire. About 47 percent of patients met the minimum clinically important difference to show the treatment is effective. While not all women studied saw statistically important improvements, the researchers concluded that chiropractic care may be of value for pain management in this population. (Journal of Manipulative and Physiological Therapeutics, October 2017)
|
Psychological risk factor difference in returning Veterans based on gender
 Photo by Master Sgt. Mark C. Olsen (01/10/2018)
Researchers with the Edith Nourse Rogers Memorial Veterans Hospital and their colleagues examined the different challenges for men and women Veterans returning from deployment. They looked at 283 post-9/11 returning combat Veterans to see how psychological risk factors differed based on gender. Results showed that female Veterans were more likely to report a history of sexual trauma. Male Veterans had a greater frequency of gambling, impulsivity, and hypersexuality. Both men and women had similar rates of depression, anxiety, insomnia, and substance use disorder. Veterans had higher rates of these conditions than non-Veterans, regardless of gender. Further research should focus on how these differences impact reintegration and functioning, say the researchers. (Journal of Interpersonal Violence, Dec. 12, 2017)
|
Report: People with PTSD have a smaller hippocampus
 Photo: ©iStock/yodiyim (01/10/2018)
People with PTSD have smaller hippocampi than those without, according to a large international consortium including several VA researchers. The study looked at 1,868 subjects who had been exposed to trauma, 794 of whom had active PTSD. Those with PTSD had significantly lower hippocampus volume than those without. The hippocampus is a section of the brain associated with emotions and long-term memory. Subjects with PTSD also had smaller amygdalae, but that finding was not deemed significant after statistical analysis. The results add support to previous findings that trauma exposure may cause volume loss in the hippocampus. The researchers describe the results as an important milestone in understanding the brain's response to trauma. (Biological Psychiatry, Feb. 1, 2018)
|
Telephone versus televideo for genetic counseling
 Photo: ©iStock/shironosov (01/10/2018)
Both telephone and televideo delivery of genetic counseling have strengths and weaknesses, found a study by researchers from three VA medical centers. Researchers surveyed 20 patients receiving genetic counseling by phone and 18 receiving it by televideo, along with their counselors. Patients and counselors were satisfied with both methods. Televideo required more travel time and expense than telephone because it must be conducted at a clinic. Patients liked the flexibility of telephone. However, counselors felt that patients missed more appointments and were distracted when using the telephone. Televideo also had the advantage of letting counselors read the body language of patients. The results show that further analysis of telehealth methods is needed to balance access to care with patient engagement, according to the researchers. (Journal of Genetic Counseling, Dec. 15, 2017)
|
No-touch disinfection effective in preventing some hospital infections, but not others
 Photo courtesy of xenex.com (01/04/2018)
No-touch disinfection methods are effective at preventing some common infections but not others, found a literature review by a team including an Iowa City VA Health Care System researcher. The researchers looked at studies on ultraviolet light or hydrogen peroxide vapor cleaning systems. They found that these techniques significantly reduced C. difficile and vancomycin-resistant enterococci infection, two antibiotic-resistant pathogens common in hospitals. They did not find differences in the infection rates for MRSA or other drug-resistant organisms for no-touch techniques versus manual cleaning alone. The authors believe that no-touch cleaning methods can augment traditional cleaning, but not replace it. (Infection Control & Hospital Epidemiology, Nov. 16, 2017)
|
COPD tied to cognitive impairment, although causation not clear
 Photo: ©iStock/ands456 (01/04/2018)
Patients with chronic obstructive pulmonary disease have a high prevalence of cognitive impairment, according to a review by Central Arkansas Veterans Healthcare System and University of Arkansas researchers. Looking at the available literature, the researchers found that older patients with COPD were more likely to have mild cognitive impairment and dementia than those without COPD. Newer studies have reported that oxygen therapy and pulmonary rehabilitation can have positive effects on cognitive impairment. There is some evidence that the severity of low oxygen levels is linked to the severity of cognitive dysfunction. However, the researchers caution that causality between the two cannot be drawn from the available data. (Current Opinion in Pulmonary Medicine, Dec. 9, 2017)
|
Effect of testosterone on cardiovascular risk remain unclear
 Photo for illustrative purposes only. ©iStock/Halfpoint (01/04/2018)
Results were mixed on whether treatment for low testosterone in older men improves cardiovascular risk factors, in a study that included several VA researchers. The researchers looked at how testosterone treatment affects cardiovascular risk factors in 788 men age 65 or older. The study was part of a larger series of trials looking at how testosterone therapy affects a number of health outcomes. Testosterone was linked to small reductions in cholesterol and fasting insulin. But testosterone therapy did not affect other cardiovascular risk factors, such as glucose markers, inflammation, or clotting. More large studies are needed to figure out what effect testosterone has on cardiovascular risk, say the researchers. (Journal of Clinical Endocrinology and Metabolism, Dec. 14, 2017)
|
Military-related trauma linked to eating disorders in male Veterans
 Photo for illustrative purposes only. ©iStock/domoyega (12/27/2017)
Military-related trauma was linked to eating disorder symptom severity in male Veterans, in a study by VA Boston Healthcare System researchers. Of a group of 642 male Veterans, 4 percent showed a probable eating disorder. Up to 3 percent of men in the general population have an eating disorder. The most common symptom in the study group was binge eating, which is also the most common for men in the general population. Symptoms were more common for those who had experienced military-related trauma, with multiple traumas linked to increased eating disorder symptoms. Military-related trauma was defined in the study as “seeing something horrible or being badly scared” during military service. Interestingly, only non-combat military trauma was linked to eating disorders. Similar results have been seen in female Veterans, but eating disorders are understudied in men. Previous studies have shown as much as 14 percent of women Veterans may have eating disorder symptoms. Non-military trauma, such as childhood trauma, was not shown to be linked to eating disorders in the study group. The researchers say better assessment of eating disorders in male Veterans is needed. (International Journal of Eating Disorders, November 2017)
|
Antibiotic timing off for many dental procedures
 Photo: ©iStock/domoyega (12/27/2017)
While most patients in a small one-site VA study received antibiotics when having a dental procedure, most did not receive them at the right time. Guidelines now recommend that a single course of antibiotics be given before tooth extractions, dental implants, and periodontal procedures. Of 183 Veterans having a dental procedure, 83 percent received antibiotics. Of those, 92 percent received antibiotics only after the procedure. Only 3 percent received antibiotics before the procedure, with 5 percent receiving antibiotics both before and after. The researchers conclude that more efforts are needed to ensure proper timing of antibiotic treatment in dental practices. (Open Forum Infectious Diseases, Nov. 15, 2017)
|
Medical marijuana and opioid misuse may be linked
 Photo: ©iStock/LPETTET (12/27/2017)
Medical marijuana use may be linked to risk of prescription opioid misuse, according to a study by VA Portland Health Care System and Kaiser Permanente researchers. They studied 371 patients on long-term opioid therapy. Eighteen percent of those patients also used medical marijuana for pain. Those who used medical marijuana were significantly more likely to be at risk for prescription opioid misuse. The study showed no significant differences between those who used marijuana and those who did not in terms of pain relief, depression, or anxiety. The results highlight the need for more research on the long-term impact of medical marijuana, according to the researchers. (General Hospital Psychiatry, Nov. 8, 2017)
|
New cholesterol drug not cost-effective
 Photo: ©iStock/jamesbenet (12/14/2017)
Adding a PCSK9 inhibitor to statin therapy for high cholesterol is not cost-effective, found a study including a Michael E. DeBakey VA Medical Center researcher. PCSK9 inhibitors have been available since 2015, but are not widely used because of the cost and the newness of the drug class. Using a statistical model for a theoretical group of patients, based on the existing medical literature, the researchers determined that adding a PCSK9 inhibitor drug to a statin would typically reduce LDL cholesterol by 59 percent, and adverse cardiovascular events (such as stroke and heart attack) by 15 percent per year. However, the drug is very expensive: $14,300 per year. This price equates to a cost of almost $500,000 per quality-adjusted life year, an economic measure of disease burden that takes quality of life into account. The normal cost the market is willing to pay per quality-adjusted life year is $100,000. The price of PCSK9 would need to be lowered by 62 to 83 percent to become cost-effective, according to the researchers. (JAMA Cardiology, Oct. 18, 2017)
|
Protein shown to suppress breast cancer growth in mice
 Photo: ©iStock/dra_schwartz (12/14/2017)
A protein known as GPER1 suppressed the growth of breast cancer cells in a U.S. and Chinese study that included an Omaha VA Medical Center researcher. Prolonged exposure to estrogen is a risk factor in the progression of breast cancer. GPER1 has been shown to control how estrogen affects certain genes. The researchers looked at how the protein reacted in both human cells and mouse models. They found that GPER1 proteins bind to certain gene sites, disrupting cancer cell division and growth. Injection of GPER1 into mice did not harm their biology or behavior. The results suggest this protein could be a promising chemotherapy drug to treat breast cancer. (Molecular Cancer Therapeutics, June 2017)
|
Mandibular advancement device offers viable alternative to CPAP
 Photo: ©iStock/cherrybeans (12/14/2017)
Mandibular advancement devices (MAD) may be a good alternative to CPAP for treating obstructive sleep apnea in Veterans with PTSD, according to a VA Western New York Healthcare System study. A MAD is a mouth guard that holds the lower jaw and tongue forward, creating more breathing space during sleeping. Continuous positive airway pressure (CPAP) therapy involves a machine and breathing mask that creates pressure to keep the airway open. Researchers tested 35 subjects with both treatments. Results showed that CPAP provided better breathing results during sleep. However, both treatments improved sleep apnea and PTSD symptoms over no treatment. While CPAP is more effective than MADs, patients are much more likely to use a MAD consistently than they are CPAP, especially patients with PTSD. Patients used the MAD an average of 2.2 hours longer per night than CPAP. Fifty-eight percent of participants preferred the MAD to CPAP, while only 29 percent preferred CPAP. (Journal of Clinical Sleep Medicine, Nov. 15, 2017)
|
VA responsive to FDA drug warning on antidepressant, but less so for older patients
 Photo: ©iStock/Cecile_Arcurs (12/08/2017)
VA prescription of high doses of a common antidepressant decreased after FDA safety warnings, but not for all patient groups, found a VA Ann Arbor Healthcare System study. The FDA issued warnings against high doses of the antidepressant citalopram (sold as Celexa) in 2011 and 2012. Within the VA health system, high-dose citalopram use decreased by 2 percent per month between the first warning in 2011 and second in 2012. Less than 3 percent of citalopram users were on a high dose after both warnings. However, about 31 percent of older patients remained on doses higher than the new recommendation. Lower citalopram use was accompanied by significant increases in prescription of alternative antidepressants. While the results suggest that notification systems used in VA enable a quick response to medication warnings, more research is needed on how facilities receive and respond to these warnings, say the researchers. (American Journal of Geriatric Psychiatry, September 2017)
|
Telehealth management program may lower burden for dementia caregivers
 Photo: ©iStock/Thomas_EyeDesign (12/08/2017)
A telephone-based dementia care management program led to reduced burden on caregivers, found a study involving several VA centers. Home caregivers of patients with dementia participated in a telehealth education program. Participants engaged in two to three contacts per month for three months. They completed modules on dementia-related behavior management strategies and caregiver coping techniques. Participants in the telephone learning program showed lower burden, compared with those who received standard clinical care. The telehealth group also showed lower frequency of dementia-related behaviors and caregiver distress in response to these symptoms. The results suggest that a care management program delivered by telephone can improve outcomes for both patients with dementia and their caregivers. (American Journal of Geriatric Psychiatry, September 2017)
|
Variations in performance on cognitive tests may foretell Alzheimer's
 Photo: ©iStock/solidcolours (12/08/2017)
Cognitive tests may be effective in predicting Alzheimer's disease, found a study including William S. Middleton Memorial Veterans Hospital researchers. The researchers looked at biomarker and cognitive test data gathered over six years from 349 patients. They found that performance on cognitive tests lined up with biomarkers from lumbar punctures in predicting the advance of Alzheimer's disease and mild cognitive impairment. Specifically, the participants at risk were those who performed unevenly across tests in different cognitive areas, such as executive functioning, attention, verbal learning, memory, and reading. Such tests may pose an alternative to invasive medical procedures for prediction or early detection of the disease, according to the researchers. (Journal of Alzheimer's Disease, 2018)
|
New tool to predict mortality of dialysis patients
 Photo: ©iStock/porpeller (12/08/2017)
VA and Kaiser Permanente researchers have developed a new risk prediction tool for patients transitioning to dialysis. The researchers looked at demographics, renal disease causes, other conditions, and lab data for more than 35,000 Veterans who transitioned to dialysis over a 6.5-year period. Twenty-seven percent died within a year of beginning dialysis. Researchers predicted about that number of deaths based on the data. They validated the prediction tool by looking at more than 4,000 patients outside VA. This new tool could help identify high-risk patients and aid in dialysis planning, say the researchers. (American Society of Nephrology Kidney Week, Nov. 3, 2017)
|
Study links genes to suicide-attempt risk
 Photo: ©iStock/nicolas (11/30/2017)
A team including several VA researchers has identified a gene variation that may be linked to risk of suicide attempts. The researchers studied the mapped genomes of a large group of soldiers to look for similarities in those who had attempted suicide. They found similar variation in two genes in one genome location. The genes (CEP162 and MRAP2) are involved in how the body uses the energy it gets from food. The results suggest that this gene variation may increase the risk of suicide, according to the researchers. The results may also show a genetic link between risk of suicide and bipolar disorder, they say. (American Journal of Medical Genetics, December 2017)
|
Genetic markers of schizophrenia predict lithium nonresponse in bipolar disorder
 Photo: ©iStock/Morrhigan (11/30/2017)
Patients with bipolar disorder who also have a high genetic risk for schizophrenia do not respond as well to lithium treatment as those without schizophrenia markers, found a large, international consortium including several VA researchers. Lithium is the standard mood stabilizer used to treat bipolar disorder. However, up to 30 percent of patients do not respond to lithium. The researchers looked at the genomes of more than 2,000 patients with bipolar disorder. They found that patients who had gene variations that have previously been shown to predict schizophrenia also did not respond to lithium for bipolar disorder. The results could be used to predict how effective lithium treatment will be for individual patients, say the researchers. (JAMA Psychiatry, Nov. 9, 2017)
|
Program will match cancer patients with clinical trials
 Photo: ©iStock/RoBeDeRo (11/30/2017)
Researchers with the VA Boston Healthcare System have created an online system to match cancer patients with clinical trials. The researchers partnered with a team at the University of California, San Francisco to adapt their CTMatch application to VA patients with non-small cell lung cancer. The system is part of the Precision Oncology Program, a VA program that offers genomic analysis of patients with tumors. The researchers hope that the system will lead to better treatments for patients by matching them with the most relevant clinical trials. (American Medical Informatics Association Annual Symposium, Nov. 7, 2017)
|
Trend toward earlier hospice enrollment in VA
 Photo: ©iStock/Martin Prescott (11/21/2017)
Early hospice enrollment increased over time in the VA health care system for patients with advanced-stage lung cancer, found VA Portland Health Care System researchers and their colleagues. Early enrollment in hospice can improve quality of care and caregiver well-being, according to the researchers. They looked at data from nearly 22,000 patients diagnosed with lung cancer between 2007 and 2013. Seventy percent of patients were enrolled in hospice. Of those, 53 percent were enrolled in the last month of life, while 15 percent were enrolled in the last three days. Over the time period studied, hospice enrollment increased. Time between diagnosis and hospice enrollment decreased. This trend toward timely hospice enrollment is encouraging, say the researchers. They also note that regional variability in hospice enrollment suggests room for improvement. (Cancer, Oct. 10, 2017)
|
RNA markers altered in rheumatoid arthritis
 Photo: ©iStock/selvanegra (11/21/2017)
Small RNA segments are altered in people with rheumatoid arthritis, found a VA Tennessee Valley Healthcare System study. Small, noncoding RNA segments within human genes regulate biological processes. Researchers looked at the RNA variations in blood plasma of people with rheumatoid arthritis. They found significant alteration in 12 RNA sequences, compared with subjects without arthritis. The results could be used to help diagnose rheumatoid arthritis, say the researchers. (American College of Rheumatology Annual Meeting, Nov. 6, 2017)
|
For back pain, telehealth cognitive behavioral therapy matches in-person treatment
 Photo: ©iStock/fstop123 (11/21/2017)
Cognitive behavioral therapy for low back pain delivered by phone had similar results to in-person treatment, in a study by VA San Diego Healthcare System researchers. Patients with chronic low back pain participated in eight weeks of either cognitive behavioral therapy over the phone or in-person supportive care. Both groups showed similar levels of pain improvement. Both also had strong participation. The results show that telehealth approaches to psychotherapy could be useful in treating pain. (Clinical Journal of Pain, Sept. 1, 2017)
|
Exploring the risks of sexual assault for deployed versus non-deployed servicewomen
 Photo by Sgt. Richard Blumenstein/USMC (11/21/2017)
Researchers from the Iowa City VA Health Care System and their colleagues looked at the rates of sexual assault against servicewomen who were deployed, versus those who were not deployed. Of more than 1,000 women surveyed who served during the wars in Iraq and Afghanistan, 16 percent had experienced sexual assault in the military. More servicewomen experienced sexual assault while not deployed. However, after adjusting for time spent in each setting, the researchers found that women were at greater risk of sexual assault during deployment. The results suggest that both locations require unique strategies to reduce sexual assault, say the researchers. (American Journal of Industrial Medicine, November 2017)
|
Computer algorithms accurately identify fatty liver disease
 Photo: ©iStock/choja (11/16/2017)
Researchers at the Michael E. Debakey VA Medical Center and their colleagues have developed computer algorithms that can accurately identify fatty liver disease from radiology reports. The algorithms use natural language processing to "read" text reports from radiology tests. They were able to identify patients with fatty liver disease more than 90 percent of the time. The algorithms could be used to rapidly screen patient records to gather data for studies on the disease, say the researchers. (Digestive Diseases and Sciences, October 2017)
|
Electronic trigger detects mammogram follow-up delays
 Photo: ©iStock/thomasandreas (11/16/2017)
An electronic trigger was effective at detecting delayed follow-up after an abnormal mammogram result, found Michael E. DeBakey VA Medical Center researchers. The researchers used a computer algorithm to search electronic health records for abnormal mammogram results with no noted follow-up. Looking at more than 2,000 records, the algorithm had 71 percent accuracy for detecting follow-up delays. The results suggest that electronic triggers could help track and reduce missed opportunities to act early for treatment, according to the researchers. The results also show that delayed follow-ups continue to be a problem for some despite federal laws requiring patient notification of mammogram results within 30 days, they say. (Journal of the American College of Radiology, Nov. 1, 2017)
|
Window of Hope therapy is effective at reducing hopelessness in people with TBI
 Photo for illustrative purposes only. ©iStock/KatarzynaBialasiewicz (11/16/2017)
The Window of Hope therapy program significantly reduced feelings of hopelessness in participants with traumatic brain injury, found a VA Rocky Mountain MIRECC study. Window of Hope is a cognitive behavioral therapy adapted for TBI. Hopelessness often occurs in people with TBI, sometimes leading to suicide. Those who participated in 10 weekly sessions scored significantly lower on a measure of hopelessness than those who did not. They continued to feel less hopeless three months after the therapy. The results show that the Window of Hope program is an effective way to treat hopelessness in this population, say the researchers. (Journal of Head Trauma Rehabilitation, Oct. 27, 2017)
|
Common fluids no better than saline for preventing kidney injury during angiograms
 Photo: ©iStock/kalus (11/16/2017)
Commonly used angiogram fluids are no better than saline at preventing kidney injury from the procedure, found a large international study funded by the VA Cooperative Studies Program and the National Health and Medical Research Council of Australia. Angiograms use a contrast solution containing iodine to illuminate blood vessels and organs for imaging. Intravenous sodium bicarbonate and oral N-acetylcysteine are commonly given during angiogram along with the contrast solution because they were thought to reduce the risk of kidney damage from the contrast. But the study of nearly 5,000 patients showed that these treatments were no better than a simple salt solution at preventing kidney injury. "The findings have implications every time someone with kidney disease in any hospital in the U.S. or worldwide undergoes angiograms," explains Dr. Steven Weisbord of the VA Pittsburgh Healthcare System, lead author on the paper. The results show that "saline solution alone should be the standard of care for the procedure," says Weisbord. (New England Journal of Medicine, Nov. 12, 2017)
|
Self-monitoring can lower blood pressure when used with other treatments
 Photo: ©iStock/mixetto (11/09/2017)
Self-monitoring leads to lower blood pressure when combined with other treatments, found a large international review including several VA researchers. The researchers analyzed 36 relevant articles on high blood pressure. They found that having patients monitor their own blood pressure on a regular basis at home resulted in reductions in pressure when combined with treatments such as medication, education, and lifestyle counseling. Self-monitoring by itself, however, did not lower blood pressure. The American Heart Association recommends self-monitoring at home for all those with high blood pressure, as the regular and frequent readings help providers track whether treatments are working. Based on the new study results, the researchers recommend including self-monitoring with other methods to treat high blood pressure. (PLoS Medicine, Sept. 19, 2017)
|
Blister packaging improves medication adherence
 Photo by Scott R. Galvin (11/09/2017)
Psychiatric patients are more likely to take their medications correctly when it is given in blister packaging, found a study by the Rocky Mountain Mental Illness Research, Education and Clinical Center at the Denver VA Medical Center. Blister packaging consists of individual doses of pills in plastic bubbles with a foil backing, similar to how cold medication is often packaged. Study participants who received blister packaging were 59 percent more likely to follow their medication instructions than those who received medication in standard pill bottles. The results suggest that using this kind of packaging could improve treatment outcomes for psychiatric patients, say the researchers. (Journal of Psychiatric Practice, September 2017)
|
Patients often overestimate activity level
 Photo: ©iStock/sdominick (11/09/2017)
Patients and their surrogates often largely overestimate activity level, according to a collaboration between VA and Australian researchers. The researchers asked patients admitted to the ICU or their surrogates to estimate how many steps they took each day prior to hospitalization. The researchers then used smartphone GPS and pedometer data to get objective numbers. Patients and surrogates overestimated the numbers of steps per day by more than 3,000. The results suggest that clinicians should be cautious when using subjective estimates of activity level, especially if they are using that information to plan treatment, say the researchers. (Critical Care Medicine, October 2017)
|
Transgender health care in VA and the military
 Photo courtesy of Bedford VAMC (11/02/2017)
Researchers from several VA health care systems reviewed the literature on the care received by transgender people in VA and the U.S. military. They found that more than 5,000 transgender Veterans receive care in VA. Little data exists on care of transgender active-duty service members, mostly because transgender individuals were not permitted to serve openly until June 2016. Transgender Veterans experience higher rates of both mental and physical health conditions than non-transgender Veterans, according to the review. VA and military facilities have increased access to health care for transgender Veterans and service members in recent years. However, the researchers caution that more studies about improving health outcomes for this group are needed. (Current Sexual Health Reports, September 2017)
[use image from Currents story on 9-6-17: Study: Majority of transgender Veterans satisfied with VA care]
|
Small, dense cholesterol particles linked to lower death risk
 Photo: ©iStock/designer491 (11/02/2017)
Patients with a pattern of small, dense LDL cholesterol particles had a lower risk of death after a heart attack than those with large, buoyant particles, found a study including a researcher from the Michael E. DeBakey VA Medical Center. Doctors have long known that higher LDL cholesterol levels can put people at risk for cardiovascular problems such as heart attack. In the new study, researchers found a 32 percent lower risk of death after a heart attack for patients with small, dense LDL particles in their blood stream, compared with patients with larger, buoyant particles. Despite the interesting findings, the researchers caution that more research is needed to figure out what causes this association. In the meantime, treatment after heart attack should continue to focus on lowering overall LDL cholesterol levels, they say. (Journal of Clinical Lipidology, Oct. 3, 2017)
|
Public attitudes on homelessness more compassionate than in the past
 Photo for illustrative purposes only. ©iStock/Photawa (11/02/2017)
Public attitudes and perceptions about homelessness have changed in recent years, according to a recent VA study. Researchers surveyed 541 adults in November 2016 and compared the results to surveys conducted in 1990. The more recent survey showed more compassion and liberal attitudes about homelessness than the older surveys. The largest changes were related to increased support for homeless individuals using public spaces for sleeping and panhandling. Survey participants overestimated the proportion of homeless people who are young and minorities. They underestimated the proportion who have mental or substance use problems. The increase public support for homeless individuals shown here presents new opportunities to address homelessness through legislation and public health initiatives, say the researchers. (American Journal of Community Psychology, Oct. 13, 2017)
|
Antibiotic group shown to be effective against drug-resistant bacteria
 Photo: ©iStock/adventtr (10/26/2017)
A VA St. Louis Health Care System team showed that a new group of antibiotics are effective against drug-resistant bacteria. The researchers tested 254 related antibiotic compounds, known as the nucleotidyltransferase superfamily, against a variety of common bacteria. They found multiple compounds to be effective at preventing the growth of drug-resistant bacteria, such as E. coli and Staphylococcus. The results show that this antibiotic group stops bacteria growth in a different way than existing antibiotics, according to the researchers. (ASM/ESCMID Conference on Drug Development to Meet the Challenge of Antimicrobial Resistance, Sept. 6, 2017)
|
Longevity gap for people with schizophrenia
 Photo: ©iStock/Mark_Hubsky (10/26/2017)
Mortality rates for people with schizophrenia have not gone down in recent years despite a decline in mortality rates in the general population, found a review by VA San Diego Healthcare System and University of California San Diego researchers. People with schizophrenia tend to have a 15–20 year shorter life expectancy than those without. Average life expectancy in developed countries, including the United States, increased from 72 years in the 1970s to 82 years in 2010. But this increase was not seen in the schizophrenic population. The study found that the gap in the mortality rate between people with schizophrenia and the general population increased by 37 percent from pre-1970s reports to post-1970s reports. The researchers suggest that this gap is caused by unmet health care needs stemming from the social stigma of mental illness, along with a lack of infrastructure and social support that leads to problems such as homelessness and incarceration for people with schizophrenia. The results suggest that major changes in mental health stigma, health care, and economic policy are urgently needed to improve medical care for people with schizophrenia, they say. (Schizophrenia Research, Sept. 27, 2017)
|
Family violence linked to higher risk of suicide attempt
 Photo: ©iStock/lolostock (10/26/2017)
Suicide attempts were higher in soldiers with a history of family violence, found an analysis of data from the Army STARRS study. According to the study, odds of a suicide attempt increased with the number of family violence events experienced. Soldiers who had experienced family violence in the past month were five times as likely to attempt suicide as those with no family violence history. Odds of a suicide attempt were higher for both violence perpetrators and victims. The results show that it is important to consider family violence when looking at the risk of suicide among soldiers, say the researchers. (Psychiatry Research, Sept. 20, 2017)
|
Mental disorders linked to suicidal behavior
 Photo for illustrative purposes only. ©iStock/Marjan_Apostolovic (10/26/2017)
A study of surveys given as part of the large Army STARRS study reinforced the idea that mental disorders are significantly associated with suicidal behavior. The researchers combined data from the All-Army Survey with two other Army STARRS study to get a large sample that included deployed soldiers and Army National Guard and Reserve troops. Previous studies on this topic using the All-Army Survey only looked at about 5,000 soldiers. This study used data from nearly 30,000 soldiers. Results revealed that all self-reported disorders tested for were associated with suicidal thoughts in both men and women. The surveys screened for major depressive episode, bipolar disorder, panic disorder, generalized anxiety disorder, PTSD, ADHD, intermittent explosive disorder, and substance use disorder. Disorders characterized by agitation and impulsiveness predicted a transition from suicidal thoughts to attempts in men. For both men and women, being in the regular Army (rather than National Guard or Army Reserve) was associated with greater risk. Being deployed and having a junior rank were also linked to higher risk of suicide attempts for men. (Suicide and Life Threatening Behavior, Sept. 19, 2017)
|
Lower-extremity neuroprostheses continue to function in the long term
 Photo: ©iStock/kali9 (10/04/2017)
Neuroprostheses to allow patients with spinal cord injuries to stand were still functioning and useful several years after being implanted, found a Louis Stokes Cleveland VA Medical Center research team. The researchers followed up with 22 patients with lower-extremity neuroprostheses an average of six years after they had the devices implanted. The neuroprostheses cause otherwise paralyzed muscles to contract by providing electrical impulses through implanted electrodes, allowing patients to stand. Being able to stand has many health benefits, such as improved circulation, bowel and bladder function, and digestion. Sixty percent of the patients still used their neuroprostheses for exercise and other activities for more than 10 minutes per day. First-generation implants still functioned correctly in 90 percent of patients with those devices. Second-generation implants (with slightly improved technology) still functioned in 98 percent of cases. Overall, 94 percent of the patients were satisfied with the prostheses. The findings suggest that implanted lower-extremity neuroprostheses can provide lasting benefits for patients, say the researchers. (Archives of Physical Medicine and Rehabilitation, Sept. 9, 2017)
|
Meditation could help with cardiovascular risk reduction
 Photo: ©iStock/PeopleImages (10/04/2017)
Meditation could reduce the risk of cardiovascular disease, according to a scientific statement from the American Heart Association. The AHA council, which included several VA researchers, reviewed more than 400 scientific articles on meditation. They found that meditation can have long-standing effects on the brain, which can in turn lower cardiovascular risk. Meditation may be able to help with cardiovascular risk factors such as stress, smoking, high blood pressure, and various metabolic functions. Meditation has low costs and low risks. This means it could be a useful addition to treatments for cardiovascular problems, say the researchers. However, they note that the quality of studies was only modest. More research is needed on meditation and cardiovascular risk, they say. (Journal of the American Heart Association, Sept. 28, 2017)
To find out more about VA research on mindfulness-based stress reduction (MBSR) read "Using mindfulness to combat stress-related heart disease in women Veterans."
Listen to Dr. Karen Saban, a VA researcher at Edward Hines, Jr. VA Hospital, as she discusses her work with MBSR.
|
Yoga could improve adverse effects of menopause
(10/04/2017)
Yoga may reduce vasomotor and psychological symptoms in women going through menopause, according to a Durham VA Medical Center and Duke University review. Vasomotor symptoms (e.g., hot flashes) are related to blood vessel dilation. Searching the available literature, the researchers found one review and three randomized controlled trials on yoga for treating menopause symptoms. The findings suggest practicing yoga reduced vasomotor symptoms and psychological symptoms such as anxiety and mood disturbances, say the researchers. However, they caution that more research with larger numbers and comparison groups is needed. (Complementary Therapies in Medicine, October 2017)
|
Three gene variants linked to Alzheimer’s disease
 Photo: ©iStock/malgorzata tatarynowicz (09/27/2017)
A large, international research group including several VA researchers identified three rare gene variants associated with late-onset Alzheimer’s disease. The researchers looked at the genetic maps of more than 85,000 subjects. They found coding variants of three genes (PLCG2, ABI3, and TREM2) to be associated with Alzheimer’s disease. All three genes are commonly expressed in microglia cells—a common cell type in the brain and spinal cord involved in the central nervous system’s immune defense. The results add evidence that the body’s immune response process is directly related to Alzheimer’s disease, according to the researchers. (Nature Genetics, September 2017)
|
CPAP use may improve sexual quality of life in women
 Photo: ©iStock/ viola83181 (09/27/2017)
Use of continuous positive airway pressure (CPAP) may improve sexual quality of life in women, found a VA Puget Sound Health Care System study. Sleep apnea often reduces sexual quality of life through reduced libido, reduced intimacy, erectile dysfunction, and other mechanisms. The researchers tested patients with newly diagnosed sleep apnea after 12 months of CPAP use, compared with controls who did not use CPAP. Women CPAP users showed improvement in sexual quality of life, but men did not. (American Academy of Otolaryngology–Head and Neck Surgery Annual Meeting, Sept. 12, 2017)
|
Sleep intervention shown effective for older adults
 Photo: ©iStock/bowdenimages (09/27/2017)
VA Greater Los Angeles Healthcare System and Durham VA Medical Center researchers found that a sleep intervention program improved sleep for older adults in an adult day health care program. Patients in the experiment group received four weekly sessions of the program, which included sleep compression (limiting time in bed to avoid lying awake), modified stimulus control (avoiding activities other than sleep, such as watching television, in bed), and sleep hygiene (e.g., limiting daytime naps and caffeine). Patients in the program improved on sleep efficiency, number of nighttime awakenings, and minutes awake at night, compared with a usual-care group. Some benefit remained four months after the program. The results suggest that a short behavioral sleep intervention could benefit older patients in day health care programs. (Sleep, Aug. 1, 2017)
|
Hip or knee replacement usually not followed by boost in physical activity
 Photo: ©iStock/eyenigelen (09/25/2017)
Most patients do not increase their physical activity levels after total hip or knee replacement, according to a literature review by a team that included a Durham VA Medical Center researcher. Patients often have large reductions in pain and increased physical function and quality of life after total hip or knee replacement. However, the researchers found no corresponding increases in physical activity after six months, and only modest increases after 12 months. The lack of physical activity may be behavioral, since a sedentary lifestyle is hard to change, say the researchers. (Arthritis Care & Research, Sept. 12, 2017)
|
More diabetic Medicare patients overtreated than undertreated
 Photo: ©iStock/andesr (09/25/2017)
More diabetic Medicare patients overtreated than undertreated
Medicare patients with diabetes are more likely to be overtreated than undertreated, found a Centers for Medicare and Medicaid Services and VA Health Services Research and Development Service study. The researchers studied data from more than 78,000 Medicare recipients with diabetes. They found that 11 percent were potentially overtreated for their diabetes. About 7 percent were potentially undertreated. Patients over 75 and those enrolled in Medicaid were more likely to be overtreated. Therapy was de-intensified for only 14 percent of overtreated diabetics. The results suggest that greater personalization of treatment would benefit patients with diabetes, say the researchers. (Journal of General Internal Medicine, Sept. 13, 2017)
|
Antiviral drugs could increase kidney transplant options for patients with hepatitis C
 Photo: ©iStock/pixologicstudio (09/25/2017)
Kidney transplants from deceased donors positive for hepatitis C antibodies could shorten transplant wait times for patients with hepatitis C when antiviral drugs are administered early, according to a Miami VA Healthcare System and University of Miami study. Patients with hepatitis C often need kidney transplants because the virus can cause renal disease. The researchers started 25 patients on direct-acting antiviral agents soon after they received kidney transplants from antibody-positive donors. The hepatitis C virus was not detected in the blood of 24 of the patients after 12 weeks. Transplants from donors with hepatitis C antibodies are not generally accepted because of risk of spreading the virus. But with new drugs that act directly on the virus, kidney transplants from these donors could decrease organ wait times and increase survival for patients with hepatitis C, say the researchers. (Transplant International, September 2017)
|
Study probes impact of stress on Coast Guardsmen’s mental health
 Coast Guard photo by Petty Officer 3rd Class Eric D. Woodall (09/11/2017)
Researchers with VA and other institutions assessed 241 active-duty Coast Guard members and found rates of posttraumatic stress disorder and depression comparable to those of the Army and other military services after deployment. The Coast Guardsmen in the study, a fifth of them female, were all serving at boat stations, which carry out operations such as search and rescue. The overall rate of PTSD was 15 percent. Nonmilitary trauma was twice as common as military trauma among those with the disorder. The overall rate of depression was 8 percent, with women at higher risk. Based on psychological tests, the researchers found that certain types of personalities predicted either PTSD or depression. They note that Coast Guard personnel have been understudied, relative to other military branches. The new study is the largest to date to look at Coast Guardsmen’s stress-related mental health symptoms. The researchers say the results are “provocative,” raising questions for future studies. They add that “accounting for personality could provide opportunities for early intervention.” (Frontiers in Psychology, Sept. 14, 2017)
|
Older women especially susceptible to blood pressure spikes during exercise
 Photo for illustrative purposes only. ©iStock/shironosov (09/11/2017)
When researchers conducted exercise tests with four groups of volunteers—younger men and women, average age 23; and older men and women, average age 73—they saw exaggerated increases in systolic blood pressure (the upper number in a blood pressure reading) only in the older women. On average, the systolic blood pressure of the older women rose 47 points, whereas in older men the increase was only 27 points. Among younger men and women, the increases were 25 and 22 points, respectively. The older women showed unique responses on other measures of blood pressure, as well. While regular exercise helps lower blood pressure in the long run, blood pressure does rise during an exercise session, as the heart works harder. But increases that run too high could be a sign of impending cardiovascular disease. The researchers, from VA and the University of Utah, say the work adds to the understanding of the impact of age and sex on blood pressure. The work was funded by VA and the American Heart Association. (The FASEB Journal, April 2017)
|
Expanding VA home-based primary care to American Indian communities
 Photo for illustrative purposes only. ©iStock (09/11/2017)
VA’s home-based primary care (HBPC) enables aging, infirm Veterans to stay in their homes, rather than move to long-term care facilities. But the model was developed in urban settings, and extending it to rural areas involves unique challenges. Researchers studied the roll-out of HBPC at 14 VA medical centers that reached out to Native American reservations in their regions. A dozen succeeded in implementing a HBPC program. The study found variations across the sites. Typically, however, there were “key individuals who were able to build trust and faith in VA healthcare among American Indian communities.” All the programs required adaptations to overcome barriers associated with rural areas. Examples were care providers needing to travel long distances to reach Veterans’ homes, and delays in hiring additional clinicians to ease heavy caseloads. The study team urges more opportunities for federal health care organizations—including VA—and nonfederal health agencies to network and share what they have learned about providing care to American Indians. (Implementation Science, Sept. 2, 2017)
|
Behavioral health needs spur enrollment in VA care for Army Guard, Reserve members
 Photo for illustrative purposes only. ©iStock/Marjan_Apostolovic (09/06/2017)
Army National Guard and Reserve members with greater behavioral health needs are more likely than those with fewer needs to link to the Veterans Health Administration after deployment, found a study by VA Salt Lake City and VA Palo Alto Health Care Systems researchers and their colleagues. Service members are screened for alcohol misuse, depression, and PTSD three to six months after returning from deployment. Those who screened positive for PTSD and depression were more likely to enroll in VA health care, and 54 to 84 percent received VA treatment once diagnosed. Men who screened positive for alcohol misuse were more likely to enroll in VA health care, but women were not. Relatively few men and women diagnosed with alcohol use disorder received treatment. While the findings about VA health care engagement are encouraging, more outreach is needed toward those with alcohol use disorder, especially women Veterans, say the researchers. (Psychiatric Services, Aug. 1, 2017)
|
Arthritis prevalent in Iraq, Afghanistan Veterans
 Photo: U.S. Army (09/06/2017)
Arthritis is prevalent among Veterans of Iraq and Afghanistan, and is associated with other health problems, according to a study of VA patient data. The researchers found that nearly 12 percent of Iraq and Afghanistan Veterans had arthritis, higher than the rate found in the civilian population. Those with arthritis had greater frequencies of diabetes, high lipid levels, high blood pressure, and obesity than those without arthritis. Patients with arthritis also had higher level of prescription opioid and anti-inflammatory use. The results suggest that the need for arthritis care will increase as VA assumes the health care of Veterans from these conflicts, say the researchers. (Journal of Orthopaedic Research, March 2017)
|
Protein treatment may protect against TBI damage, finds mice study
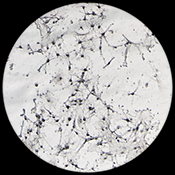 Photo: ©iStock/defun (09/06/2017)
Treatment with a neuronal protein could protect the brain from damage from traumatic brain injury, found a study by VA Pittsburgh Healthcare System researchers. The researchers combined UCH-L1, a protein expressed in high levels in neurons, with other proteins to increase its ability to affect neurons. They then injected this protein into mice with TBI. The mice treated with the protein showed better brain function than controls, and neuron cell survival was also improved. The results suggest that treatment with this protein combination has the potential to improve cognitive function when given weeks or months after a TBI, say the researchers. (PLoS One, May 24, 2017)
|
Identifying health disparities in Veterans
 For illustrative purposes only. Photo: ©iStock/digitalskillet (08/30/2017)
A recent VA Evidence-based Synthesis Program literature review created a map of the evidence to identify knowledge gaps on health disparities within VA. Of the 351 studies included in the review, more than half focused on health care disparities based on race or ethnicity. The second and third most common topics were disparities based on sex and mental health condition, respectively. Very few studies focused on disparities related to sexual or gender identity or homelessness. Race/ethnicity studies more often looked at quality of care, while studies on other Veteran populations tended to focus on health care utilization. Within the studies on race/ethnicity, the majority focused on health care usage by black Veterans, with far fewer studies examining other minorities. The authors note that findings from the various studies varied widely by population, and by the particular outcome studied. Understanding where data is lacking can help VA further address health care disparities in Veterans, say the researchers. (Medical Care, September 2017)
|
Palliative care nurses improve care planning in patients with advanced cancer
 Photo: ©iStock/LPETTET (08/30/2017)
An embedded palliative care nurse can improve care planning for patients with advanced cancer, found a Greater Los Angeles VA Healthcare System study. Palliative care refers to care to improve quality of life by focusing on relieving symptoms and stress, rather than treating a disease directly. Patients in oncology clinics with a palliative care nurse practitioner were more likely to have advance care planning than those in clinics without an embedded palliative care nurse. Hospice referral was also significantly higher in the clinics with a palliative care nurse. This model could be a good way to support the treatment of patients with advanced cancer, say the researchers. (Journal of Oncology Practice, Aug. 16, 2017)
|
Taking multiple medications associated with increased risk of death
 Photo: ©iStock/WanjaJacob (08/30/2017)
Polypharmacy, or the use of multiple medications at the same time, is associated with increased risk of death, found an Iowa City VA Health Care System literature review. Researchers reviewed 47 studies from the available literature. They found that the risk of death increased with the number of medications being taken. The researchers note that it is unclear whether polypharmacy is responsible for the increased risk of death, or whether the association is driven mainly by the fact that people in worse health — and therefore at higher risk of death — tend to be on more medications. In either case, the researchers urge prescribers to pay close attention to patients’ overall medication burden when prescribing new drugs. (Journal of the American Pharmacists Association, Aug. 4, 2017)
|
Electrical brain stimulation could reduce osteoarthritis knee pain
 Photo: ©iStock/meen_na (08/23/2017)
Directly stimulating the brain with electrical current may reduce pain in patients with knee osteoarthritis, according to a study including a researcher with the South Central VA Health Care Network. Researchers assigned 40 participants either to the experimental group receiving noninvasive electrical stimulation or to a control group. They applied an electrical current using sponge electrodes placed on the head of experimental-group participants, once a day for five consecutive days. Participants who received electrical stimulation indicated significantly less knee pain than the control group, which lasted up to three weeks, although pain reduction was not seen on every pain assessment used. The researchers explain that electrical stimulation might reduce pain by modulating activity in brain areas involved in pain processing. The results suggest that electrical stimulation could be an alternative to medication for reducing osteoarthritis pain, they say. (Brain Stimulation, May 19, 2017)
|
BMI is a risk factor for colorectal cancer death
 Photo: ©iStock/Raycat (08/23/2017)
A Minneapolis VA Health Care System and University of Minnesota study confirmed that higher body mass index is linked to greater risk of death from colorectal cancer. Researchers followed more than 46,000 participants for 30 years. Participants who were overweight or obese based on BMI scores had a marginally increased risk of death from colorectal cancer. Although lifestyle risk factors such as BMI have been linked with colorectal cancer death, results on this link have been inconsistent. This is the first study to show a direct association between BMI and long-term colorectal cancer mortality, say the researchers. (Digestive Diseases and Sciences, July 21, 217)
|
Repeated upper endoscopy overused in VHA
 Photo: ©iStock/zilli (08/23/2017)
Repeated upper endoscopy is overused in the Veterans Health Administration, found a study by researchers from several VA health care systems. Upper endoscopy is a procedure in which a camera is used to look at the esophagus, stomach, and beginning of the small intestine. Although common, upper endoscopy is invasive and costly. Of the 85,690 cases of VHA patients receiving repeated upper endoscopy in a five-year period, 50 percent were deemed to be possible or probable overuse. Although overuse of this procedure is common within VHA, the authors note that it is less likely to be overused in VHA than in health systems that serve Medicare beneficiaries. Efforts are needed to better understand why this procedure is overused and to promote appropriate use, say the researchers. (American Journal of Gastroenterology, July 11, 2017)
|
Reducing opioid dose in long-term therapy may be beneficial, but evidence is limited
 Photo: ©iStock/Hailshadow (08/15/2017)
A literature review by researchers from several VA health care systems suggested that reducing opioid dose may improve pain, function, and quality of life for patients on long-term opioid therapy. However, most of the studies found were of poor quality. This shows that there is inadequate evidence on the risks of opioid tapering, say the researchers. They suggest that clinicians should discuss the potential benefits of opioid tapering with patients, in addition to discussing the goals and risks of opioid therapy. More studies are needed on the effects of reducing opioid dosage, according to the researchers. (Annals of Internal Medicine, Aug. 1, 2017)
|
Lower natriuretic peptide levels found in racial groups more prone to hypertension and diabetes
 Photo: ©iStock/solidcolours (08/15/2017)
Hormone concentrations linked to several diseases differ based on genetic heredity, found a study including a researcher from the VA San Diego Healthcare System. Lower levels of hormones called natriuretic peptides are associated with increased risk of hypertension and diabetes. Studying over 5,000 people, the researchers found that natriuretic peptide levels were 44 percent lower in black participants and 46 percent lower in participants of Chinese descent, compared with white participants. Natriuretic peptide levels for Hispanic participants fell in between the white participant group and the other two groups. Hispanic participants with higher genetic European ancestry had higher levels, while those with higher African ancestry had lower levels. Black participants with higher genetic European ancestry also had higher natriuretic peptide levels. The results could help explain why hypertension and diabetes are more common in black, Chinese, and Hispanic individuals than in white individuals, say the researchers. (American Journal of Cardiology, June 30, 2017)
|
Patients comfortable receiving text messages about HIV testing
 Photo: ©iStock/ballero (08/15/2017)
Text messages could be used to prompt patients to ask their doctors about HIV testing, according to a study by researchers from the Michael E. DeBakey VA Medical Center and their associates. Researchers surveyed 265 patients in a health center waiting room. They found that that 55 percent of patients had never talked to their doctors about HIV testing. Of those, 74 percent said that they would be comfortable asking their doctors for the HIV test. A majority of patients surveyed said they would be comfortable receiving text messages prompting them to talk to their doctors about HIV testing. Text messages could be a useful tool to encourage communication between patients and doctors about HIV testing, say the researchers. (Journal of the Association of Nurses in AIDS Care, July 11, 2017)
|
Suicide attempt risk increases in Army units with a history of suicide attempts
 Army photo by Staff Sgt. Jennifer Bunn. For illustrative purposes only. (08/10/2017)
The risk of suicide attempt among soldiers increased with the number of other suicide attempts made within the unit within the past year, found the Army Study to Assess Risk and Resilience in Servicemembers. The results show that suicide attempts by members of one's unit increase the risk of suicide attempt for a soldier. The odds of a suicide attempt were more than double for a soldier in a unit with five or more attempts in the past year, compared to one in a unit with no attempts within the past year. Suicide attempts within a unit were associated with risk of future suicide attempts regardless of unit size or job within the military. The study suggests preventive efforts should target those who have been exposed to suicide attempts by members of their units, in addition to those who know people who died by suicide, say the researchers. (JAMA Psychiatry, July 26, 2017)
|
Heart failure may increase risk of chronic kidney disease
 Photo for illustrative purposes only. ©iStock/digitalskillet (08/10/2017)
Heart failure may be associated with a higher risk of chronic kidney disease, according to a Memphis VA Medical Center study. Examining data from more than 3 million Veterans, the researchers found that those with heart failure had a much higher rate of chronic kidney disease than those without. Of patients with heart failure, 22 percent had a rapid decline in kidney function over a two-year period, while only 8.5 percent of patients without heart failure had such a decline. Heart failure has not previously been linked to poor kidney outcomes in patients with normal kidney function. (Circulation: Heart Failure, August 2017)
|
Pre-surgery chemotherapy may improve survival in pancreatic cancer
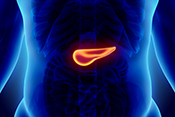 Photo: ©iStock/yodiyim (07/31/2017)
Chemotherapy before surgery could lower the risk of death for people with pancreatic cancer, according to Michael E. DeBakey VA Medical Center and Baylor College of Medicine researchers. By studying data from nearly 20,000 patients, the researchers found that those who underwent chemotherapy before surgery survived longer than those who had only surgery to remove the pancreas, or those who received chemotherapy after surgery. The study is the first to convincingly demonstrate a clear benefit of pre-surgery chemotherapy. (Surgery, June 27, 2017)
|
Electronic health record alerts linked to provider burnout
 Photo: ©iStock/monkeybusinessimages (07/31/2017)
Increased notifications from electronic health records can contribute to provider burnout, found a Michael E. DeBakey VA Medical Center study. Physicians and other providers often do not have protected time devoted to responding to these messages. The notifications could include, for example, test results, referral responses, medication refill requests, and messages from colleagues. In a survey of care providers, the researchers found that those who felt their workloads had increased because of electronic health record notifications were more likely to experience physical fatigue and cognitive weariness, two signs of burnout. They suggest that training, protected time for alert management, and improvements to electronic health record systems could help providers avoid burnout. (Applied Clinical Informatics, July 5, 2017)
|
Biopsy pattern can predict lethality of prostate cancer
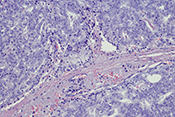 Photo: ©iStock/OGphoto (07/31/2017)
A specific pattern on a prostate biopsy can predict the risk of cancer metastasis (spread) and mortality, according to a study of VA medical center data. The Gleason score grades tissue samples from 1 (normal prostate tissue) to 5 (very abnormal cancer growth patterns), and combines the two highest grades from a number of samples for a composite score for the biopsy. Two samples graded 3 and 5 would yield a Gleason score of 8, as would two samples both graded 4. The researchers found that patients with a grade of 5 on any tissue sample had a greater risk of metastasis and death than those with a Gleason 4+4 pattern, regardless of the grades of other samples in the biopsy. The results suggest that the presence of a sample graded as 5 should be viewed as an indicator of a uniquely aggressive cancer, regardless of the composite score, say the researchers. (Journal of Urology, July 11, 2017)
|
TBI and psychiatric conditions may lead to greater suicide risk
 Photo: ©iStock/Nikada (07/20/2017)
Psychiatric conditions may add to the relationship between traumatic brain injury and suicide, according to a VA Boston Healthcare System study. The researchers looked at data for more than 270,000 Veterans deployed to Iraq and Afghanistan. They found that Veterans with a TBI had an increased risk of a suicide attempt. Further, 83 percent of those with TBI who attempted suicide also had a psychiatric condition. Conditions examined were PTSD, depression, anxiety, and substance use. While these conditions on their own could increase suicide risk, they may help explain the correlation between TBI and suicide. Psychiatric conditions are more common in people with TBI. The results suggest that Veterans with these conditions should be monitored closely for suicidal behavior, say the researchers. (American Journal of Epidemiology, May 3, 2017)
|
Parents' PTSD linked to children's psychosocial problems
 Photo for illustrative purposes only. ©iStock/Squaredpixels (07/20/2017)
PTSD symptoms in parents are related to lower psychosocial functioning in their children, found a study by Central Texas Veterans Health Care System researcher and colleagues. Researchers surveyed more than 100 Veterans with children between ages 3 and 18. Veterans with PTSD reported lower levels of parenting satisfaction, and children of Veterans with PTSD had higher levels of psychosocial problems, such as trouble sleeping and behavioral problems. Positive parenting, as opposed to parenting based on punishment, was linked to higher parent satisfaction and child psychosocial problems. But parents with PTSD were less likely to practice positive parenting. The results suggest that offering resources to improve positive parenting and to better address the influence of PTSD on the parent-child relationship would be helpful, say the researchers. (Military Behavioral Health, May 23, 2017)
|
Study suggests steps to curb anesthesia-related adverse events
 Photo: ©iStock/knape (07/20/2017)
A study by VA's National Center of Patient Safety identified 36 adverse events involving anesthesia care in VA during a three-year period between 2012 and 2015. The most common event was medication errors. The authors say increased standardization could further decrease adverse events. They recommend expanding efforts to incorporate bar codes, checklists, and simulations of best practices. They also suggest storing similar-looking or -sounding medications separately, and limiting the stock of high-risk medications. (Anesthesia and Analgesia, July 1, 2017)
|
Emotional awareness and expression training reduces IBS symptoms
 Photo: ©iStock/Steve Debenport (07/13/2017)
Emotional awareness and expression training (EAET) can reduce irritable bowel syndrome symptoms, found a study headed by a Michael E. DeBakey VA Medical Center researcher. Participants took part in three weeks of either EAET or relaxation training. EAET teaches patients to recognize emotions related to stressful situations and to express those emotions directly. Participants receiving EAET had significant improvements in IBS symptoms both after training and 10 weeks later, compared to both the relaxation training group and controls. However, EAET did not improve psychological symptoms, such as depression and anxiety, while relaxation therapy did. The results show that EAET may be an effective additional treatment for IBS, say the researchers. (Neurogastroenterology and Motility, June 22, 2017)
|
Treating trauma-related muscle loss with stem cells
 Photo: ©iStock/ChrisChrisW (07/13/2017)
Researchers with the VA Palo Alto Health Care System were able to treat volumetric muscle loss in mice using muscle stem cells. Volumetric muscle loss is the loss of skeletal muscle from trauma or surgery. By using a 3D muscle tissue scaffold to give the stem cells structure, the researchers were able to stimulate muscle regeneration. They also found that physical therapy after the muscle construct was implanted improved function of the muscles. The results show that cell-based therapies may be an effective way to engineer tissue within animals and people, according to the researchers. (Nature Communications, June 20, 2017)
|
'Anxiety sensitivity' seen as possible link between PTSD, suicide risk
 Photo for illustrative purposes only. ©iStock/Marjan_Apostolovic (07/13/2017)
Anxiety sensitivity may help explain the connection between PTSD and suicide, according to a Southeast Louisiana Veterans Health Care System study. Anxiety sensitivity is an exaggerated fear of experiencing symptoms related to anxiety, separate from the actual symptoms. Studying 60 male Veterans, the researchers found a significant association between PTSD symptom severity and greater frequency of suicidal thoughts, plans, and impulses. The results further showed that cognitive anxiety sensitivity concerns may be responsible for this link. The results suggest that when people with PTSD worry that their personalities have changed or that they are not thinking normally, this may underlie an increased risk of suicidal behavior. (Journal of Affective Disorders, June 19, 2017)
|
Yelp ratings give edge to VA hospitals, study finds
 Photo: ©iStock/Tinpixels (07/13/2017)
VA hospitals scored slightly higher in Yelp ratings than their affiliated university hospitals, according to a study by a team with VA and Stanford University. Yelp is an online customer rating service that allows the public to post ratings and reviews of a wide range of products and services, including doctors and hospitals. The VA and Stanford researchers found that on average, the VA hospitals scored half a point better than their affiliates: 3.70 versus 3.19. On Yelp, five stars is the top rating, and one the lowest. Past research, including a 2016 study by VA researchers and others, has shown that online consumer reviews may be a good reflection of official hospital performance measures, such as those from the Centers for Medicare and Medicaid Services. The authors note that analyzing Yelp ratings can also complement other research that involves more extensive and rigorous comparisons of hospital quality. (American Journal of Managed Care, June 28, 2017)
|
Finding the best treatment for hoarding disorder
 Photo: ©iStock/trekandshoot (07/05/2017)
Older adults with hoarding disorder had greater improvement with cognitive rehabilitation and exposure/sorting therapy (CREST) than with geriatric case management, found a study by VA San Diego Healthcare System researchers. Hoarding disorder involves a psychological inability to throw possessions away, and can lead to health and safety risks. Participants received one of the treatments in 26 sessions over six months. About 2 to 6 percent of the general population shows hoarding symptoms, and the rate may be up to three times higher in older adults. Those in the CREST group had a 38 percent improvement in symptoms, while those in the case management group improved by 25 percent. CREST involves cognitive training and behavioral exposure to stressors. Case management involves more standard support and advocacy. Both groups continued to show improvement six months after treatment. The results show that CREST is an effective treatment for hoarding disorder, but that case management is also beneficial, say the researchers. (Journal of Clinical Psychiatry, May 23, 2017)
|
Little research available on probiotics, prebiotics for TBI, PTSD
 Photo: ©iStock/Barmaleeva (07/05/2017)
A literature review by researchers at the VA Rocky Mountain Mental Illness Research Education and Clinical Center found little research on using prebiotics and probiotics to treat traumatic brain injury and PTSD. Recent findings have suggested that inflammation may be an underlying mechanism of both TBI and PTSD. If this is so, anti-inflammatory agents such as prebiotics or probiotics could present a new strategy to treat both conditions. Prebiotics are nondigestible food ingredients, such as fiber, that promote the growth of helpful bacteria in the body. Probiotics are living micro-organisms that provide health benefits when eaten, such as healthy bacteria found in yogurt. However, the researchers found only three studies addressing probiotics and TBI and one study on PTSD. They did not find any studies on probiotic treatments for TBI and PTSD together. More studies are needed to explore the possibilities of this type of treatment for the two conditions, say the researchers. (Brain, Behavior, and Immunity, June 9, 2017)
|
Intestinal fungi play role in alcoholic liver disease
 Photo: ©iStock/ksass (06/14/2017)
Chronic alcohol consumption can lead to an imbalance of intestinal fungi, which in turn can lead to chronic liver disease, according to a study that included researchers from the VA San Diego Healthcare System. In mice, alcohol consumption increased the amount of fungus in the intestines, and also allowed the fungus to travel to other parts of the body. This increased the likelihood of liver disease. Treating the mice with antifungal drugs reduced the fungal overgrowth. The researchers also studied human patients, and found that those with alcohol dependence had lower fungal diversity and too much of one specific fungus. The people with this fungal imbalance had higher mortality rates. While several types of fungi naturally occur in the human intestine, they can cause harm if they spread to other parts of the body. The results show that alcohol affects levels of intestinal fungi and that controlling these fungi levels may help treat alcohol-related liver disease, say the researchers. (Journal of Clinical Investigation, May 22, 2017)
|
Childhood mistreatment linked to suicidal behavior
 Photo: ©princessdlaf (06/14/2017)
Childhood mistreatment is strongly associated with suicidal behavior among new soldiers, according to the Army Study to Assess Risk and Resilience in Servicemembers. The research team, led by a VA San Diego Healthcare System psychiatrist, looked at data for nearly 40,000 soldiers reporting for basic training. They found that those who reported childhood abuse or neglect had higher odds of suicidal thoughts or attempts over their lifetime. More frequent and pervasive mistreatment was more strongly associated with suicidal behavior. Focus on childhood abuse might lead to new ways to reduce suicide risk among new soldiers, say the researchers. (Journal of Clinical Psychiatry, May 23, 2017)
|
Mantram repetition program improves insomnia
 Photo by Kevin Walsh (06/08/2017)
The mantram repetition program (MRP) helped manage insomnia in patients with PTSD, in a VA San Diego Healthcare System study. The MRP is a "mind-body-spiritual intervention" that "teaches a portable set of cognitive-spiritual skills for symptom management," according to the research team. Patients who participated in the MRP over eight weeks had significant improvement in insomnia symptoms, compared with before they used the program. MRP participants also had moderate improvements in PTSD symptoms. The results suggest that mantram meditation could be useful to address both insomnia and PTSD symptoms, say the researchers. (Advances in Nursing Science, April 2017)
|
Homelessness among Veterans seen in specialty mental health care
 Photo: ©iStock/kevinruss (06/08/2017)
Researchers from VA New England MIRECC and Yale School of Medicine studied the one-year incidence of homelessness among 300,000 Veterans seen in VA specialty mental health clinics. They found that 5.6 percent of Veterans referred to anxiety or PTSD clinics experienced homelessness. The homelessness rate for the entire Veteran population is about 3.7 percent over a five-year period. Veterans who were unmarried or diagnosed with a drug use disorder were more than twice as likely to become homeless. Black Veterans or those earning less than $25,000 a year were more than one and a half times as likely to become homeless. Monitoring early signs of housing vulnerability in this population is important to preventing homelessness, say the researchers. (Psychological Services, May 2017)
|
Testosterone replacement therapy could lower risk of atrial fibrillation
 Photo: ©iStock/sudok1 (06/08/2017)
Returning testosterone to normal levels using testosterone replacement therapy (TRT) appears to significantly decrease the incidence of atrial fibrillation, according to a Kansas City VA Medical Center study. Atrial fibrillation is the most common irregular heart rhythm, and causes a high number of cardiac problems and deaths. Looking at the records of more than 70,000 Veterans, the researchers found that patients whose testosterone levels were normalized by TRT had significantly lower risk of atrial fibrillation than those who had TRT but not normalized testosterone levels or those who did not receive TRT. The results suggest that low testosterone levels are associated with higher risk of atrial fibrillation, say the researchers. (Journal of the American Heart Association, May 9, 2017)
|
ALS medicine may help fight drug-resistant cancer
 Photo: ©iStock/vitanovski (06/08/2017)
The drug riluzole may be useful in treating some drug-resistant cancers, according to a study including researchers from the Miami VA Healthcare System. The researchers found that reactive oxygen species, chemical compounds containing oxygen, were present in cisplatin-resistant cells. Cisplatin is a common chemotherapy medication. They used riluzole, a drug used to treat ALS, to increase the amount of reactive oxygen species in these cancerous cells. Increasing the ROS levels selectively killed the cisplatin-resistant cells. The results show that riluzole could be repurposed as an antitumor agent, say the researchers. (Oncotarget, May 2, 2017)
|
'Psychological autopsy' explores suicide risk factors
 Photo: ©iStock/vadimguzhva (06/08/2017)
A team including researchers with the VA San Diego Healthcare System performed "psychological autopsies" to look for differences between soldiers who died by suicide and matched control groups. Researchers talked to next of kin or Army supervisors of soldiers who had died by suicide. They compared responses to those of similar relations of two other groups of soldiers: one matched to the experimental group demographically, and the other comprised of soldiers who had suicidal thoughts but had not completed suicide. Almost 80 percent of soldiers who died by suicide had a prior mental disorder, and about half told someone that they were considering suicide. The risk factors for those who died by suicide were not different from the risk factors for those with suicidal thoughts, showing that more research is needed into what moves someone from thinking about suicide to completing the act. (Psychological Medicine, May 15, 2017)
|
Homeless Veterans have more negative primary care experiences than non-homeless Veterans
 Photo: ©iStock/Solange_Z (05/25/2017)
Homeless Veterans consistently reported more negative experiences with primary medical care than non-homeless Veterans, in a large national survey of Veterans with mental health and/or substance use disorders. Homeless Veterans reported more negative experiences with comprehensive care, communication, care coordination, medication decision-making, and self-management support than non-homeless Veterans. Negative experiences with primary care may make homeless Vets more likely to avoid mental health and substance use treatment, say the researchers. Homeless Vets may need more specific services aimed at encouraging them to continue with primary care services, they conclude. VA implemented patient-aligned care teams specifically tailored to homeless Veterans in 2012, but the effects of this program have not been studied thoroughly. (Psychological Services, May 2017)
|
New system implemented to advise patients of pregnancy risks from medications
 Photo: ©iStock/michaeljung (05/25/2017)
The VA Pittsburgh Healthcare System recently began a program to guide primary care providers in discussing teratogenic medications. A teratogen is something that could cause pregnancy problems or complications. The new framework is called TARCC, which stands for teratogen, alternative, risks, contraception, and chart. It is designed to remind care providers of what to discuss with patients when prescribing new medicines. While research shows that a high number of women Veterans are prescribed teratogenic medications, the majority do not receive counseling on risks or on contraceptive topics. This lack of communication prompted the new system. TARCC has been added as part of the electronic health record reminder system. The study authors plan to evaluate the effects of the TARCC reminders after they have been in place for at least a year. After being shared at a VA women's health conference, TARCC has been adopted in educational literature distributed nationally to VA health care providers. (Journal of Midwifery and Women's Health, May 9, 2017)
|
Study proposes redefining 'normal' levels of blood iron
 Photo: ©iStock/spanteldotru (05/25/2017)
A team of VA researchers defined new levels of ferritin and transferrin in the blood to be used as indicators of type 2 diabetes and cardiovascular disease risk. Ferritin and transferrin are proteins that contain iron and are found in blood. Research has shown that high iron levels correlate with both diabetes risk and death from cardiovascular disease. However, the levels of ferritin and transferrin that are considered "normal" are so broad that increased risk of both diseases has been seen in the normal ranges. The researchers found that ferritin levels of 15 ng/mL up to 80–100 ng/mL (nanograms per milliliter) in the blood and transferrin levels of 15 to 55 percent were associated with lower type 2 diabetes and cardiovascular disease risk, and therefore should be considered the proper “normal” range. (Current Diabetes Review, May 4, 2017)
|
Aggressive care at end of life for lung cancer linked to lower family satisfaction
 Photo: ©istock/beerkoff (05/18/2017)
Aggressive care in the last month of life for patients with non-small cell lung cancer was associated with lower family satisfaction with care, according to a study of VA data. Aggressive care includes chemotherapy, mechanical ventilation, acute hospitalization, and being admitted to an intensive care unit. The researchers looked at data on 847 cancer patients who died in VA care over a three-year period. They found that families of patients who had received at least one episode of aggressive care rated care lower compared with when aggressive care did not take place. Families of patients in hospice or palliative care units tended to rate care higher. The results suggest that aggressive care does not contribute positively to patients' and families' experiences in the final days of life, say the researchers. (Cancer, April 17, 2017)
|
Collaboration to accelerate proteogenomics cancer care
 Photo: ©istock/selvanegra (05/18/2017)
VA, the Department of Defense (DoD), and the National Cancer Institute have joined forces to advance cancer research and care. The new program, described in a recent journal article, is called the Applied Proteogenomics Organizational Learning and Outcomes Network, or APOLLO. The three agencies will work together to use advanced genomic and proteomic techniques to address cancer treatment at a molecular level. Genomics is the study of DNA and RNA, while proteomics is the molecular study of proteins. The collaboration arose out of the Cancer Moonshot initiative. (Clinical Pharmacology and Therapeutics, May 2017)
|
Possible biomarker of Gulf War illness identified
 Photo: Tech. Sgt. H. Deffner, U.S. Army (05/18/2017)
A team including several VA researchers identified biomarkers in the blood of both rodents and humans that may indicate Gulf War illness (GWI). Both animals and humans showed increases in multiple types of phospholipids related to GWI. These findings suggest inflammatory imbalances in GWI, since phospholipids play a role in the inflammatory process, say the researchers. GWI is hard to diagnose because it can present as multiple different symptoms. As such, identifying biological changes related to the condition could help with diagnosis and treatment. (PLoS One, April 28, 2017)
|
Psychological treatment may help patients with IBS
 Photo for illustrative purposes only. ©iStock/bowdenimages (05/12/2017)
Psychological treatments have some benefits for patients with irritable bowel syndrome (IBS), according to a literature review by researchers at the Michael E. DeBakey VA Medical Center. The researchers looked at studies of direct psychological treatments in gastrointestinal practices. They found that patients saw short-term benefits after treatment regardless of the type of treatment. IBS and pain symptoms improved for patients in behavioral therapy, mindfulness-based stress reduction, and emotional awareness training, compared with patients receiving no treatment. While these treatments seem to benefit patients with IBS, evidence on their effectiveness in this setting is limited. More research is needed to find best practices for psychological treatment in gastrointestinal care, say the researchers. (Digestive Diseases Week meeting, May 9, 2017)
|
Online weight-management program effective for patients with mental illness
 Photo for illustrative purposes only. ©iStock/lovro77 (05/12/2017)
An online weight-management program proved more effective than an in-person program or usual care, in a Greater Los Angeles VA Healthcare System study. Researchers assigned 276 overweight patients with serious mental illness either to computerized weight management with peer coaching (WebMOVE), in-person weight services, or usual care. Those in the WebMOVE group lost an average of six pounds after six months. Those in the other two groups did not show a significant change. Patients with mental illness face barriers to in-patient intervention because of expensive clinician time required and transportation problems. But an online program can be tailored to patients' specific needs and easily administered, say the researchers. (Journal of General Internal Medicine, April 2017)
|
Protein shown to suppress breast cancer growth in lab setting
 Photo: ©iStock/vitanovski (05/12/2017)
Researchers at the Kansas City VA Medical Center have shown how a specific protein can control breast cancer tumor growth and progression. By isolating a breast cancer cell line in the lab, the researchers showed how the protein CCN5 regulates the transition of cancer stem cells into cancer epithelial cells. CCN5 essentially blocks cellular growth by making tumor-initiating cells into non–tumor-initiating cells. Less expression of CCN5 by the genes correlates to tumor growth. The researchers speculate that restoring CCN5 protein could be beneficial in breast cancer and possibly other forms of cancer. (Scientific Reports, April 27, 2017)
|
CPAP could ease PTSD in Vets with sleep apnea
 Photo: ©iStock/BVDC (05/04/2017)
PTSD symptoms improved in patients with obstructive sleep apnea who were given continuous positive airway pressure (CPAP) treatment, found a VA Western New York Healthcare System study. The researchers had 47 Veterans with obstructive sleep apnea use a CPAP device while they slept for three months. They found that patients' PTSD symptom improvement correlated with consistent CPAP usage. Veterans with severe to very severe PTSD had larger improvements than those with mild to moderate PTSD. CPAP usage also decreased the frequency of nightmares. The abatement of PTSD symptoms could be the result of better sleep from treating patients' sleep apnea, say the researchers. (Sleep Medicine, May 2017)
|
Little research available on blast versus nonblast TBI
 DoD photo by Lance Cpl. Immanuel Johnson (05/04/2017)
A literature review by Minneapolis VA Health Care System researchers found that little information is available about outcomes for blast versus nonblast traumatic brain injury (TBI) in U.S. military personnel. The research available shows that blast and nonblast TBI groups had similar rates of depression, sleep disorders, alcohol use, vision loss, balance problems, and functional status. Results were inconsistent about PTSD, headache, hearing loss, and neurocognitive functions. More research is needed on the differences between blast and nonblast TBI, along with consistent definitions of blast exposure, say the researchers. (Journal of Head Trauma Rehabilitation, April 18, 2017)
|
Study probes links between smoking, increased pain
 ©iStock/bagi1998 (05/04/2017)
There may be an association between smoking, gender, and musculoskeletal pain, according to a VA study. Researchers surveyed more than 1,000 Veterans who served in Iraq or Afghanistan about PTSD symptoms, depressive symptoms, and pain severity. They found that female Veterans who smoked had more moderate to severe musculoskeletal pain than female nonsmokers. This difference was not significance in male Veterans. Smoking may serve as a stress-reducer for some patients, which may explain why those in greater pain are more likely to smoke. The results support a need for more research on the gender-based risk factors for pain in Veterans who smoke, say the researchers. (Pain Medicine, March 14, 2017)
|
Drug-resistant bacteria on the rise in patients with spinal cord injury
 Photo: ©iStock/Scharvik (04/27/2017)
Patients with spinal cord injury and related disorders are at an increased risk of drug-resistant bacterial infection, according to a study of 130 VA medical centers. Researchers found that more than a third of gram-negative bacterial infections found in patients over a nine-year period were drug-resistant. Over that period, drug-resistant strains of bacteria became increasingly common. Infections may be more common in spinal cord injury patients because of altered bodily function as a result of the injury. Infections may also be diagnosed later than usual because of the loss of sensation. Priority should be given to controlling the spread of resistant bacteria and studying epidemiologic trends in spinal cord injury patients, say the researchers. (Journal of Spinal Cord Medicine, Feb. 15, 2017)
|
Mapping brain activity in PTSD and mild TBI
 Photo: ©iStock/spanteldotru (04/27/2017)
Researchers from two VA health care systems and their colleagues used a technique called magnetoencephalography to map activity in the brains of patients with PTSD and mild traumatic brain injury. Magnetoencephalography records the magnetic fields produced by electrical currents in the brain. The researchers found that alpha brain waves showed reductions in network structure—the interconnected system of neurons within the brain—in PTSD. The scans also showed a shift in connectivity from alpha bandwidth electrical activity to theta bandwidth in both conditions. There was also increased randomness associated with PTSD and increased structure with traumatic brain injury. The study shows the potential of magnetoencephalography to analyze brain activity in these two conditions, and to distinguish between them when similar symptoms occur, say the researchers. (Brain Connectivity, February 2017)
|
Case study points to better strategy for monitoring liver cancer
 Photo: ©iStock/luchsche (04/27/2017)
A recent case study suggested that screening for liver cancer at the molecular level for high-risk patients could help manage the disease. The hepatitis C virus is a major risk factor for liver cancer. An international team including a researcher from the Iowa City VA Health Care System followed a patient with hepatitis C and liver cancer. The patient had three tumors treated and removed. He then achieved sustained virologic response — when the hepatitis C virus is not detected in the blood. The researchers then compared RNA molecules from the patient with samples from other patients with liver cancer and hepatitis C. The comparison showed that the patient was at high risk for the cancer to return. By screening for cancer more frequently, at three-month intervals, the care team was able to detect a liver lesion early and treat it. They say the molecular biomarker test could help with early cancer detection in the growing population of hepatitis C patients. (Hepatology)
|
New technique for artificial lung manufacturing
 Photo: Jason Miller (04/21/2017)
Researchers with the VA Ann Arbor Healthcare System have come up with a new way to manufacture microfluidic artificial lungs that may have applications for human patients. Artificial lungs have been used for years to supplement patients' breathing, and recent microfluidic artificial lung technology has shown potential for great improvement in function. But microfluidic artificial lung material is hard to scale large enough for human use. The researchers have found a way to assemble a lung structure through continuous "rolling" and bonding of a single, patterned layer of polydimethyl siloxane. They expect that this technique will work to construct microfluidic artificial lungs large enough for human use. (Biomicrofluidics, April 2017)
|
Evaluation reveals areas for improvement in Veterans Choice Program
 Photo: ©iStock/sturti (04/21/2017)
Researchers at the Louis Stokes Cleveland VA Medical Center used the Lean Six Sigma quality-improvement strategy to evaluate the Veterans Choice Program (VCP), which allows eligible VA-enrolled Veterans to get certain health services at non-VA sites in their communities. The study found that key issues to target for improvement included inefficient exchange of information between staff and patients, shortages of VCP-participating providers, appointment duplication, declines in care coordination, and lack of program adaptability. Using evaluations such as Lean Six Sigma could help identify further ways to improve the program, suggest the researchers. (Medical Care, April 13, 2017)
|
Bulk of VA testosterone use for off-label purposes
 Photo: ©iStock/RapidEye (04/21/2017)
Only a small portion of testosterone prescriptions given in VA were for conditions for which testosterone has been approved by the FDA, according to a study of VA system data. The FDA approves testosterone only for diseases of the testis, pituitary, and hypothalamus. Yet only 6.3 percent of prescriptions in the VA were for these conditions over a five year period. The results show a need for more efforts to optimize testosterone-prescribing practices, say the researchers. They do note that there may be valid therapy reasons for off-label testosterone use. (Journal of General Internal Medicine, March 2017)
|
Many wet wipes contain potential allergens
 Photo by April Eilers (04/06/2017)
Two studies by Minneapolis VA Medical Center researchers found that many commonly used wet wipes contain a high number of potential allergens. The researchers examined ingredient lists for 178 facial wipe and 54 personal hygiene wipe products. They found that a majority of wet wipes on the market contain ingredients that could cause allergic contact dermatitis. The most common potential allergens in both types of wipes were fragrances, botanicals, preservatives, and propylene glycol. Preservatives such as methylisothiazolinone are the ingredients most likely to cause contact dermatitis, according to an earlier study by the same researchers and their colleagues that involved more than 9,000 patch-tested patients. It is important to consider the ingredients in wet wipes when evaluating contact dermatitis, say the researchers. (Dermatitis, March 23, 2017)
|
Combination of two therapies may be effective treatment for those with PTSD and borderline personality disorder
 Photo for illustrative purposes only. ©iStock/Highwaystarz-Photography (04/06/2017)
A combination of dialectical behavior therapy and prolonged exposure therapy may be a safe and effective means of treating Veterans with both PTSD and borderline personality disorder, found a Minneapolis VA Health Care System study. Twenty-two Veterans underwent a 12-week intensive outpatient program combining the two treatments. After the treatment, 91 percent of participants showed a significant reduction in PTSD symptoms. Dysfunctional coping styles (e.g., self-harm) were also reduced, as was suicidal ideation. Patients with borderline personality disorder are often excluded from PTSD treatments out of concern for an increased suicide risk. Combining the two treatments shows promise for treating this difficult population, say the researchers. (Journal of Traumatic Stress, March 22, 2017)
|
Frequent in-person coaching most effective for weight loss
 Photo: ©iStock/LeoPatrizi (03/30/2017)
Consistent and continuous treatment is needed to address obesity, according to a study of weight loss programs offered by VA. Researchers at two Midwestern VA medical centers tracked the weight loss of 332 Veterans participating in three different programs over two years. One group received usual care (VA's MOVE! program), one attended a Small Changes group program in person, and one received Small Changes counseling by phone. Small Changes encourages participants to make modest changes to dietary intake and physical activity level. In the first year, in which participants began with weekly sessions and tapered off to monthly sessions, those in the Small Changes in-person group lost twice as much weight as the other two groups. All groups showed significant weight loss. However, in the second year, when Small Changes participants had weight-loss sessions only every two months, the Small Changes in-person group experienced significant weight regain, while the other two groups continued their weight loss. Weight regain was often related to diabetes. The results show that ongoing and frequent contact with coaching is important for weight-management programs, say the researchers. (Journal of General Internal Medicine, March 7, 2017)
|
Nearly half of soldiers with mTBI had postconcussive symptoms three months postdeployment
 Photo: Staff Sgt. William Tremblay/USA (03/30/2017)
In a study by the Defense and Veterans Brain Injury Center study, almost half of soldiers who had a mild traumatic brain injury (mTBI) while serving in Afghanistan or Iraq had postconcussive symptoms three months after their deployment. The researchers examined 366 soldiers with previous mTBI and 599 without three months after they were screened for TBI upon their return. Forty-seven percent of those with mTBI had postconcussive symptoms at the three-month mark, while only 25 percent of controls did. The most common symptoms were sleep problems, forgetfulness, irritability, and headaches. Those with mTBI were twice as likely as controls to have received rehabilitative services after deployment. "The persistence of symptoms, even absent [posttraumatic stress], suggests that mTBI is associated with continuing problems for longer than has been generally recognized in the active duty population," wrote the researchers. (Neurology, March 17, 2017)
|
Alzheimer's caregiver intervention not associated with additional health care costs
 Photo: ©iStock/Eva-Katalin (03/30/2017)
REACH programs to support caregivers of patients with Alzheimer's disease and related dementias did not lead to increased health care costs for either patient or caregiver, according to a study by VA researchers in Tennessee and New York. REACH (Resources for Enhancing Alzheimer's Caregivers Health) provides caregivers with interventions to increase coping skills and management of patient behaviors. Previous research has shown that REACH interventions benefit both caregivers and patients, but concerns about additional health care costs may have hindered the program's adoption. The study shows that REACH did not add to health care costs. In fact, VA patients in the REACH program showed significantly lower health care costs. (Journal of the American Geriatric Society, March 13, 2017)
|
Copper cuts bacteria growth on hospital surfaces
 Courtesy of EOS Surfaces (03/23/2017)
Copper-impregnated surfaces may lower bacteria growth on hospital surfaces, found a Central Texas Veterans Healthcare System study. Copper is known to self-sanitize and naturally reduce the growth of bacteria. However, few studies have looked at its effectiveness in reducing contamination in real-world hospital settings. Researchers measured the number of bacteria on copper-containing and standard bedside tray tables in hospital rooms. They found that the bacteria amount was 81 percent lower on the copper-infused trays 30 hours after the test began. The copper-containing trays showed similar levels of bacteria as trays in rooms under isolation protocol to prevent infection. The copper-infused surfaces used in the study have the appearance of stone. Using them in patient rooms may help reduce the spread of infection in hospitals, say the researchers. (American Journal of Infection Control, Feb. 22, 2017)
|
Recommendations on using weight-management drugs
 Photo: ©iStock/emesilva (03/23/2017)
A VA Health Services Research and Development workgroup recently developed recommendations for the use of weight management medications (WMMs) within VA. Previous data show that only 2 percent of Veterans in VA care eligible for WMMs are prescribed the medications. The workgroup found that barriers to this treatment included patient and provider concerns about safety and efficacy, limited involvement of primary care, and overly restrictive medication criteria. The workgroup recommended educating patients and providers about WMMs and the health benefits of weight loss, increasing primary care provider engagement, relaxing criteria for use, and creating a system to help patients navigate weight-management options. (Journal of General Internal Medicine, April 2017)
|
Past sexual assault linked to risk for sexually transmitted disease
 Photo: ©iStock/jarun011 (03/23/2017)
Women Veterans who have experienced sexual assault may be at increased risk for sexually transmitted infections (STIs). Researchers interviewed women Veterans at two facilities in the VA Midwest Healthcare Network. Of the 996 women interviewed, 51 percent reported past sexual assault, and 32 percent had a history of STIs. Women who had experienced sexual assault were significantly more likely to report a history of STIs. The cause of this correlation is not clear. History of sexual assault should be considered when determining the need for STI screening, say the researchers. (Journal of Women’s Health, March 10, 2017)
|
Rebuilding cartilage using collagen scaffolding
 Photo: Ames Laboratory, U.S. Dept. of Energy (03/23/2017)
British researchers and a collaborator at the Memphis VA Medical Center published work on a new way to promote cartilage regeneration in osteoporosis. Providing a three-dimensional scaffold for cell attachment could help stem cells to form into cartilage. The researchers found that creating a scaffold that mimics the composition and structure of the cartilage in the body promotes this growth. Using collagen type-II and chondroitin sulfate promoted cartilage growth more than other scaffold configurations. The technique could lead to better tissue-engineering treatments for osteoarthritis. (Scientific Reports, March 3, 2017)
|
Functional electrical stimulation helps MS patient walk
 Photo: ©iStock/yodiyim (03/15/2017)
Functional electrical stimulation improved the walking ability of a patient with multiple sclerosis, in a case study by researchers at the Louis Stokes Cleveland VA Medical Center. The patient had lower limb weakness and was frequently unable to take a step unaided. Doctors implanted electrodes into the muscles of his hip, knee, and ankle. The electrodes delivered stimulation that helped activate the muscles in his legs. Over a 90-day trial, he was able to consistently take steps with electrical stimulation. The case study shows that implanted electrical stimulation devices could help restore walking in patients with muscle weakness caused by MS, according to the researchers. (American Journal of Physical Medicine & Rehabilitation, Feb. 1, 2017)
|
ADHD associated with nonsuicidal self-injury
 Photo by Mitch Mirkin (03/15/2017)
Male Veterans with attention deficit hyperactivity disorder (ADHD) were significantly more likely to report nonsuicidal self-injury (NSSI) than those without ADHD, according to a study by VA Mid-Atlantic Health Care Network and Central Texas VA Health Care System researchers. Veterans with PTSD were more likely to have ADHD symptoms than those without PTSD. However, PTSD was not associated with NSSI, contrary to what the researchers expected, based on past studies. The findings show that ADHD may increase the risk of NSSI in male Veterans independent of other factors such as PTSD, say the researchers. (Psychiatry Research, Feb. 24, 2017)
|
Statin use linked to higher odds of diabetes in physically active people
 ©iStock/gilaxia (03/15/2017)
Statin use was associated with double the odds of diabetes and its complications without offsetting cardiovascular benefits, in a VA North Texas Health Care System and University of Texas Southwestern study. The researchers looked at rates of diabetes and cardiovascular outcomes in healthy, physically fit people who were using statins to prevent cardiovascular disease. Statin use is currently recommended for adults 40 to 75 years old with one or more risk factors for cardiovascular disease, such as high cholesterol, diabetes, high blood pressure, or smoking and a calculated risk of heart attack. The researchers found 12.5 percent of statin users and 5.8 percent of nonusers were diagnosed with diabetes. Furthermore, 1.7 percent of statin users and 0.7 percent of nonusers were diagnosed with diabetic complications, such as nerve, kidney, and eye damage. Of the statin users, 1.6 percent had major acute cardiovascular events, compared to 1.5 percent of nonusers. Those rates were much lower than in the general population, but did not show a difference between statin users and nonusers. The researchers concluded that the risks and benefits of statin use in healthy, physically active people may need to be reconsidered. (Journal of Science and Medicine in Sport, Jan. 24, 2017)
|
Smaller changes in cortisol levels linked to better response to PTSD treatment
 ©Stock/marekuliasz (03/09/2017)
Change in cortisol levels during treatment predicted how well patients with PTSD responded to psychotherapy, found researchers at the Atlanta and Ann Arbor VA health care systems. Cortisol is a hormone released by the adrenal gland in response to stress. The researchers measured cortisol in the saliva during treatment of 30 Veterans undergoing either prolonged-exposure or present-centered therapy. They found that patients who had a greater increase in cortisol levels over the course of treatment had less reduction of PTSD symptoms. Contrary to what the researchers expected, overall cortisol levels did not predict how well patients responded to treatment. Modulating patients' hormonal responses may aid their response to treatment, suggest the researchers. (Journal of Clinical Psychiatry, Jan. 17, 2017)
|
Causes of suicide on hospital grounds
 ©Stock/sshepard (03/09/2017)
Researchers with the VA National Center for Patient Safety analyzed the root causes of suicide or suicide attempts on VA hospital grounds and in hospital common spaces and clinic areas (as opposed to patient rooms). They found that the primary causes were breakdowns in communication between patient and staff; the need for improved psychiatric and medical treatment of suicidal patients; and problems with the physical environment, such as unmonitored nonclinical areas. Forty-seven suicides or suicide attempts were reported over a 15-year period. The researchers recommend that hospital staff evaluate the environment for suicide hazards, consider prohibiting firearms (currently, VA facilities nationwide do not allow firearms on their campuses), assist patients who do not have appointments, and promote better communication between staff about high-risk patients. (Journal of Patient Safety, Feb. 22, 2017)
|
Neuroprotective compound may improve brain function after stroke
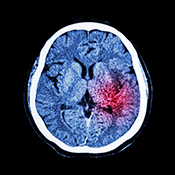 ©Stock/stockdevil (03/09/2017)
The neuroprotective compound P7C3-A20 improved brain function after stroke in rats, found a study by Iowa City VA Health Care System and University of Miami researchers. Rats injected with the compound did better than controls on sensorimotor and cognitive tests. The rats treated with P7C3-A20 also showed significantly less cortical and hippocampal atrophy. They also had improved growth of new nerve tissue. The results suggest that this compound could be useful in protecting the brain from ischemic stroke, say the researchers. (Experimental Neurology, Jan. 8, 2017)
|
More studies needed on the effect of risk factors on multiple sclerosis
 ©iStock/sudok1 (03/02/2017)
Two literature reviews by VA researchers and their associates showed that more research is needed on how risk factors affect multiple sclerosis (MS) progression. One review showed that low vitamin D levels were consistently associated with MS progression, and smoking was associated with more rapid decline in MS disability. However, the different methods and measures used by different studies make it hard to draw conclusions. A second review by the same researchers found that no current risk factor interventions had significant effects on MS progression. More studies are needed on vitamin D supplements, long-term exercise, and smoking cessation, say the researchers. (Multiple Sclerosis Journal, Feb. 1, 2017; Multiple Sclerosis Journal, Feb. 1, 2017)
|
Clinical practice guidelines for low back pain
 ©iStock/ChesiireCat (03/02/2017)
VA researchers were part of an American College of Physicians group that developed recommendations for treating low back pain by reviewing multiple studies published on the topic. They recommend that patients with acute or subacute low back pain should use non-medication treatment such as heat, massage, or acupuncture. If medication is required, clinicians should prescribe nonsteroidal anti-inflammatory drugs or muscle relaxants. Patients with chronic low back pain should be treated without medications whenever possible. If patients do not respond to non-medication treatment, they should be prescribed nonsteroidal anti-inflammatory drugs as first-line therapy, or tramadol (sold as Ultram or Zytram) or duloxetine (sold as Cymbalta) as second-line therapy. Opioids should be an option only after other treatments have proved ineffective and only if potential benefits outweigh risks. (Annals of Internal Medicine, Feb. 14, 2017)
|
New understanding of how white blood cells work
 ©iStock/blueringmedia (03/02/2017)
Researchers with the University of Iowa and Iowa City VA Health Care System found evidence of neutrophil plasticity, or the ability of these cells to change in the body. Neutrophils are the most common type of white blood cell. The concepts of neutrophil plasticity and different neutrophil phenotypes (cells with different structural characteristics) are new; previously, scientists thought that these cells all had similar properties. The researchers exposed neutrophils to H. pylori bacteria, and found that the structure of the nucleus of some neutrophil cells changed after bacterial infection. This demonstrates that the cells can change while still alive. The results could lead to a better understanding of bacterial diseases, particularly how white blood cells fight and interact with infections. (Journal of Immunology, Mar. 1, 2017)
|
Psychotropic medication linked to higher dementia risk in patients with PTSD
 Photo: ©iStock/Kwangmoozaa (02/23/2017)
PTSD by itself has been linked to a higher risk for dementia later in life, but certain medications often used as part of PTSD treatment appear to compound that association. An analysis of data on more than 417,000 Veterans found that those with PTSD who were treated with selective serotonin reuptake inhibitors (SSRIs), novel antidepressants, or atypical antipsychotics were more likely to be diagnosed with dementia, relative to those with or without a PTSD diagnosis but not using any of these drugs. The patients in the study had an average age of 67.7 at the start of the study period, back in 2003, and they were followed, on average, for about 9 years. Those using benzodiazepines or serotonin-norepinephrine reuptake inhibitors (SNRIs) had an increased dementia risk, regardless of whether they had PTSD. The researchers say while it's possible some of the drugs may directly contribute to dementia risk, it's also possible that their use is a marker for more severe PTSD symptoms, or other underlying brain conditions, that may account for the higher dementia risk. They recommend further study. (Journal of the American Geriatrics Society, January 2017)
|
Wii Fit exercise program boosts balance in older adults
 A Veteran receives an explanation of the Wii-Fit from Dr. Kalpana Padala at the Central Arkansas Healthcare System. (Photo by Jeff Bowen) (02/23/2017)
A Wii Fit exercise program improved balance in older adults, found a Central Arkansas Veterans Healthcare System study. Fifteen Veterans participated in an exercise program on the Wii Fit video game for 45 minutes, three days a week for eight weeks. The control group, also including 15 Veterans, performed a computer-based cognitive program. Those in the exercise group scored significantly better than controls on measures of balance. The results show that a Wii Fit exercise program is safe and feasible for community-dwelling older adults with balance problems. (Journal of Aging Research, Feb. 5, 2017)
|
Physical activity counseling improves activity levels at low cost
 Photo: ©iStock/kali9 (02/23/2017)
A physical activity counseling program improved activity levels and gait speed in older Veterans at only a small percentage of patients' health care costs in a VA Mid-Atlantic Health Care Network study. The program included initial in-person exercise counseling, followed by telephone counseling at two, four, and six weeks, and monthly thereafter for one year. The total cost of the program per participant averaged $696, about 6 percent of patients' estimated annual health care costs. The cost of this program may be offset by lower health care costs due to improved physical fitness, but that result was not statistically significant in the study. (Journal of the American Geriatrics Society, January 2017)
|
Thiazide blood-pressure drugs could lower fracture risk
 ©iStock/Sutthaburawonk (02/15/2017)
A certain class of blood pressure medication may improve bone strength in patients with osteoporosis, according to a secondary analysis of data from a larger study involving VA medical centers. Research shows that people with high blood pressure tend to have more osteoporotic fractures. This study showed that patients on chlorthalidone, a thiazide-type medication also sold as Hygroton, had lower risk of hip and pelvic fracture than those on amlodipine (sold as Norvasc) or lisnopril (sold as Zestril). Thiazides are one class of diuretics, or water pills. They increase the amount of water and salt expelled from the body as urine. They also affect the body’s balance of minerals. The results suggest that thiazide-type blood pressure medication could reduce fracture risk in older adults. (JAMA Internal Medicine, January 2017)
|
Transparent clinical notes can build trust with mental health patients
 ©iStock/Steve Debenport (02/15/2017)
Allowing patients in VA mental health care to view clinical notes about their visits with providers can strengthen or strain their trust in those providers, depending on the contents of the notes. Researchers interviewed 28 patients who had access to OpenNotes, allowing them to see what their clinicians wrote about their treatment. The study found that ensuring consistency between what occurs during appointments and what the notes say makes patients trust their clinicians more. Notes that highlight patient individuality and strengths also help create trust. Showing transparency and respect in clinical notes can help build trust with patients, say the researchers. (Psychiatric Services, Feb. 1, 2017)
|
Modest brain changes seen in patients with schizophrenia after computer exercises
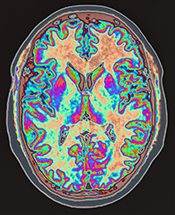 ©iStock/Image Source (02/15/2017)
Patients with schizophrenia showed cognitive improvements after cognitive remediation training in a Minneapolis VA Health Care System study. Cognitive remediation involves computer exercises that place demands on working memory. Patients who received 48 hours of cognitive remediation over a 16-week period showed increased activation of the left prefrontal cortex of the brain, compared with those in the placebo group, who received only basic computer skills training. Increased brain activation, as shown on a type of MRI scan that tracks blood flow, correlated with improved task accuracy and suggests improved neuroplasticity. According to the researchers, the results suggest that brain activation may be an important target for schizophrenia interventions. However, the results were modest, and significant changes were not reported in other areas of the brain, contrary to what the researchers expected. (British Journal of Psychiatry, February 2017)
|
C. difficile treatment with vancomycin results in fewer deaths than treatment with metronidazole
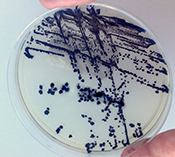 ©iStock/Scharvik (02/09/2017)
The antibiotic vancomycin reduced the risk of death after C. difficile infection over another antibiotic, metronidazole, found a study of VA health care system data. In recent decades, C. difficile infection has become a major cause of death inside and outside of hospitals. Metronidazole is the most common drug used to treat C. difficile. While C. difficile recurrence rates were similar with both drugs, this study showed that those treated with vancomycin were less likely to have died than those treated with metronidazole within 30 days after treatment. The findings justify vancomycin as initial therapy for C. difficile infection, according to the researchers. (JAMA Internal Medicine, Feb. 6, 2017)
|
Unique challenges of delivering primary care to women Veterans
 ©iStock/javi_indy (02/09/2017)
VA's Patient Aligned Care Team (PACT) initiative faces unique challenges in delivering care to women Veterans, according to a VA Greater Los Angeles Health Care System study. The researchers interviewed 73 primary care providers and other staff about the benefits and difficulties of providing PACT care to women Veterans. Those interviewed said that PACT improved continuity of care and helped nursing staff practice effectively. Problems included inconsistent implementation of PACT procedures, short staffing, and space constraints. Challenges unique to the care of women Veterans included more psychosocial needs, the need for specialized training for staff, and inadequate staffing due to a separation between woman's health and primary care services. (Women's Health Issues, Jan. 4, 2017)
|
Clock-in-the-Box test helps predict return home after hospital stay
 ©iStock/monkeybusinessimages (02/09/2017)
The Clock-in-the-Box (CIB) test is effective at predicting whether older patients will return home after hospitalization, suggests a new study. The CIB is a brief cognitive screening measure that assesses memory and executive functions. This VA Boston Healthcare System study found that every unit of increase on the CIB was associated with a lower likelihood of being discharged to somewhere other than home, such as a nursing home or rehabilitation center. The results support the CIB as a tool to inform clinical treatment decisions and discharge planning, say the researchers. (Clinical Interventions in Aging, Nov. 11, 2016)
|
E. coli contamination widespread in U.S. chicken
 Photo: ©iStock/MikeyGen73 (02/02/2017)
Antibiotic-resistant E. coli contamination is widespread in commercial U.S. chicken meat, found a study that included Minneapolis VA Health Care System researchers. Many of the strains of E. coli found in chicken do not respond to antibiotics. This means that it can be much harder to treat people infected with E. coli from eating chicken. Organic chicken breasts had slightly lower levels of antibiotic resistance, but had just as strong E. coli contamination as non-organic chicken. The study, conducted in 2013, suggests retail chicken products in the U.S. pose a potential health threat to consumers even if they are labeled as organic. Food-safety experts say thorough cooking kills the bacteria in meat, but consumers don’t always follow guidelines. (Applied and Environmental Microbiology, Jan. 6, 2017)
|
Compound improves cognitive function after stroke
 Photo: ©iStock/FikMik (02/02/2017)
A chemical compound called P7C3-A20 could help improve cognitive function after stroke. When given to rats, P7C30-A20 protected existing neurons from atrophy and promoted the regeneration of new neurons in the brain. The rats treated with P7C30-A20 performed better than controls on movement and memory tests after seven days. The researchers also found decreased cortical and hippocampal atrophy in the treated rats. This study suggests that P7C3 compounds may be useful in protecting the brain from stroke. This study was conducted by researchers with the University of Miami, University of Iowa, and Iowa City VA Health Care System. (Experimental Neurology, Jan. 8, 2017)
|
Review of significant infectious-disease research cites key VA study
 Photo: ©iStock/AlexRaths (02/02/2017)
A recent review of infectious-disease research selected a 2015 VA study as contributing significantly to the field. The VA study, published in the journal Clinical Infectious Diseases, looked at the effectiveness of two drugs in fighting vancomycin-resistant Entrerococcus bloodstream infections (VRE-BSIs), bacterial infections that resist treatment with common antibiotics. The study found that treatment with the antibiotic linezolid resulted in significantly higher treatment failure than treatment with daptomycin. Linezolid treatment was also associated with a higher rate of mortality in the study group. According to the researchers, the results show that daptomycin is a better choice than linezolid for treating VRE-BSIs. (American Journal of Health-System Pharmacy, Feb. 15, 2017)
|
New evidence on how aspirin may help prevent cancer
(01/26/2017)
Researchers with the Michael E. DeBakey VA Medical Center and University of Texas may have found why aspirin can help prevent and treat some cancers. Scientists have long known that taking aspirin can lower the risk of certain cancers and stop the spread of cancer cells, but how this works is not well understood. The new research suggests that aspirin stops platelets from interacting with cancer cells, which affects cancer growth. The researchers further found that a new type of aspirin (based on lipid molecules) may be even more effective at preventing cancer. (Cancer Prevention Research, Dec. 20, 2016)
|
Protein in lungs could be target for asthma drugs
 Photo: ©iStock/yodiyim (01/26/2017)
Targeting asthma drugs to a specific protein (HIF-1alpha) in the lungs could help limit airway inflammation, according to a VA San Diego Healthcare System study. A drug to inhibit HIF-1alpha in mice led to less allergic inflammation in the airway, although the response varied based on genetic factors. Asthma can be caused by different genetic variants, and current therapies are limited in their effectiveness. The researchers suggest HIF-1alpha inhibitors may be a way to effectively target certain forms of the disorder. (Clinical Immunology, Jan. 13, 2017)
|
Pay-for-performance has limited effect on health care
 Photo: ©iStock/simarik (01/26/2017)
Pay-for-performance programs may improve health care procedures, but evidence does not show that they improve patient outcomes. Pay-for-performance programs give financial rewards or penalties to health care providers and institutions according to their performance on quality measures. A literature review found some evidence that these programs improve the processes that institutions use, but this evidence was low-strength and somewhat contradictory. The review found no evidence that these programs improve patient outcomes. (Annals of Internal Medicine, Jan. 10, 2017)
|
Few Veterans with moderate or severe TBI go back to work
 Photo: ©iStock/lentolo (01/18/2017)
Few service members and Veterans with moderate to severe traumatic brain injury (TBI) return to work one year after their injury, according to a VA Polytrauma Rehabilitation Centers study. In a study of 293 Veterans and service members, only 21 percent were employed one year after a TBI. Those who were older, were minorities, or had a more severe TBI were more likely to be unemployed. Every additional year of age was linked to a 2 percent decrease in employment likelihood. Eighty-three percent of minorities were unemployed after one year, compared with 76 percent of nonminorities. Eighty-five percent of subjects with severe TBI were unemployed, while only 63 percent of subjects with moderate TBI were unemployed. These results will help VA plan rehabilitation services, say the researchers. (Journal of Head Trauma Rehabilitation, Jan. 5, 2017)
|
Rewards can push older adults to walk more
 Photo: ©iStock/FatCamera (01/18/2017)
Older adults were more likely to meet daily step goals when they received reward money or had money donated to charity for reaching those goals. Study participants were challenged to increase their daily step counts by 50 percent. Those who were offered a reward of $20, a $20 donation to the charity of their choice, or a combination of the two were more likely to meet the step goal than those who were offered only feedback during a 16-week period. According to the researchers, incentives such as these could be used to get older adults to walk more. (American Journal of Preventive Medicine, Jan. 3, 2017)
|
Toxic exposures common in recent wars
 Photo: Airman 1st Class Christopher Griffin/USAF (01/18/2017)
A study of 224 Iraq and Afghanistan Veterans found that 97.2 percent were exposed to toxic hazards during deployment. Toxic exposure was associated with chronic multisymptom illness (CMI) symptoms in these Veterans. The most common type of toxic exposure was breathing in smoke or fumes. Pesticide exposure was the most likely predictor of CMI. More analysis is needed on specific toxic hazards Veterans face and the relationship with CMI in order to improve prevention, say the researchers. (Journal of Occupational and Environmental Medicine, January 2017)
|
Sunlight improves function of immune cells
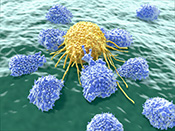 Photo: ©iStock/selvanegra (01/12/2017)
Researchers at the Washington DC VA Medical Center, Georgetown University, and Vinh University in Vietnam found a mechanism that may explain why sunlight can reduce instances of autoimmune disease and some cancers, as shown in past research. Through experiments with human cells and mouse tissue, they found that T cells within skin are naturally sensitive to blue light. T cells serve an important purpose in the immune system and help the body adapt to disease. Blue light, which is absorbed by the skin from sunlight, appears to improve the movement of T cells within the body, which benefits the immune system. Scientists have long known that sunlight can have positive effects on the immune system, but were not sure why. (Scientific Reports, Dec. 20, 2016)
|
Multiple medical conditions linked to arthritis-causing disease
 Photo: ©iStock/bloodstone (01/12/2017)
Researchers looked at a large Veteran population to identify other conditions associated with calcium pyrophosphate crystal deposition disease (CPDD), a common cause of arthritis. They found that people with CPDD had high rates of hyperparathyroidism, gout, osteoarthritis, rheumatoid arthritis, hemochromatosis, hypomagnesemia, and chronic kidney disease. These patients also tend to take calcium supplements, the study found. The use of common high blood pressure and heartburn medicines was not associated with CPDD. Knowing these links could help doctors develop treatment strategies for CPDD. (Arthritis Care & Research, Nov. 29, 2016)
|
Health-promoting behaviors may reduce suicidal thoughts in Veterans with PTSD
 Photo: ©iStock/PeopleImages (01/12/2017)
A survey of more than 100 Iraq and Afghanistan Veterans found that those who participated in health-promoting behaviors had a lower rate of suicidal thoughts. Research shows that Veterans with PTSD are more likely to have suicidal thoughts. But the link was less pronounced among those in the study with PTSD who said they routinely engaged in activities to foster good nutrition, physical activity, stress management, spiritual growth, health responsibility, and interpersonal relationships. The researchers say promoting these activities in Veterans with PTSD could help lower suicide risk. (PLoS One, Dec. 21, 2016)
|
High-protein diet linked to lower bone risk
 Photo ©iStock/stock colors (01/05/2017)
Older men who eat more protein have a lower risk of broken bones, according to a recent study. The study looked at 5,875 men over 15 years. Those with more protein in their diet had fewer broken bones than those who ate less protein, and the source of protein also mattered. More protein from dairy and other animal sources (meat, fish, poultry, eggs) was linked to lower hip fracture risk, while protein from plants (such as legumes, grains, and nuts) was not. Higher protein was tied to fewer hip fractures but not fewer spine fractures, showing this connection might vary by body part. While the study focused only on men, and by itself does not prove a direct causal link between protein intake and bone strength, the researchers nonetheless suggest that adding one to two servings per day of protein-rich foods may help older adults cut fracture risk. (Journal of Bone and Mineral Research, Dec. 12, 2016)
|
Intensive outpatient program did not lower health care cost or use
 Photo ©iStock/shironosov (01/05/2017)
Intensive outpatient care resulted in health care use and costs that were similar to those of standard care in a VA Palo Alto Health Care System study. The study compared 433 high-need patients in standard Patient Aligned Care Team (PACT) care with 150 patients in an Intensive Management program (ImPACT). Patients in ImPACT receive extra outpatient care, including tracking goals and priorities, care management for medical and social service needs, and coordination between VA and non-VA providers. Patients in both programs had similar costs and numbers of hospital visits. Those in the ImPACT group were slightly more satisfied with VA care. These results were surprising—the researchers expected ImPACT to reduce care utilization and cost. (JAMA Internal Medicine, Dec. 27, 2016)
|
'Safety huddles' ease risks linked to electronic health records
 Photo ©iStock/sturti (01/05/2017)
"Safety huddles" can help limit safety risks related to electronic health records (EHRs), found a VA study. These risks include mislabeled medicine, data loss due to computers not working, and incorrect treatment doses. One medical center used a daily meeting of care providers and support staff to discuss safety concerns and "great catches" of potential problems. Over 249 meetings, they were able to identify and address 245 EHR-related safety concerns. The study authors recommend that health care systems use huddles to help improve EHR use. (Journal of the American Medical Informatics Association, Dec. 28, 2016)
|
Study compares infection control in VA, non-VA nursing homes
 Photo: ©iStock/Wavebreak (12/29/2016)
VA and non-VA nursing homes differed in their approach to catheter-associated urinary tract infections, according to a recent study. VA nursing homes reported more hours per week devoted to infection prevention, were more likely to have committees to review infection policies, had higher physician and nurse staffing-to-bed ratios, had higher percentages of 24-hour registered nurse supervision, and kept track of catheter-associated urinary tract infection rates more regularly, compared with non-VA nursing homes. Most VA nursing homes also had infection prevention programs integrated within VA acute-care programs. A lower percentage of VA nursing homes had policies on appropriate catheter use, compared with non-VA nursing homes. The authors suggest that universal practices should be adopted in both VA and non-VA nursing homes. (Infection Control and Hospital Epidemiology, online Dec. 5, 2016)
|
How do the experiences of U.S. and Australian Veterans compare?
 Photo courtesy of Australian Army (12/29/2016)
A recent comparison based on data from VA and the Australian Department of Veterans’ Affairs showed several differences in post-1990 deployment outcomes. The U.S. deployed significantly more personnel than Australia during this period. Veterans from the two countries had similar overall rates of PTSD. Gulf War Veterans from both countries had a reduced risk of suicide, compared with the general population, but U.S. Veterans of Iraq and Afghanistan had higher rates of suicidal thoughts. U.S. Gulf War Veterans had higher rates of multisymptom illness than Australians, and were also more likely to have been in combat. The two countries’ health care systems were alike in terms of their range of services, focus on mental health, and increasing use of technology, but different in some aspects of service provision and financial structure. (Australian DVA website, Dec. 14, 2016)
|
Concerns about falling not linked to low blood pressure
 Photo: ©iStock/ Imagesbybarbara (12/22/2016)
In one of the latest findings to be reported from a major study on high blood pressure treatment that was funded by the National Institutes of Health and involved VA researchers, fear of falling was not associated with low blood pressure or with blood pressure medication use in older adults. While participants with more concern about falling were found to be taking more medicine to combat high blood pressure, the study did not find a link between actual low blood pressure due to medication use and fear of falling. Fear of falling is common in older adults with high blood pressure who take medication to manage the condition. Many do not wish to increase their dose because they fear medication-induced low blood pressure will increase their risk of falling. The researchers point out that it is important to address patients’ fear of falling, in addition to actual fall risk. (Journal of the American Geriatrics Society, November 2016)
|
Virtual training for staff helps prevent pressure ulcers
 Photo: ©iStock/ Johnny Greig (12/22/2016)
A new training program decreased the rate of pressure ulcers in VA. The Virtual Breakthrough Series (VBS) is a teleconferencing and email-based training program that uses personalized coaching and group education to help staff implement care changes to prevent pressure ulcers in patients. After the project was implemented, the pressure ulcer rate dropped from 1.2 to 0.9 per 1,000 bed days of care. VBS has previously been used to prevent catheter-associated urinary tract infections and to prevent falls. The researchers say that together, these studies show that VBS could be a powerful tool to improve the quality and safety of care in VA. (Journal of Nursing Care and Quality, online Nov. 29, 2016)
|
Veterans show no health effects of uranium exposure 25 years later
 Photo courtesy of www.gulflink.osd.mil (12/22/2016)
Gulf War Veterans wounded in depleted uranium friendly-fire incidents showed no uranium-related health effects 25 years after exposure. Veterans with embedded uranium fragments had elevated urine uranium concentrations, while those who had been exposed to uranium through inhalation had lower urine uranium concentrations. Although these Veterans did not show any negative health effects, metal fragments still in their bodies continue to expose them to uranium radiation, and dangerous concentration thresholds may still be reached. The researchers recommend continued health surveillance for this group. (Environmental Research, January 2017)
|
AspireAssist device leads to greater weight loss
(12/14/2016)
Patients equipped with the AspireAssist System, a tube placed in the stomach that allows stomach contents to be drawn out, lost more weight than patients who received only lifestyle counseling. In a year-long study in obese patients, patients who received both lifestyle counseling and the AspireAssist lost an average of 12.1 percent of their body weight, compared with a 3.5 percent loss for patients who only received counseling. This treatment could prove effective for long-term treatment of obesity, according to the study authors. It should be noted that the company that makes the device funded the study, which involved the San Diego VA and numerous university sites, and was involved with analyzing the data and preparing the manuscript. (American Journal of Gastroenterology, Dec. 6, 2016)
|
HIV increases risk for lung cancer
(12/14/2016)
HIV infection could contribute to the development of lung cancer, according to a study of participants in the Veterans Aging Cohort Study. Chronic inflammation and a dysfunctional immune system, both associated with HIV, are two factors that could increase the cancer risk, say the researchers. The study also showed that patients with lower T-cell counts were more likely to develop lung cancer. These findings could be used to target lung cancer prevention to this high-risk group, say the researchers. (The Lancet HIV, Dec. 2, 2016)
|
TeleMOVE is an effective weight-loss program
(12/14/2016)
A VA San Diego Healthcare System study found that participants in a VA telehealth weight-loss program lost more weight than those in the in-person program. Participants in the new TeleMOVE program lost an average of 8.6 pounds during the 90-day program, while those who attended the MOVE! in-person weight-loss classes lost an average of 4.5 pounds over the course of eight classes. Participants who adhered to the program lost more weight than those who missed sessions, regardless of which program they were in. (Obesity Research & Clinical Practice, Dec. 5, 2016)
|
Can neurocognitive function predict suicide?
 Photo: ©iStock/efks (12/08/2016)
A study of Army administrative data found an association between decreased neurocognitive functioning and suicide in soldiers. Researchers found that lower scores on a computerized test of neurocognitive functioning—including problems in decision-making, problem-solving, verbal fluency, and memory—were linked to suicide attempts or death and suicidal thoughts in the following 12 months. The study showed more suicide attempts in soldiers who were female, less educated, white non-Hispanic, and younger at the time of testing, and who had a mental health diagnosis before testing. The researchers say that neurocognitive testing may be a useful tool in predicting future risk of suicide. (Suicide & Life-Threatening Behavior, Nov. 1, 2016)
|
Military sexual trauma linked to mental health problems in transgender Veterans
(12/08/2016)
Military sexual trauma (MST) is associated with mental health problems in transgender Veterans. A study of 332 transgender Veterans who served in Iraq and Afghanistan found that MST was associated with likelihood of PTSD and personality disorder for both men and women, and with bipolar disorder and depressive disorder for women. Fifteen percent of the Veterans included in the study had experienced MST. The researchers conclude that medical forms should include gender identity in addition to biological gender, and that MST treatment should be culturally competent. (Journal of Traumatic Stress, December 2016)
|
Nanoparticle may aid in bladder cancer diagnosis, treatment
 (Photo courtesy of Pan lab) (12/08/2016)
Researchers have developed a nanoparticle that promises to help in the diagnosis and treatment of bladder cancer. The particle, called PLZ4-nanoporphyrin (PNP), emits fluorescent light when exposed to infrared light. By coating PNP with a molecule specific to bladder cancer, researchers were able to identify cancer cells with the light and diagnose the condition in mice. PNP was also shown to be able to release chemotherapy drugs, as well as photodynamic and photothermal treatment agents, slower and more effectively than other methods. While this new technique of bladder cancer diagnosis and treatment has been shown to work so far only in mice, the researchers believe it could easily be adapted to individualized medicine in a clinical setting. (Biomaterials, October 2016)
|
Educational intervention targets racial gaps in use of knee replacements
(12/01/2016)
African American patients who were shown an informational video about knee replacement surgery were 85 percent more likely than those who did not view the video to undergo the surgery, according to a study by researchers at the Philadelphia VA Medical Center and their partners. African Americans are significantly less likely than whites to have knee replacement surgery to relieve pain from arthritis, largely due to lack of knowledge about the treatment. The rate at which doctors recommended knee replacement was higher for those who viewed the video, but this result was not statistically significant. The researchers say that this low-cost, patient-centered intervention could increase use of an effective orthopedic procedure among minority patients. (JAMA Surgery, Nov. 23, 2016)
|
Telehealth versus in-person therapy for chronic pain
(12/01/2016)
Video teleconferencing can be just as effective as in-person treatment for patients in acceptance and commitment therapy (ACT), a psychological approach that can be used to help people deal with chronic pain. This study found that Veterans receiving the therapy both in person and by video teleconferencing showed significant improvements in pain interference, pain severity, mental and physical health-related quality of life, pain acceptance, activity level, depression, and pain-related anxiety. The results suggest that teleconferencing is an acceptable way to deliver the therapy, although more participants in the teleconferencing group withdrew from the treatment than in the in-person group. (Journal of Pain, Nov. 9, 2016)
|
Pedestrian pathway roughness thresholds for wheelchair user safety and comfort
 Photo: ©iStock/ands456 (12/01/2016)
Researchers at the Human Engineering Research Laboratories, a program of VA and the University of Pittsburgh, studied what level of roughness was acceptable for pedestrian pathways to avoid harmful vibrations and discomfort for wheelchair users. The researchers looked at previous studies on possible health effects of vibrations and engineering studies of wheel displacement when rolling over various surfaces, as well as surveys of wheelchair users about surfaces that cause discomfort. They found that a pathway roughness index threshold of < 50 millimeters per meter for a 100-meter-long surface and ?100 mm/m for a 3-meter-long surface would protect wheelchair users against discomfort and possible health risks. Finding these thresholds is important because current standards are not clear, according to the researchers. (>Assistive Technology, Sept. 2, 2016)
|
Blood pressure variability leads to vascular problems
(11/18/2016)
High blood pressure variability is linked to vascular problems in non-elderly people with diabetes. Variability in systolic blood pressure could be a sign of blood flow instability. A study of more than 200,000 patients tracked for more than three years in the VA health care system found that patients with the highest variability in systolic blood pressure had a 19 percent higher risk of microvascular complications than those with less varied blood pressure. Neuropathy (nerve damage) was 30 percent more likely, and retinopathy (disease of the retina that leads to vision problems) was 17 percent more likely for this group. (Journal of Diabetes and its Complications, Sept. 14, 2016)
|
Quality of care for diabetes and cardiovascular disease
(11/18/2016)
A recent study found that quality of care for diabetes and cardiovascular disease in the VA health care system was comparable between physicians and advanced-practice providers, although a majority of patients did not meet measures of proper disease risk-factor control. Advanced-practice providers include nurse practitioners and physician assistants. Regardless of provider type, there is a need within VA to improve risk-factor control in patients with diabetes and cardiovascular disease, say the researchers. (American Heart Journal, November 2016)
|
The hippocampus' role in memory
(11/17/2016)
A VA San Diego Healthcare System study suggests that the hippocampus is particularly important for linking and ordering events in memory. Patients with brain injury involving the hippocampus remembered fewer details than controls about events right after they occured. However, injured patients and controls remembered about the same amount of details when questioned one month after the event. The patients with hippocampal damage had no trouble remembering spatial details such as locations, but they were noticeably worse than controls at remembering details related to time and event sequence. (Proceedings of the National Academy of Sciences of the United States of America, Nov. 7, 2016)
|
Statins decrease progression of liver disease
(11/10/2016)
Statins, drugs frequently prescribed to treat high cholesterol, may slow the progression of liver disease in patients with both HIV and hepatitis C, according to a study of VA electronic medical records. Infection with both HIV and hepatitis C carries increased risk of cirrhosis, hepatocellular carcinoma, and death. This study showed that patients with these diseases who were also on statins had a 32-percent decreased risk of developing cirrhosis, possibly due to statins' anti-inflammatory properties. (AIDS, Oct. 23, 2016)
|
Racial differences in knee replacement surgeries
(11/10/2016)
Black Veterans were less likely than white Veterans to undergo knee replacement surgery, according to data from the VA Musculoskeletal Disorders Cohort. Over a 10-year period, rates of knee replacements were much lower for black than white veterans. Hispanic Veterans had the same rates of knee replacement as white Veterans. This study shows the importance of developing ways to reduce racial differences in Veteran health care usage, say the researchers. (Arthritis Care & Research, Oct. 27, 2016)
|
Heart rate variability as a predictor of PTSD
(11/02/2016)
Lower pre-deployment heart rate variability (HRV) can predict higher post-deployment PTSD symptom severity, according to a study of 343 Army National Guard soldiers. The results suggest that people with lower HRV, meaning fewer changes in the time between heart beats, are at higher risk for PTSD. This may be because lower HRV is associated with a reduced ability of the body to adapt to changing social or environmental demands. One caveat: The results were significant only in soldiers who scored above a cut-off score on a PTSD symptom test pre-deployment. (Biological Psychology, Oct. 20, 2016)
|
Internet-based smoking cessation programs
(11/02/2016)
Internet-based smoking cessation programs may be an effective way to reduce smoking in Veterans, found a Durham VA Medical Center study. Veterans offered telehealth programs to help them quit smoking had about the same quit rates as those participating in smoking cessation programs in the clinic. Reach of the internet intervention was significantly higher than the in-person program: 50 percent of those assigned to the internet group registered for a smoking cessation program, while only 19 percent of those in the in-person group attended a clinic-based session. Results suggest that using electronic medical records to identify smokers and offering novel interventions—such as online programs—to help them quit can significantly reduce smoking in the Veteran population. (Journal of Substance Abuse Treatment, October 2016)
|
Antibiotic prescription trends
(11/02/2016)
Antibiotic prescription decreased for physicians and dentists but increased for nurse practitioners and physician assistants—so-called midlevel providers—over a six-year period, according to a recent study. Over-prescribing of antibiotics can lead to drug-resistant bacteria. Midlevel providers were particularly likely to prescribe broad-spectrum antibiotics, which are a major part of the problem. The researchers recommend efforts to reverse the trend. (Journal of the American Pharmacists Association, Oct. 8, 2016)
|
Depression risk factors among lung cancer patients
(10/27/2016)
The main risk factors for depression among patients with lung cancer are younger age, female sex, low income, not being married, and being a smoker, found a study involving 15 VA medical centers. Researchers suggest that these risk factors should be monitored closely in this population. Patients with depression in this group had worse health-related quality of life, vitality, cancer-specific symptoms, and social support, although the study showed increased mortality only among patients with more lung cancer symptoms or less social support. (Lung Cancer, October 2016)
|
New technique to test Alzheimer's disease drugs
(10/27/2016)
Researchers at the Edith Nourse Rogers Memorial Veterans Hospital in Bedford, Massachusetts, have demonstrated a new way to test Alzheimer's disease drugs in lab models. They used stem cells from patients' blood to create 3D cell cultures of brain tissue, and were able to measure drug penetration on the sample. Modeling Alzheimer's disease in the lab is hard because of the extremely complex anatomy of the brain, but new drugs need to be tested this way before they are used in humans. This new approach with 3D cell cultures could allow scientists to test drugs more accurately than in traditional 2D cultures by more closely modeling the biology of the brain. (PLOS ONE, Sept. 29, 2016)
|
Liver transplant outcomes after circulatory death
(10/27/2016)
Liver transplants from younger donors after circulatory death had better outcomes than those from older donors after brain death, found researchers with the University of Wisconsin and William S. Middleton Memorial Veterans Hospital. Liver donation after circulatory death is generally considered to have worse outcomes than donation after brain death. However, this study showed that livers from circulatory death donors younger than 50 fared better than those from brain death donors older than 60. The researchers suggest that more liver donations after circulatory death should be accepted, which could lead to shorter transplant wait times. (Liver Transplantion, September 2016)
|
Personal stories more engaging for hypertension management
(10/17/2016)
African-American Veterans felt more engaged when viewing interventions about hypertension management that included personal stories from other Veterans, compared with information-only interventions. The study included 618 African-American Veterans with uncontrolled hypertension from three VA medical centers. One group was shown a DVD of information about hypertension, while another was shown a DVD featuring other African-American Veterans telling stories about successfully managing their hypertension. The Veterans who watched real patients tell their stories were more emotionally engaged than the other group and more likely to report intentions to change their behavior, showing that personal stories may be an effective tool to teach patients how to manage their condition. (Patient Education and Counseling, September 2016)
|
No objective benefits of yoga or aerobic exercise on sleep in midlife women
(10/17/2016)
A study found no objective effects of yoga and aerobic exercise on sleep in menopausal women with hot flashes. Although yoga and exercise have been suggested as useful for midlife women experiencing sleep disturbances, researchers found no significant differences in sleep patterns between those who practiced yoga or exercise and those who did not. The researchers used actigraphy—the continuous measurement of movement to track periods of sleep and wakefulness. While some women reported small sleep improvement after yoga or exercise, these effects could not be objectively measured. (Journal of Clinical Sleep Medicine, Sept. 9, 2016)
|
PTSD therapies are still effective in presence of TBI
(10/17/2016)
Both prolonged exposure (PE) and cognitive processing therapy (CPT) are effective treatments for Veterans with PTSD regardless of traumatic brain injury (TBI) status, according to a Salem (Virginia) VA Medical Center study. PE therapy involves emotionally reliving trauma in a safe and controlled manner. CPT focuses on evaluating and changing upsetting thoughts. Some clinicians have been reluctant to use PE for patients with both PTSD and TBI out of fear that they would be less able to tolerate the therapy or that cognitive limitations would make the therapy less effective. A previous study showed that Veterans with PTSD and TBI could benefit from PE. The current study showed that the presence or absence of traumatic brain injury did not change the effectiveness of either therapy and that PE provided greater PTSD symptom reduction than CPT. The researchers note important limitations to this study, including that it was not a randomized trial and the sample size was small. (Journal of Traumatic Stress, October 2016)
|
Aortic aneurysm repair
(10/10/2016)
Two procedures to repair aneurysms (widening of an artery that could rupture and cause internal bleeding) in the aorta have similar health and cost outcomes, according to a multicenter VA study. One procedure involves open surgery to repair the aorta. In the other, called endovascular repair, a surgeon uses X-rays to thread a stent through the arteries to the damaged part of the aorta. Researchers found that survival, quality of life, and costs were not significantly different between these two procedures. Selection of either procedure can be guided by patient and physician preference, say the researchers. (JAMA Surgery, Sept. 14, 2016)
|
Disclosing adverse surgical events
(10/10/2016)
Fully disclosing adverse effects to patients after surgery benefits both patients and surgeons. To study how often surgeons fully shared details with patients and their family, investigators surveyed surgeons at three VA medical centers. They found that after a negative event, most surgeons were likely to explain why the event happened, express regret and concern for the patient's welfare, disclose the event within 24 hours, and discuss steps taken to treat any subsequent problems. Fewer surgeons were likely to apologize to patients or discuss whether the event was preventable and how recurrences could be prevented. Surgeons who were less likely to disclose details were more likely to experience negative effects such as anxiety. The researchers believe better understanding surgeons' attitudes and experiences can help ensure full and open disclosure to patients and their families. (JAMA Surgery, July 20, 2016)
|
New device for self-administered pain relief after upper-limb injury
(10/10/2016)
Patient-controlled analgesia (PCA) allows patients to manage their own pain while being treated in hospitals. However, Veterans and service members with limb dysfunction or loss are often not able to use these devices. This problem led to the design of a new PCA adapter for patients with severe upper-limb injuries. The new device features a large surface area that fits around traditional PCA equipment, allowing for easier use. Initial case studies show that patients and clinicians were happy with the device, which could improve treatment and functional independence of Veterans and service members with upper-limb injuries. (Military Medicine, August 2016)
|

 Photo: ©iStock/Kuzmik_A
Photo: ©iStock/Kuzmik_A Photo: ©iStock/donfiore
Photo: ©iStock/donfiore Photo: ©iStock/Moyo Studio
Photo: ©iStock/Moyo Studio Photo: ©iStock/Panuwat Dangsungnoen
Photo: ©iStock/Panuwat Dangsungnoen Photo: ©iStock/Giselleflissak
Photo: ©iStock/Giselleflissak Photo courtesy of DVIDS.
Photo courtesy of DVIDS. Photo: ©iStock/FatCamera
Photo: ©iStock/FatCamera Photo: ©iStock/peterspiro
Photo: ©iStock/peterspiro Photo: ©iStock/Emilia Kohn
Photo: ©iStock/Emilia Kohn Photo: ©iStock/Zhang Rong
Photo: ©iStock/Zhang Rong Photo: ©iStock/Hailshadow
Photo: ©iStock/Hailshadow Photo: ©iStock/rdegrie
Photo: ©iStock/rdegrie Photo: ©iStock/yacobchuk
Photo: ©iStock/yacobchuk Photo: ©iStock/Fly View Productions
Photo: ©iStock/Fly View Productions Photo: ©iStock/mediamasmedia
Photo: ©iStock/mediamasmedia Photo: ©iStock/FG Trade
Photo: ©iStock/FG Trade Photo for illustrative purposes only. ©iStock/ArtistGNDphotography
Photo for illustrative purposes only. ©iStock/ArtistGNDphotography Photo: ©iStock/LittleCityLifestylePhotography
Photo: ©iStock/LittleCityLifestylePhotography Photo: ©iStock/dem10
Photo: ©iStock/dem10 Photo: Photo: ©iStock/Domepitipat
Photo: Photo: ©iStock/Domepitipat Photo: ©iStock/metamorworks
Photo: ©iStock/metamorworks Photo: ©iStock/Zinkevych
Photo: ©iStock/Zinkevych Photo: ©iStock/EmirMemedovski
Photo: ©iStock/EmirMemedovski Image: ©iStock/mustafahacalaki
Image: ©iStock/mustafahacalaki Photo: ©iStock/Ole Schwander
Photo: ©iStock/Ole Schwander Photo: ©iStock/Wavebreakmedia
Photo: ©iStock/Wavebreakmedia Photo: ©iStock/Chaichan Pramjit
Photo: ©iStock/Chaichan Pramjit Photo: ©iStock/FatCamera
Photo: ©iStock/FatCamera Photo: ©iStock/mikkelwilliam
Photo: ©iStock/mikkelwilliam Photo: ©iStock/Dragos Condrea
Photo: ©iStock/Dragos Condrea Photo: ©iStock/Zinkevych
Photo: ©iStock/Zinkevych Photo: ©iStock/SDI Productions
Photo: ©iStock/SDI Productions
 Photo: ©iStock/SDI Productions
Photo: ©iStock/SDI Productions  Photo: ©iStock/Wavebreakmedia
Photo: ©iStock/Wavebreakmedia  Photo: ©iStock/Liudmila Chernetska
Photo: ©iStock/Liudmila Chernetska  Photo: ©iStock/Doucefleur
Photo: ©iStock/Doucefleur Photo: ©iStock/Renata Angerami
Photo: ©iStock/Renata Angerami Photo: ©iStock/Delmaine Donson
Photo: ©iStock/Delmaine Donson Photo: ©iStock/FatCamera
Photo: ©iStock/FatCamera Photo: ©iStock/Yulia Gusterina
Photo: ©iStock/Yulia Gusterina Photo: ©iStock/haydenbird
Photo: ©iStock/haydenbird Photo: ©iStock/zabelin
Photo: ©iStock/zabelin Photo: ©iStock/utah778
Photo: ©iStock/utah778 Photo: ©Vanessa Nunes
Photo: ©Vanessa Nunes Photo: ©iStock/DragonImages
Photo: ©iStock/DragonImages U.S. Army photo by Paolo Bovo.
U.S. Army photo by Paolo Bovo. Photo: ©iStock/Vadym Terelyuk
Photo: ©iStock/Vadym Terelyuk Photo: ©iStock/-zlaki-
Photo: ©iStock/-zlaki- Photo for illustrative purposes only. ©iStock/Svitlana Hulko
Photo for illustrative purposes only. ©iStock/Svitlana Hulko Photo: ©iStock/gchutka
Photo: ©iStock/gchutka Photo: ©iStock/pixelfusion3d
Photo: ©iStock/pixelfusion3d Photo: ©iStock/Ake Ngiamsanguan
Photo: ©iStock/Ake Ngiamsanguan Photo: ©iStock/AndreyPopov
Photo: ©iStock/AndreyPopov Photo: ©iStock/Siarhei Khaletski
Photo: ©iStock/Siarhei Khaletski Photo: ©iStock/Ridofranz
Photo: ©iStock/Ridofranz Photo: ©iStock/Wirestock
Photo: ©iStock/Wirestock Photo: ©iStock/andreswd
Photo: ©iStock/andreswd Photo: ©iStock/ljubaphoto
Photo: ©iStock/ljubaphoto Photo courtesy of Dr. Noah Philip
Photo courtesy of Dr. Noah Philip Photo: ©iStock/Kobus Louw
Photo: ©iStock/Kobus Louw Photo: ©iStock/Christoph Burgstedt
Photo: ©iStock/Christoph Burgstedt Photo: ©iStock/Edwin Tan
Photo: ©iStock/Edwin Tan Photo: ©iStock/peakSTOCK
Photo: ©iStock/peakSTOCK Photo: ©iStock/Alexander Shelegov
Photo: ©iStock/Alexander Shelegov Photo for illustrative purposes only. ©iStock/DisobeyArt
Photo for illustrative purposes only. ©iStock/DisobeyArt Photo: ©iStock/BlackJack3D
Photo: ©iStock/BlackJack3D Photo: ©iStock/radub85
Photo: ©iStock/radub85 Photo: ©iStock/golfcphoto
Photo: ©iStock/golfcphoto Photo: ©iStock/Shidlovski
Photo: ©iStock/Shidlovski Photo: ©iStock/yavorskiy
Photo: ©iStock/yavorskiy Photo for illustrative purposes only. ©iStock/Jovanmandic
Photo for illustrative purposes only. ©iStock/Jovanmandic Photo: ©iStock/Inside Creative House
Photo: ©iStock/Inside Creative House Image: ©iStock/Shutthiphong Chandaeng
Image: ©iStock/Shutthiphong Chandaeng Photo: ©iStock/towfiqu ahamed
Photo: ©iStock/towfiqu ahamed Photo: ©iStock/ferrantraite
Photo: ©iStock/ferrantraite Photo: ©iStock/Hiraman
Photo: ©iStock/Hiraman
 Image: ©iStock/Rasi Bhadramani
Image: ©iStock/Rasi Bhadramani Image: ©iStock/LEOcrafts
Image: ©iStock/LEOcrafts Photo: ©iStock/AJ_Watt
Photo: ©iStock/AJ_Watt Photo: ©iStock/Bill Oxford
Photo: ©iStock/Bill Oxford Photo for illustrative purposes only. ©iStock/Highwaystarz-Photography
Photo for illustrative purposes only. ©iStock/Highwaystarz-Photography Photo: ©iStock/Rattankun Thongbun
Photo: ©iStock/Rattankun Thongbun Photo: ©iStock/Shidlovski
Photo: ©iStock/Shidlovski Photo: ©iStock/rogerashford
Photo: ©iStock/rogerashford Photo: ©iStock/mediaphotos
Photo: ©iStock/mediaphotos Photo: ©iStock/AsiaVision
Photo: ©iStock/AsiaVision Photo: ©iStock/RapidEye
Photo: ©iStock/RapidEye  Photo: ©iStock/ExcaliburMedia
Photo: ©iStock/ExcaliburMedia  Photo: ©iStock/monkeybusinessimages
Photo: ©iStock/monkeybusinessimages Photo: ©iStock/fizkes
Photo: ©iStock/fizkes Photo: ©iStock/Liudmila Chernetska
Photo: ©iStock/Liudmila Chernetska Photo: ©iStock/Drazen Zigic
Photo: ©iStock/Drazen Zigic Image: ©iStock/magicmine
Image: ©iStock/magicmine Photo: ©iStock/Antonio_Diaz
Photo: ©iStock/Antonio_Diaz Photo: ©iStock/stevecoleimages
Photo: ©iStock/stevecoleimages Image: ©iStock/libre de droit
Image: ©iStock/libre de droit Image: ©iStock/Dr_Microbe
Image: ©iStock/Dr_Microbe Photo: ©iStock/Solange_Z
Photo: ©iStock/Solange_Z Photo: ©iStock/ChayTee
Photo: ©iStock/ChayTee Photo: ©iStock/gchutka
Photo: ©iStock/gchutka Photo for illustrative purposes only. ©iStock/Drazen Zigic
Photo for illustrative purposes only. ©iStock/Drazen Zigic Photo: ©iStock/monkeybusinessimages
Photo: ©iStock/monkeybusinessimages Photo: ©iStock/amenic181
Photo: ©iStock/amenic181 Image: ©iStock/peterschreiber.media
Image: ©iStock/peterschreiber.media Photo: ©iStock/LaylaBird
Photo: ©iStock/LaylaBird Photo: ©iStock/hobo_018
Photo: ©iStock/hobo_018 Photo: ©iStock/bieshutterb
Photo: ©iStock/bieshutterb Photo: ©iStock/Daria Kulkova
Photo: ©iStock/Daria Kulkova Photo: ©iStock/Hispanolistic
Photo: ©iStock/Hispanolistic Image: ©iStock/natrot
Image: ©iStock/natrot Photo: ©iStock/Vadym Terelyuk
Photo: ©iStock/Vadym Terelyuk Photo: ©iStock/Halfpoint
Photo: ©iStock/Halfpoint Image: ©iStock/Rasi Bhadramani
Image: ©iStock/Rasi Bhadramani Photo: ©iStock/Ridofranz
Photo: ©iStock/Ridofranz Photo: ©iStock
Photo: ©iStock Photo: ©iStock/oatawa
Photo: ©iStock/oatawa Photo: ©iStock/Hailshadow
Photo: ©iStock/Hailshadow Photo: ©iStock/PixelsEffect
Photo: ©iStock/PixelsEffect Image: ©iStock/Dr_Microbe
Image: ©iStock/Dr_Microbe Photo: ©iStock/Christogra4
Photo: ©iStock/Christogra4 Photo: ©iStock/cherrybeans
Photo: ©iStock/cherrybeans Photo: ©iStock/PeopleImages
Photo: ©iStock/PeopleImages Photo: ©iStock/Ridofranz
Photo: ©iStock/Ridofranz Photo: ©iStock/PeopleImages
Photo: ©iStock/PeopleImages Photo: ©iStock/Marco VDM
Photo: ©iStock/Marco VDM Photo: ©iStock/rogerashford
Photo: ©iStock/rogerashford Photo: ©iStock/IURII KRASILNIKOV
Photo: ©iStock/IURII KRASILNIKOV Photo: ©iStock/jaminwell
Photo: ©iStock/jaminwell Photo: ©iStock/AsiaVision
Photo: ©iStock/AsiaVision Photo: ©iStock/Filmstax
Photo: ©iStock/Filmstax Photo: ©iStock/fotostorm
Photo: ©iStock/fotostorm Photo: ©iStock/kitzcorner
Photo: ©iStock/kitzcorner Photo: ©iStock/shapecharge
Photo: ©iStock/shapecharge Photo: ©iStock/Grand Warzawski
Photo: ©iStock/Grand Warzawski Photo: ©iStock/Bet_Noire
Photo: ©iStock/Bet_Noire Photo: ©iStock/DenisTangneyJr
Photo: ©iStock/DenisTangneyJr Photo: ©iStock/Aleksej Sarifulin
Photo: ©iStock/Aleksej Sarifulin Photo: ©iStock/dragana991
Photo: ©iStock/dragana991 Photo: ©iStock/dragana991
Photo: ©iStock/dragana991 Photo: ©iStock/M-Production
Photo: ©iStock/M-Production Photo: ©iStock/zim286
Photo: ©iStock/zim286 Photo: ©iStock/Shidlovski
Photo: ©iStock/Shidlovski Photo: ©Boston VA Medical Center
Photo: ©Boston VA Medical Center Photo: ©Getty Images/ Drazen Zigic
Photo: ©Getty Images/ Drazen Zigic Photo: ©Getty Images/Dani DG
Photo: ©Getty Images/Dani DG Image: ©Getty Images/Shutter2U
Image: ©Getty Images/Shutter2U Image: ©Getty Images/Dr_Microbe
Image: ©Getty Images/Dr_Microbe Photo: ©Getty Images
Photo: ©Getty Images Photo: ©Getty Images/hobo_018
Photo: ©Getty Images/hobo_018 Photo for illustrative purposes only. ©Getty Images/SDI Productions
Photo for illustrative purposes only. ©Getty Images/SDI Productions Image: ©Getty Images/magicmine
Image: ©Getty Images/magicmine Photo: ©Getty Images/FG Trade
Photo: ©Getty Images/FG Trade Photo: ©Getty Images/FatCamera
Photo: ©Getty Images/FatCamera Photo: ©Getty Images/Hispanolistic
Photo: ©Getty Images/Hispanolistic Photo: ©Getty Images/SDI Productions
Photo: ©Getty Images/SDI Productions Photo courtesy of Xenex Disinfection Services.
Photo courtesy of Xenex Disinfection Services. Photo: ©Getty Images/wenht
Photo: ©Getty Images/wenht  Photo: ©Getty Images/SDI Productions
Photo: ©Getty Images/SDI Productions Photo: ©Getty Images/gorodenkoff
Photo: ©Getty Images/gorodenkoff Photo: ©Getty Images/Portra
Photo: ©Getty Images/Portra Photo: ©Frontiers Media SA
Photo: ©Frontiers Media SA Photo: ©Getty Images/LPETTET
Photo: ©Getty Images/LPETTET Photo: ©Getty Images/SeventyFour
Photo: ©Getty Images/SeventyFour Photo: ©Getty Images/Doucefleur
Photo: ©Getty Images/Doucefleur Photo: ©Getty Images/coldsnowstorm
Photo: ©Getty Images/coldsnowstorm Photo: ©Getty Images/FluxFactory
Photo: ©Getty Images/FluxFactory Photo: ©Getty Images/Baranova Valentina
Photo: ©Getty Images/Baranova Valentina Photo: ©Getty Images/eyecare productions
Photo: ©Getty Images/eyecare productions Photo: © Getty Images/Johnrob
Photo: © Getty Images/Johnrob Photo: © Getty Images/Ole_CNX
Photo: © Getty Images/Ole_CNX Photo: © Getty Images/Ozgu Arslan
Photo: © Getty Images/Ozgu Arslan Photo: © Getty Images/magicmine
Photo: © Getty Images/magicmine  Photo: ©Getty Images/rudi_suardi
Photo: ©Getty Images/rudi_suardi Photo: © Getty Images/MTStockStudio
Photo: © Getty Images/MTStockStudio  Photo: ©Getty Images/monkeybusinessimages
Photo: ©Getty Images/monkeybusinessimages Image: ©Getty Images/wildpixel
Image: ©Getty Images/wildpixel Photo: ©Getty Images/simpson33
Photo: ©Getty Images/simpson33 Photo: ©Getty Images/Evgeniy Anikeev
Photo: ©Getty Images/Evgeniy Anikeev Photo: ©Getty Images/HRAUN
Photo: ©Getty Images/HRAUN Image: ©Getty Images/CIPhotos
Image: ©Getty Images/CIPhotos Photo: ©Getty Images/dblight
Photo: ©Getty Images/dblight Photo: ©Getty Images/FG Trade
Photo: ©Getty Images/FG Trade Photo: ©Getty Images/SbytovaMN
Photo: ©Getty Images/SbytovaMN Photo: ©Getty Images/AnnaStills
Photo: ©Getty Images/AnnaStills Photo: ©Getty Images/Halfpoint
Photo: ©Getty Images/Halfpoint Photo: ©Getty Images/YakubovAlim
Photo: ©Getty Images/YakubovAlim Photo: ©Getty Images/digitalskillet
Photo: ©Getty Images/digitalskillet Photo: ©Getty Images/andresr
Photo: ©Getty Images/andresr Photo: ©Getty Images/pcess609
Photo: ©Getty Images/pcess609 Photo: ©Getty Images/Rafmaster
Photo: ©Getty Images/Rafmaster Photo: ©Getty Images/Marco VDM
Photo: ©Getty Images/Marco VDM Image: ©Getty Images/HYWARDS
Image: ©Getty Images/HYWARDS Photo: ©Getty Images/Vladimir Vladimirov
Photo: ©Getty Images/Vladimir Vladimirov Photo: ©Getty Images/peakSTOCK
Photo: ©Getty Images/peakSTOCK Photo: ©Getty Images/cmannphoto
Photo: ©Getty Images/cmannphoto Photo: ©Getty Images/sturti
Photo: ©Getty Images/sturti Photo: ©Getty Images/PaulCalbar
Photo: ©Getty Images/PaulCalbar Photo: ©Getty Images/gradyreese
Photo: ©Getty Images/gradyreese Photo: ©Getty Images/pablohart
Photo: ©Getty Images/pablohart Photo: ©Getty Images/urbazon
Photo: ©Getty Images/urbazon Photo: ©Getty Images/DNY59
Photo: ©Getty Images/DNY59 Photo by Jeff Bowen
Photo by Jeff Bowen Photo: ©Getty Images/Ridofranz
Photo: ©Getty Images/Ridofranz Photo: ©Getty Images/scyther5
Photo: ©Getty Images/scyther5 Photo: ©Getty Images/FatCamera
Photo: ©Getty Images/FatCamera Photo: ©Getty Images/nong2
Photo: ©Getty Images/nong2 Photo: ©Getty Images/Lordn
Photo: ©Getty Images/Lordn Photo: ©Getty Images/puhimec
Photo: ©Getty Images/puhimec Photo: ©Getty Images/FG Trade
Photo: ©Getty Images/FG Trade Photo: ©Getty Images/Visivasnc
Photo: ©Getty Images/Visivasnc Photo: ©Getty Images/Helin Loik-Tomson
Photo: ©Getty Images/Helin Loik-Tomson Photo: ©Getty Images/fizkes
Photo: ©Getty Images/fizkes Photo: ©Getty Images/Igor Vershinsky
Photo: ©Getty Images/Igor Vershinsky Photo: ©Getty Images/AsiaVision
Photo: ©Getty Images/AsiaVision Photo: ©Getty Images/DanielBendjy
Photo: ©Getty Images/DanielBendjy Photo for illustrative purposes only. ©Getty Images/SDI Productions
Photo for illustrative purposes only. ©Getty Images/SDI Productions Photo: ©Getty Images/SanyaSM
Photo: ©Getty Images/SanyaSM Photo: ©Getty Images/FG Trade
Photo: ©Getty Images/FG Trade Photo: ©Getty Images/PeopleImages
Photo: ©Getty Images/PeopleImages Photo: ©Getty Images/Charday Penn
Photo: ©Getty Images/Charday Penn Photo: ©Getty Images/shironosov
Photo: ©Getty Images/shironosov Photo: ©Getty Images/Srdjanns74
Photo: ©Getty Images/Srdjanns74 Image: ©Getty Images/MediaProduction
Image: ©Getty Images/MediaProduction Photo: ©Getty Images/Dean Mitchell
Photo: ©Getty Images/Dean Mitchell Photo: ©Getty Images/SDI Productions
Photo: ©Getty Images/SDI Productions Photo: ©Getty Images/nd3000
Photo: ©Getty Images/nd3000 Photo: ©Getty Images/LaylaBird
Photo: ©Getty Images/LaylaBird Photo: ©Getty Images/Delmaine Donson
Photo: ©Getty Images/Delmaine Donson Photo: ©Getty Images/Isbjorn
Photo: ©Getty Images/Isbjorn Photo: ©Getty Images/zabelin
Photo: ©Getty Images/zabelin Photo: ©Getty Images/Khanchit Khirisutchalual
Photo: ©Getty Images/Khanchit Khirisutchalual Photo: ©Getty Images/tommaso79
Photo: ©Getty Images/tommaso79 Photo: ©Getty Images/Halfpoint
Photo: ©Getty Images/Halfpoint Photo: ©Getty Images/Vladimir Vladimirov
Photo: ©Getty Images/Vladimir Vladimirov Photo: ©Getty Images/smartstock
Photo: ©Getty Images/smartstock Photo: ©Getty Images/Fertnig
Photo: ©Getty Images/Fertnig Photo: ©Getty Images/Renata Angerami
Photo: ©Getty Images/Renata Angerami Photo: ©Getty Images/Barbasa
Photo: ©Getty Images/Barbasa Photo: ©Getty Images/Courtney Hale
Photo: ©Getty Images/Courtney Hale Photo: ©Getty Images/peeterv
Photo: ©Getty Images/peeterv Photo: ©Getty Images/whyframestudios
Photo: ©Getty Images/whyframestudios Image: ©Getty Images/mesut zengin
Image: ©Getty Images/mesut zengin Photo: ©Getty Images/utah778
Photo: ©Getty Images/utah778 Photo: ©Getty Images/portishead1
Photo: ©Getty Images/portishead1 Photo: ©Getty Images/PeopleImages
Photo: ©Getty Images/PeopleImages Photo: ©Getty Images/AlexSava
Photo: ©Getty Images/AlexSava Photo: ©Getty Images/6okean
Photo: ©Getty Images/6okean Photo: ©Getty Images/SDI Productions
Photo: ©Getty Images/SDI Productions Photo: ©Getty Images/Viacheslav Peretiatko
Photo: ©Getty Images/Viacheslav Peretiatko Photo: ©Getty Images/Savushkin
Photo: ©Getty Images/Savushkin Photo: ©Getty Images/fotostorm
Photo: ©Getty Images/fotostorm Photo: ©Getty Images/supersizer
Photo: ©Getty Images/supersizer Photo: ©Getty Images/FatCamera
Photo: ©Getty Images/FatCamera Photo: ©Getty Images/jeremyiswild
Photo: ©Getty Images/jeremyiswild Photo: ©Getty Images/Aleksej Sarifulin
Photo: ©Getty Images/Aleksej Sarifulin Image: ©Getty Images/nopparit
Image: ©Getty Images/nopparit Photo: ©Getty Images/AsiaVision
Photo: ©Getty Images/AsiaVision Photo: ©Getty Images/angkhan
Photo: ©Getty Images/angkhan Photo: ©Getty Images/FG Trade
Photo: ©Getty Images/FG Trade Photo: ©Getty Images/ljubaphoto
Photo: ©Getty Images/ljubaphoto Photo: ©Getty Images/Tero Vesalainen
Photo: ©Getty Images/Tero Vesalainen Photo: ©Getty Images/Cunaplus_M.Faba
Photo: ©Getty Images/Cunaplus_M.Faba Photo: ©Getty Images/megaflopp
Photo: ©Getty Images/megaflopp Image: ©Getty Images/peterschreiber.media
Image: ©Getty Images/peterschreiber.media Photo: ©Getty Images/Suriyawut Suriya
Photo: ©Getty Images/Suriyawut Suriya  Photo: ©Getty Images/kitzcorner
Photo: ©Getty Images/kitzcorner  Photo: ©Getty Images/Yaroslav Olieinikov
Photo: ©Getty Images/Yaroslav Olieinikov Photo: ©Getty Images/Tempura
Photo: ©Getty Images/Tempura Photo: ©Getty Images/ljubaphoto
Photo: ©Getty Images/ljubaphoto Photo: ©Getty Images/sompong_tom
Photo: ©Getty Images/sompong_tom Photo: ©Getty Images/Drazen Zigic
Photo: ©Getty Images/Drazen Zigic Photo: ©Getty Images/Miljan Zivkovic
Photo: ©Getty Images/Miljan Zivkovic Photo: ©Getty Images/Tashatuvango
Photo: ©Getty Images/Tashatuvango Photo: ©Getty Images/Jovanmandic
Photo: ©Getty Images/Jovanmandic Photo: ©Getty Images/Creatas
Photo: ©Getty Images/Creatas Photo: ©Getty Images/Lars Neumann
Photo: ©Getty Images/Lars Neumann Photo: ©Getty Images/andresr
Photo: ©Getty Images/andresr Photo: ©Getty Images/FG Trade
Photo: ©Getty Images/FG Trade Photo: ©Getty Images/DNY59
Photo: ©Getty Images/DNY59 Photo: ©Getty Images/Drazen Zigic
Photo: ©Getty Images/Drazen Zigic  Photo: ©Getty Images/Georgijevic
Photo: ©Getty Images/Georgijevic  Photo: ©Getty Images/PIKSEL
Photo: ©Getty Images/PIKSEL Photo: ©Getty Images/stevecoleimages
Photo: ©Getty Images/stevecoleimages Photo: ©Getty Images/mixetto
Photo: ©Getty Images/mixetto Photo: ©Getty Images/sasacvetkovic33
Photo: ©Getty Images/sasacvetkovic33 Photo: ©Getty Images/shironosov
Photo: ©Getty Images/shironosov Photo: ©Getty Images/angelp
Photo: ©Getty Images/angelp Photo: ©Getty Images/Mladen Zivkovic
Photo: ©Getty Images/Mladen Zivkovic Photo: ©Getty Images/FotoDuets
Photo: ©Getty Images/FotoDuets Photo: ©Getty Images/Kubra Cavus
Photo: ©Getty Images/Kubra Cavus Photo: ©Getty Images/Jay Yuno
Photo: ©Getty Images/Jay Yuno Image: ©Getty Images/EzumeImages
Image: ©Getty Images/EzumeImages Photo: ©Getty Images/cherrybeans
Photo: ©Getty Images/cherrybeans Photo: ©Getty Images/arinarici
Photo: ©Getty Images/arinarici Photo: ©Getty Images/Kanawa_Studio
Photo: ©Getty Images/Kanawa_Studio Photo: ©Getty Images/miodrag ignjatovic
Photo: ©Getty Images/miodrag ignjatovic Photo: ©Getty Images/sanjagrujic
Photo: ©Getty Images/sanjagrujic Photo: ©Getty Images/Manjurul
Photo: ©Getty Images/Manjurul Photo: ©Getty Images/Kayoko Hayashi
Photo: ©Getty Images/Kayoko Hayashi Photo: ©Getty Images/Tero Vesalainen
Photo: ©Getty Images/Tero Vesalainen Photo: ©Getty Images/Drazen Zigic
Photo: ©Getty Images/Drazen Zigic Image: ©Getty Images/image_jungle
Image: ©Getty Images/image_jungle Photo: ©Getty Images/bernardbodo
Photo: ©Getty Images/bernardbodo Photo: ©Getty Images/Drazen Zigic
Photo: ©Getty Images/Drazen Zigic Image: ©Getty Images/Bigpra
Image: ©Getty Images/Bigpra Photo: ©Getty Images/miodrag ignjatovic
Photo: ©Getty Images/miodrag ignjatovic Image: ©Getty Images/Dr_Microbe
Image: ©Getty Images/Dr_Microbe Photo: ©Getty Images/alexi_tm
Photo: ©Getty Images/alexi_tm Photo for illustrative purposes only. ©Getty Images/LittleBee80
Photo for illustrative purposes only. ©Getty Images/LittleBee80 Photo: ©Getty Images/kieferpix
Photo: ©Getty Images/kieferpix Photo: ©Getty Images/Feverpitched
Photo: ©Getty Images/Feverpitched Photo: ©Getty Images/Pornpak Khunatorn
Photo: ©Getty Images/Pornpak Khunatorn Photo for illustrative purposes only. ©Getty Images/zoranm
Photo for illustrative purposes only. ©Getty Images/zoranm Photo: ©Getty Images/stefanamer
Photo: ©Getty Images/stefanamer Photo: ©Getty Images/smartstock
Photo: ©Getty Images/smartstock Image: ©Getty Images/peterschreiber.media
Image: ©Getty Images/peterschreiber.media Photo by Billie Slater
Photo by Billie Slater Photo: ©Getty Images/SDI Productions
Photo: ©Getty Images/SDI Productions Photo: ©Getty Images/guvendemir
Photo: ©Getty Images/guvendemir Photo: ©Getty Images/PeopleImages
Photo: ©Getty Images/PeopleImages Photo: ©Getty Images/FG Trade
Photo: ©Getty Images/FG Trade Photo: ©Getty Images/BackyardProduction
Photo: ©Getty Images/BackyardProduction Photo: ©Getty Images/Lucky7trader
Photo: ©Getty Images/Lucky7trader Photo: ©Getty Images/FatCamera
Photo: ©Getty Images/FatCamera Photo: ©Getty Images/towfiqu ahamed
Photo: ©Getty Images/towfiqu ahamed Photo: ©Getty Images/Motortion
Photo: ©Getty Images/Motortion Photo: ©Getty Images/digitalskillet
Photo: ©Getty Images/digitalskillet Photo: ©Getty Images/Courtney Hale
Photo: ©Getty Images/Courtney Hale Photo: ©Getty Images/Punnarong
Photo: ©Getty Images/Punnarong Photo: ©Getty Images/grandriver
Photo: ©Getty Images/grandriver Photo: ©Getty Images/Zaharia_Bogdan
Photo: ©Getty Images/Zaharia_Bogdan Photo: ©Getty Images/Srdjanns74
Photo: ©Getty Images/Srdjanns74 Photo: ©Getty Images/South_agency
Photo: ©Getty Images/South_agency Photo: ©Getty Images/LifestyleVisuals
Photo: ©Getty Images/LifestyleVisuals Photo: ©Getty Images/Inside Creative House
Photo: ©Getty Images/Inside Creative House Photo: ©Getty Images/JurgaR
Photo: ©Getty Images/JurgaR Photo: ©Getty Images/PeopleImages
Photo: ©Getty Images/PeopleImages Photo for illustrative purposes only. ©Getty Images/AleksandarGeorgiev
Photo for illustrative purposes only. ©Getty Images/AleksandarGeorgiev Photo: ©Getty Images/luismmolina
Photo: ©Getty Images/luismmolina Image: ©Getty Images/Design Cells
Image: ©Getty Images/Design Cells Photo: ©Getty Images/morrowlight
Photo: ©Getty Images/morrowlight Photo courtesy of HERL
Photo courtesy of HERL Photo: ©Getty Images/bymuratdeniz
Photo: ©Getty Images/bymuratdeniz Photo: ©Getty Images/ZzzVuk
Photo: ©Getty Images/ZzzVuk Photo: ©Getty Images/Courtney Hale
Photo: ©Getty Images/Courtney Hale Photo: ©Getty Images/SeventyFour
Photo: ©Getty Images/SeventyFour Photo: ©Getty Images/solarseven
Photo: ©Getty Images/solarseven Photo: ©Getty Images/Image Source
Photo: ©Getty Images/Image Source Image: ©Getty Images/BlackJack3D
Image: ©Getty Images/BlackJack3D Image: ©Getty Images/Gio_tto
Image: ©Getty Images/Gio_tto Photo: ©Getty Images/ljubaphoto
Photo: ©Getty Images/ljubaphoto Photo: ©Getty Images/insta_photos
Photo: ©Getty Images/insta_photos Photo: ©Getty Images/zabelin
Photo: ©Getty Images/zabelin Photo: ©Getty Images/Malikov Aleksandr
Photo: ©Getty Images/Malikov Aleksandr Image: ©Getty Images/Gilnature
Image: ©Getty Images/Gilnature Photo: ©Getty Images/evgenyb
Photo: ©Getty Images/evgenyb Photo: ©Getty Images/rogerashford
Photo: ©Getty Images/rogerashford Photo for illustrative purposes only. ©Getty Images/SDI Productions
Photo for illustrative purposes only. ©Getty Images/SDI Productions Photo for illustrative purposes only. ©Getty Images/SeventyFour
Photo for illustrative purposes only. ©Getty Images/SeventyFour Photo: ©Getty Images/Morsa Images
Photo: ©Getty Images/Morsa Images Photo: ©Getty Images/GeniusKp
Photo: ©Getty Images/GeniusKp Photo: ©Getty Images/sturti
Photo: ©Getty Images/sturti Photo: ©Getty Images/PeopleImages
Photo: ©Getty Images/PeopleImages Photo for illustrative purposes only. ©Getty Images/Nes
Photo for illustrative purposes only. ©Getty Images/Nes Photo: ©Getty Images/Geber86
Photo: ©Getty Images/Geber86 Photo: ©Getty Images/PeopleImages
Photo: ©Getty Images/PeopleImages Photo: ©Getty Images/Andranik Hakobyan
Photo: ©Getty Images/Andranik Hakobyan Photo for illustrative purposes only. ©Getty Images/FG Trade
Photo for illustrative purposes only. ©Getty Images/FG Trade Photo: ©Getty Images/yanyong
Photo: ©Getty Images/yanyong Image: ©Getty Images/magicmine
Image: ©Getty Images/magicmine Photo: ©Getty Images/Ridofranz
Photo: ©Getty Images/Ridofranz Photo: ©Getty Images/mustafagull
Photo: ©Getty Images/mustafagull Photo: ©Getty Images/Chris Marshall
Photo: ©Getty Images/Chris Marshall Photo: ©Getty Images/Marje
Photo: ©Getty Images/Marje Photo: ©Getty Images/PeopleImages
Photo: ©Getty Images/PeopleImages Photo: ©Getty Images/dra_schwartz
Photo: ©Getty Images/dra_schwartz Photo: ©Getty Images/LordHenriVoton
Photo: ©Getty Images/LordHenriVoton Image: ©Getty Images/dzika_mrowka
Image: ©Getty Images/dzika_mrowka Photo: ©Getty Images/Inside Creative House
Photo: ©Getty Images/Inside Creative House Photo: ©Getty Images/danchooalex
Photo: ©Getty Images/danchooalex Photo: ©Getty Images/SDI Productions
Photo: ©Getty Images/SDI Productions Image: ©Getty Images/selvanegra
Image: ©Getty Images/selvanegra Photo: ©Getty Images/AsiaVision
Photo: ©Getty Images/AsiaVision Image: ©Getty Images/image_jungle
Image: ©Getty Images/image_jungle Photo: ©Getty Images/BeholdingEye
Photo: ©Getty Images/BeholdingEye  Photo for illustrative purposes only. ©Getty Images/Ridofranz
Photo for illustrative purposes only. ©Getty Images/Ridofranz  Photo: ©Getty Images/vitapix
Photo: ©Getty Images/vitapix  Image: ©Getty Images/kirstypargeter
Image: ©Getty Images/kirstypargeter Photo: ©Getty Images/rogerashford
Photo: ©Getty Images/rogerashford Photo: ©Getty Images/Andrei Sauko
Photo: ©Getty Images/Andrei Sauko Photo: ©Getty Images/globalmoments
Photo: ©Getty Images/globalmoments Photo: ©Getty Images/South_agency
Photo: ©Getty Images/South_agency Photo: ©Getty Images/Mukhina1
Photo: ©Getty Images/Mukhina1 Photo: ©Getty Images/spukkato
Photo: ©Getty Images/spukkato Photo: ©Getty Images/PeopleImages
Photo: ©Getty Images/PeopleImages Photo: ©Getty Images/gorodenkoff
Photo: ©Getty Images/gorodenkoff Photo: ©Getty Images/Kativ
Photo: ©Getty Images/Kativ Photo: ©Getty Images/Photodisc
Photo: ©Getty Images/Photodisc Photo: ©Getty Images/FatCamera
Photo: ©Getty Images/FatCamera Photo: ©Getty Images/ablokhin
Photo: ©Getty Images/ablokhin Image: ©Getty Images/wir0man
Image: ©Getty Images/wir0man Photo: ©Getty Images/AntonioGuillem
Photo: ©Getty Images/AntonioGuillem Photo: ©Getty Images/Marat Musabirov
Photo: ©Getty Images/Marat Musabirov Photo: ©Getty Images/Aaron Hawkins
Photo: ©Getty Images/Aaron Hawkins Photo: ©Getty Images/koya79
Photo: ©Getty Images/koya79 Photo: ©iStock/Cortney Hale
Photo: ©iStock/Cortney Hale ©iStock/Wavebreakmedia Photo for illustrative purposes only.
©iStock/Wavebreakmedia Photo for illustrative purposes only.  Image: ©iStock/Evgeny Gromov
Image: ©iStock/Evgeny Gromov Photo: ©iStock/PeopleImages
Photo: ©iStock/PeopleImages Photo: ©iStock/Dusan Ilic
Photo: ©iStock/Dusan Ilic Photo: ©iStock/yulka3ice
Photo: ©iStock/yulka3ice Photo: ©iStock/Prostock-Studio
Photo: ©iStock/Prostock-Studio Image: ©iStock/Floriana
Image: ©iStock/Floriana Photo: ©iStock/Brasil2
Photo: ©iStock/Brasil2 Photo: ©iStock/Piyapong Thongcharoen
Photo: ©iStock/Piyapong Thongcharoen Photo: ©iStock/robertcicchetti
Photo: ©iStock/robertcicchetti ©iStock/molchanovdmitry
©iStock/molchanovdmitry Photo: ©iStock/ljubaphoto
Photo: ©iStock/ljubaphoto Photo: ©iStock/koto_feja
Photo: ©iStock/koto_feja Photo: ©iStock/kckate16
Photo: ©iStock/kckate16 Photo: ©iStock/Ridofranz
Photo: ©iStock/Ridofranz Photo: ©iStock/PeopleImages
Photo: ©iStock/PeopleImages Photo: ©iStock/MattGush
Photo: ©iStock/MattGush Photo: ©iStock/Giuseppe Lombardo
Photo: ©iStock/Giuseppe Lombardo Photo: ©iStock/Hispanolistic
Photo: ©iStock/Hispanolistic Photo: ©iStock/Daisy-Daisy
Photo: ©iStock/Daisy-Daisy Photo: ©iStock/Nattakorn Maneerat
Photo: ©iStock/Nattakorn Maneerat Photo: ©iStock/Jose Girarte
Photo: ©iStock/Jose Girarte Photo: ©iStock/humonia
Photo: ©iStock/humonia Photo: ©iStock/pixdeluxe
Photo: ©iStock/pixdeluxe Photo: ©iStock/Bim
Photo: ©iStock/Bim Photo: ©iStock/jarun011
Photo: ©iStock/jarun011 Photo: ©iStock/sasirin pamai
Photo: ©iStock/sasirin pamai Photo: ©iStock/ligonpix
Photo: ©iStock/ligonpix Photo: ©iStock/baona
Photo: ©iStock/baona Photo for illustrative purposes only. ©iStock/Courtney Hale
Photo for illustrative purposes only. ©iStock/Courtney Hale Photo: ©iStock/KatarzynaBialasiewicz
Photo: ©iStock/KatarzynaBialasiewicz Photo: ©iStock/NoDerog
Photo: ©iStock/NoDerog Photo: ©iStock/fizkes
Photo: ©iStock/fizkes Photo: ©iStock/ljubaphoto
Photo: ©iStock/ljubaphoto Photo: ©iStock/gsheldon
Photo: ©iStock/gsheldon Photo for illustrative purposes only. ©iStock/ajr_images
Photo for illustrative purposes only. ©iStock/ajr_images Photo: ©iStock/vitapix
Photo: ©iStock/vitapix Photo: ©iStock/FatCamera
Photo: ©iStock/FatCamera Photo: ©iStock/Juanmonino
Photo: ©iStock/Juanmonino Photo: ©iStock/Srdjanns74
Photo: ©iStock/Srdjanns74 Photo: ©iStock/hudiemm
Photo: ©iStock/hudiemm Image: ©iStock/wildpixel
Image: ©iStock/wildpixel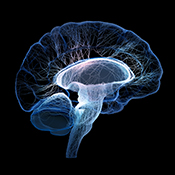 Image: ©iStock/johan63
Image: ©iStock/johan63 Photo: ©iStock/JamesBrey
Photo: ©iStock/JamesBrey Image: ©iStock/Naeblys
Image: ©iStock/Naeblys Photo: ©iStock/Enes Evren
Photo: ©iStock/Enes Evren Photo: ©iStock/Ivan-balvan
Photo: ©iStock/Ivan-balvan Photo: ©iStock/Henrik5000
Photo: ©iStock/Henrik5000 Photo: ©iStock/Evgenyi_Eg
Photo: ©iStock/Evgenyi_Eg Photo: ©iStock/Olga Novikova
Photo: ©iStock/Olga Novikova Photo: ©iStock/PeopleImages
Photo: ©iStock/PeopleImages Image: ©iStock/peterschreiber.media
Image: ©iStock/peterschreiber.media Photo: ©iStock/Kichigin
Photo: ©iStock/Kichigin Photo: ©iStock/MilosStankovic
Photo: ©iStock/MilosStankovic Photo: ©iStock/digicomphoto
Photo: ©iStock/digicomphoto Photo: ©iStock/ligonpix
Photo: ©iStock/ligonpix Photo: ©iStock/Dean Mitchell
Photo: ©iStock/Dean Mitchell Photo: ©iStock/grandriver
Photo: ©iStock/grandriver Photo: ©iStock/KarenMower
Photo: ©iStock/KarenMower Photo: ©iStock/wildpixel
Photo: ©iStock/wildpixel Photo: ©iStock/ananaline
Photo: ©iStock/ananaline Image: ©iStock/luismmolina
Image: ©iStock/luismmolina Photo: ©iStock/Georgijevic
Photo: ©iStock/Georgijevic Photo for illustrative purposes only. ©iStock/monkeybusinessimages
Photo for illustrative purposes only. ©iStock/monkeybusinessimages Photo: ©iStock/nensuria
Photo: ©iStock/nensuria Image: ©iStock/wildpixel
Image: ©iStock/wildpixel Photo: ©iStock/SDI Productions
Photo: ©iStock/SDI Productions Photo: ©iStock/Hailshadow
Photo: ©iStock/Hailshadow Photo: ©iStock/CasarsaGuru
Photo: ©iStock/CasarsaGuru Photo: ©iStock/izusek
Photo: ©iStock/izusek Photo: ©iStock/Drazen Zigic
Photo: ©iStock/Drazen Zigic Photo: ©iStock/mustafagull
Photo: ©iStock/mustafagull Photo: ©iStock/insta_photos
Photo: ©iStock/insta_photos Photo: ©iStock/amenic181
Photo: ©iStock/amenic181 Photo: ©iStock/utah778
Photo: ©iStock/utah778 Photo: ©iStock/RealPeopleGroup
Photo: ©iStock/RealPeopleGroup Photo: ©iStock/xavierarnau
Photo: ©iStock/xavierarnau Image: ©iStock/peterschreiber.media
Image: ©iStock/peterschreiber.media Photo: ©iStock/Sezeryadigar
Photo: ©iStock/Sezeryadigar Photo: ©iStock/AlxeyPnferov
Photo: ©iStock/AlxeyPnferov Photo: ©iStock/katleho Seisa
Photo: ©iStock/katleho Seisa Photo: ©iStock/kovop58
Photo: ©iStock/kovop58 Photo: ©iStock/Marjan_Apostolovic
Photo: ©iStock/Marjan_Apostolovic Photo: ©iStock/turk_stock_photographer
Photo: ©iStock/turk_stock_photographer Photo: ©iStock/Rockfinder
Photo: ©iStock/Rockfinder Photo: ©iStock/Aleksej Sarifulin
Photo: ©iStock/Aleksej Sarifulin Image: ©iStock/wildpixel
Image: ©iStock/wildpixel Photo: ©iStock/shapecharge
Photo: ©iStock/shapecharge Photo: ©iStock/Antic Zlatko
Photo: ©iStock/Antic Zlatko Image: ©iStock/4X-image
Image: ©iStock/4X-image Photo: ©iStock/AaronAmat
Photo: ©iStock/AaronAmat Photo: ©iStock/ljubaphoto
Photo: ©iStock/ljubaphoto Photo: ©iStock/thebigland88
Photo: ©iStock/thebigland88 Photo: ©iStock/shunyufan
Photo: ©iStock/shunyufan Photo: ©iStock/grandriver
Photo: ©iStock/grandriver Photo: ©iStock/LordHenriVoton
Photo: ©iStock/LordHenriVoton Photo: ©iStock/Satyrenko
Photo: ©iStock/Satyrenko Photo: ©iStock/Hailshadow
Photo: ©iStock/Hailshadow Photo: ©iStock/MachineHeadz
Photo: ©iStock/MachineHeadz Photo: ©iStock/annebaek
Photo: ©iStock/annebaek Illustration: ©iStock/sankalpmaya
Illustration: ©iStock/sankalpmaya Photo: ©iStock/Srdjanns74
Photo: ©iStock/Srdjanns74 Photo: ©iStock/1281086710.jpg
Photo: ©iStock/1281086710.jpg Photo: ©iStock/AleksandarGeorgiev
Photo: ©iStock/AleksandarGeorgiev Photo: ©iStock/Atiwat Studio
Photo: ©iStock/Atiwat Studio Photo: ©iStock/FG Trade
Photo: ©iStock/FG Trade Photo: ©iStock/TefiM
Photo: ©iStock/TefiM Photo: ©iStock/Juanmonino
Photo: ©iStock/Juanmonino Photo: ©iStock/JONGHO SHIN
Photo: ©iStock/JONGHO SHIN Photo: ©iStock/Nenad Cavoski
Photo: ©iStock/Nenad Cavoski Photo: ©iStock/yenwen
Photo: ©iStock/yenwen Photo: ©iStock/JONGHO SHIN
Photo: ©iStock/JONGHO SHIN Photo: ©iStock/anyaivanova
Photo: ©iStock/anyaivanova Photo: ©iStock/kali9
Photo: ©iStock/kali9 Photo: ©iStock/1147468451
Photo: ©iStock/1147468451 Photo: ©iStock/monkeybusinessimages
Photo: ©iStock/monkeybusinessimages Photo: ©iStock/LightFieldStudios
Photo: ©iStock/LightFieldStudios Photo: ©iStock/Chinnapong
Photo: ©iStock/Chinnapong Photo: ©iStock/SDI Productions
Photo: ©iStock/SDI Productions Photo: ©iStock/PeopleImages
Photo: ©iStock/PeopleImages Photo: ©iStock/peterschreiber.media
Photo: ©iStock/peterschreiber.media Photo: ©iStock/Charles Wollertz
Photo: ©iStock/Charles Wollertz Photo: ©iStock/katleho Seisa
Photo: ©iStock/katleho Seisa Photo: ©iStock/Gio_tto
Photo: ©iStock/Gio_tto Photo: ©iStock/digihelion
Photo: ©iStock/digihelion Photo: ©iStock/homeworks255
Photo: ©iStock/homeworks255 Photo: ©iStock/bagi1998
Photo: ©iStock/bagi1998 Photo: ©iStock/fotografixx
Photo: ©iStock/fotografixx Photo for illustrative purposes only. ©iStock/Geber86
Photo for illustrative purposes only. ©iStock/Geber86 Veterans Health Administration photo
Veterans Health Administration photo Photo: ©iStock/blueringmedia
Photo: ©iStock/blueringmedia Photo for illustrative purposes only. ©iStock/Juanmonino
Photo for illustrative purposes only. ©iStock/Juanmonino Photo: ©iStock/vadimguzhva
Photo: ©iStock/vadimguzhva Photo for illustrative purposes only. ©iStock/digitalskillet
Photo for illustrative purposes only. ©iStock/digitalskillet Photo for illustrative purposes only. ©iStock/jacoblund
Photo for illustrative purposes only. ©iStock/jacoblund Illustration: ©iStock/Nerthuz
Illustration: ©iStock/Nerthuz Photo: ©iStock/lapandr
Photo: ©iStock/lapandr Photo for illustrative purposes only. ©iStock
Photo for illustrative purposes only. ©iStock Photo: ©iStock/Morsa Images
Photo: ©iStock/Morsa Images U.S. Army photo by Maj. Thomas Cieslak
U.S. Army photo by Maj. Thomas Cieslak Photo: ©iStock/davidperks
Photo: ©iStock/davidperks Photo by Robert Turtil
Photo by Robert Turtil Photo: ©iStock/jamesbenet
Photo: ©iStock/jamesbenet Photo: ©iStock/laflor
Photo: ©iStock/laflor Photo: ©iStock/selvanegra
Photo: ©iStock/selvanegra Photo: ©iStock/VladimirSorokin
Photo: ©iStock/VladimirSorokin DOD photo by Lance Cpl. Immanuel Johnson
DOD photo by Lance Cpl. Immanuel Johnson Photo: ©iStock/beerkoff
Photo: ©iStock/beerkoff  Photo for illustrative purposes only. ©iStock/BraunS
Photo for illustrative purposes only. ©iStock/BraunS Photo: ©iStock/homeworks255
Photo: ©iStock/homeworks255 Photo: ©iStock/SDI Productions
Photo: ©iStock/SDI Productions Photo: ©iStock/erdikocak
Photo: ©iStock/erdikocak
 Photo: ©iStock/Rostislav_Sedlacek
Photo: ©iStock/Rostislav_Sedlacek Photo: ©iStock/vadimguzhva
Photo: ©iStock/vadimguzhva Photo: ©iStock/vitapix
Photo: ©iStock/vitapix Photo: ©iStock/duncan1890
Photo: ©iStock/duncan1890 Photo: ©iStock/licsiren
Photo: ©iStock/licsiren Photo: ©iStock/SDI Productions
Photo: ©iStock/SDI Productions Photo: ©iStock/NickyLloyd
Photo: ©iStock/NickyLloyd Photo: ©iStock/stevanovicigor
Photo: ©iStock/stevanovicigor Photo: ©iStock/Rawf8
Photo: ©iStock/Rawf8 Photo: ©iStock/monkeybusinessimages
Photo: ©iStock/monkeybusinessimages Photo: ©iStock/jxfzsy
Photo: ©iStock/jxfzsy Photo: ©iStock/yodiyim
Photo: ©iStock/yodiyim Photo: ©iStock/fotografixx
Photo: ©iStock/fotografixx Photo: ©iStock/eclipse_images
Photo: ©iStock/eclipse_images Photo: ©iStock/MJFelt
Photo: ©iStock/MJFelt Photo: ©iStock/kieferpix
Photo: ©iStock/kieferpix Photo: ©iStock/Zinkevych
Photo: ©iStock/Zinkevych Photo: ©iStock/jxfzsy
Photo: ©iStock/jxfzsy Photo: ©iStock/mr.suphachai praserdumrongchai
Photo: ©iStock/mr.suphachai praserdumrongchai Photo by April Eilers
Photo by April Eilers Photo: ©iStock/yelo34
Photo: ©iStock/yelo34 Photo: ©Peter Horrox
Photo: ©Peter Horrox Photo: ©iStock/PeopleImages
Photo: ©iStock/PeopleImages Photo: ©iStock/FG Trade
Photo: ©iStock/FG Trade Photo: ©iStock/rogerashford
Photo: ©iStock/rogerashford Photo: ©iStock/JohnnyGreig
Photo: ©iStock/JohnnyGreig Photo: ©iStock/Mikhail Artamonov
Photo: ©iStock/Mikhail Artamonov Photo: ©iStock/PIKSEL
Photo: ©iStock/PIKSEL Photo: ©iStock/Aleksandr_Gromov
Photo: ©iStock/Aleksandr_Gromov Photo: ©iStock/Mary Swift
Photo: ©iStock/Mary Swift Photo for illustrative purposes only. ©iStock/amenic181
Photo for illustrative purposes only. ©iStock/amenic181 Photo: ©iStock/Chinnapong
Photo: ©iStock/Chinnapong Photo: ©iStock/kieferpix
Photo: ©iStock/kieferpix Photo for illustrative purposes only. ©iStock/FatCamera
Photo for illustrative purposes only. ©iStock/FatCamera Photo: ©iStock/Rattankun Thongbun
Photo: ©iStock/Rattankun Thongbun Photo: ©iStock/fizkes
Photo: ©iStock/fizkes Photo: ©iStock/Hailshadow
Photo: ©iStock/Hailshadow Photo: ©iStock/LumiNola
Photo: ©iStock/LumiNola Photo for illustrative purposes only. ©iStock/adamkaz
Photo for illustrative purposes only. ©iStock/adamkaz Photo: ©iStock/yodiyim
Photo: ©iStock/yodiyim Photo: iStock/JohnnyGreig
Photo: iStock/JohnnyGreig Photo: iStock/SDI Productions
Photo: iStock/SDI Productions Photo: iStock/peakSTOCK
Photo: iStock/peakSTOCK Photo: iStock/KenTannenbaum
Photo: iStock/KenTannenbaum Photo: iStock/axelbueckert
Photo: iStock/axelbueckert Photo: iStock/g-stockstudio
Photo: iStock/g-stockstudio Photo: iStock/adventtr
Photo: iStock/adventtr Photo: iStock/SDI Productions
Photo: iStock/SDI Productions Photo: iStock/monkeybusinessimages
Photo: iStock/monkeybusinessimages Photo: iStock/MangTeng
Photo: iStock/MangTeng Photo: iStock/Rasi Bhadramani
Photo: iStock/Rasi Bhadramani Photo: iStock/SDI Productions
Photo: iStock/SDI Productions Photo for illustrative purposes only. ©iStock/patrickheagney
Photo for illustrative purposes only. ©iStock/patrickheagney Photo: ©iStock/Hailshadow
Photo: ©iStock/Hailshadow Photo: ©iStock/alvarez
Photo: ©iStock/alvarez Photo for illustrative purposes only. ©iStock/Marjan_Apostolovic
Photo for illustrative purposes only. ©iStock/Marjan_Apostolovic Photo: ©iStock/vadimguzhva
Photo: ©iStock/vadimguzhva Photo for illustrative purposes only. ©iStock/PeopleImages
Photo for illustrative purposes only. ©iStock/PeopleImages Photo for illustrative purposes only. ©iStock/GlobalStock
Photo for illustrative purposes only. ©iStock/GlobalStock Photo: ©iStock/PeopleImages
Photo: ©iStock/PeopleImages Photo: ©iStock/dra_schwartz
Photo: ©iStock/dra_schwartz Photo for illustrative purposes only. ©iStock/DjelicS
Photo for illustrative purposes only. ©iStock/DjelicS Photo for illustrative purposes only. ©iStock/Human Role
Photo for illustrative purposes only. ©iStock/Human Role Photo: ©iStock/South_agency
Photo: ©iStock/South_agency Photo for illustrative purposes only. ©iStock/DragonImages
Photo for illustrative purposes only. ©iStock/DragonImages Photo: ©iStock/Dennis Torkhov
Photo: ©iStock/Dennis Torkhov Photo for illustrative purposes only. ©iStock/nimis69
Photo for illustrative purposes only. ©iStock/nimis69 (U.S. Army Reserve photo by Master Sgt. Michel Sauret,for illustrative purposes only.)
(U.S. Army Reserve photo by Master Sgt. Michel Sauret,for illustrative purposes only.) Photo: ©iStock/pixelci
Photo: ©iStock/pixelci Photo for illustrative purposes only. ©iStock/Yuri_Arcurs
Photo for illustrative purposes only. ©iStock/Yuri_Arcurs Photos for illustrative purposes only. ©iStock/ Petko Ninov; DigitalSkillset
Photos for illustrative purposes only. ©iStock/ Petko Ninov; DigitalSkillset Photo: ©iStock/leezsnow
Photo: ©iStock/leezsnow Photo: ©iStock/nicolas
Photo: ©iStock/nicolas Photo: ©iStock/kali9
Photo: ©iStock/kali9 Photo for illustrative purposes only. ©iStock/JohnnyGreig
Photo for illustrative purposes only. ©iStock/JohnnyGreig Photo for illustrative purposes only. ©iStock/FatCamera
Photo for illustrative purposes only. ©iStock/FatCamera Photo: ©/Charles Wollertz
Photo: ©/Charles Wollertz Photo by Jerry Daliege
Photo by Jerry Daliege Photo: ©iStock/kevinruss
Photo: ©iStock/kevinruss Photo for illustrative purposes only. ©iStock/fizkes
Photo for illustrative purposes only. ©iStock/fizkes Photo: ©iStock/FG Trade
Photo: ©iStock/FG Trade Photo for illustrative purposes only. ©iStock/FlairImages
Photo for illustrative purposes only. ©iStock/FlairImages Photo for illustrative purposes only. ©iStock/adamkaz
Photo for illustrative purposes only. ©iStock/adamkaz Photo for illustrative purposes only. ©iStock/sturti
Photo for illustrative purposes only. ©iStock/sturti Photo: ©iStock/contrastaddict
Photo: ©iStock/contrastaddict Photo for illustrative purposes only. ©iStock/milanvirijevic
Photo for illustrative purposes only. ©iStock/milanvirijevic Photo: ©iStock/izusek
Photo: ©iStock/izusek Photo: ©iStock/Design Cells
Photo: ©iStock/Design Cells Photo by Mitch Mirkin
Photo by Mitch Mirkin Photo for illustrative purposes only. ©iStock/monkeybusinessimages
Photo for illustrative purposes only. ©iStock/monkeybusinessimages Photo: ©iStock/Nicolas
Photo: ©iStock/Nicolas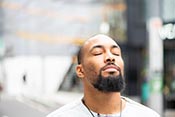 Photo for illustrative purposes only. ©iStock/electravk
Photo for illustrative purposes only. ©iStock/electravk Photo by Senior Airman Julianne Showalter, USAF
Photo by Senior Airman Julianne Showalter, USAF Photo for illustrative purposes only. ©iStock/seb_ra
Photo for illustrative purposes only. ©iStock/seb_ra Photo for illustrative purposes only. ©iStock/fizkes
Photo for illustrative purposes only. ©iStock/fizkes Photo: ©iStock/koto_feja
Photo: ©iStock/koto_feja  Photo for illustrative purposes only. ©iStock/ClarkandCompany
Photo for illustrative purposes only. ©iStock/ClarkandCompany Photo: ©iStock/chesiireCat
Photo: ©iStock/chesiireCat Photo for illustrative purposes only. ©iStock/Viktoriia Hnatiuk
Photo for illustrative purposes only. ©iStock/Viktoriia Hnatiuk Photo for illustrative purposes only. ©iStock/Image Source
Photo for illustrative purposes only. ©iStock/Image Source Photo by Jerry Daliege
Photo by Jerry Daliege Photo for illustrative purposes only. ©iStock/Darunechka
Photo for illustrative purposes only. ©iStock/Darunechka Photo: ©iStock/Pornpak Khunatorn
Photo: ©iStock/Pornpak Khunatorn Photo: ©iStock/cdascher
Photo: ©iStock/cdascher Photo for illustrative purposes only. ©iStock/Burlingham
Photo for illustrative purposes only. ©iStock/Burlingham Photo: ©iStock/Maya23K
Photo: ©iStock/Maya23K Photo: ©iStock/ftwitty
Photo: ©iStock/ftwitty Photo: ©iStock/microgen
Photo: ©iStock/microgen Photo for illustrative purposes only. ©iStock/SDI Productions
Photo for illustrative purposes only. ©iStock/SDI Productions Photo: ©iStock/danchooalex
Photo: ©iStock/danchooalex Photo for illustrative purposes only. ©iStock/electravk
Photo for illustrative purposes only. ©iStock/electravk Illustration: ©iStock/Victor_Brave
Illustration: ©iStock/Victor_Brave Illustration: ©iStock/poba
Illustration: ©iStock/poba Photo: ©iStock/Eduard Lysenko
Photo: ©iStock/Eduard Lysenko Photo for illustrative purposes only. ©iStock/tommaso79
Photo for illustrative purposes only. ©iStock/tommaso79 Photo: ©iStock/Gligatron
Photo: ©iStock/Gligatron Photo: ©iStock/mescioglu
Photo: ©iStock/mescioglu Illustration: ©iStock/Lars Neumann
Illustration: ©iStock/Lars Neumann Photo: ©iStock/sanjagrujic
Photo: ©iStock/sanjagrujic Photo for illustrative purposes only. ©iStock/Kali9
Photo for illustrative purposes only. ©iStock/Kali9 Photo: ©iStock/ZzzVuk
Photo: ©iStock/ZzzVuk Photo by Spc. Anthony Zendejas/USA
Photo by Spc. Anthony Zendejas/USA U.S. Army photo by Maj. Thomas Cieslak
U.S. Army photo by Maj. Thomas Cieslak Photo: ©iStock/shironosov
Photo: ©iStock/shironosov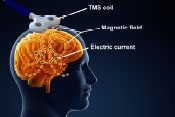
 Photo: ©iStock/ljubaphoto
Photo: ©iStock/ljubaphoto Photo: ©iStock/D-Keine
Photo: ©iStock/D-Keine Photo for illustrative purposes only. Courtesy of Cincinnati VAMC
Photo for illustrative purposes only. Courtesy of Cincinnati VAMC Photo: ©iStock/Denes Farkas
Photo: ©iStock/Denes Farkas Photo for illustrative purposes only. ©iStock/RgStudio
Photo for illustrative purposes only. ©iStock/RgStudio Photo by CPT George Clemmons/USAF
Photo by CPT George Clemmons/USAF (Photo illustration by Michael Escalante)
(Photo illustration by Michael Escalante) Photo for illustrative purposes only. ©iStock/BakiBG
Photo for illustrative purposes only. ©iStock/BakiBG Photo: ©iStock/South_agency
Photo: ©iStock/South_agency Photo: ©iStock/fizkes
Photo: ©iStock/fizkes Photo: ©iStock/uchar
Photo: ©iStock/uchar Photo by Lance Cpl. Immanuel Johnson/USMC
Photo by Lance Cpl. Immanuel Johnson/USMC Photo: ©iStock/jarun011
Photo: ©iStock/jarun011 Photo: ©iStock/KatarzynaBialasiewicz
Photo: ©iStock/KatarzynaBialasiewicz Photo: ©iStock/MartinPrescott
Photo: ©iStock/MartinPrescott Photo: ©iStock/JoKMedia
Photo: ©iStock/JoKMedia U.S. Army photo by Spc. Jeffery
U.S. Army photo by Spc. Jeffery Photo: ©iStock/Suriyawut Suriya
Photo: ©iStock/Suriyawut Suriya Photo: ©iStock/Alexey_ds
Photo: ©iStock/Alexey_ds Photo: ©iStock/sestovic
Photo: ©iStock/sestovic Photo: ©iStock/Creative-Family
Photo: ©iStock/Creative-Family Photo for illustrative purposes only. ©iStock/stockstudioX
Photo for illustrative purposes only. ©iStock/stockstudioX Photo: ©iStock/asiandelight
Photo: ©iStock/asiandelight Photo for illustrative purposes only. ©iStock/asiseeit
Photo for illustrative purposes only. ©iStock/asiseeit iStock/South_agency
iStock/South_agency Photo for illustrative purposes only. By Ensign Haraz Ghanbari/USN
Photo for illustrative purposes only. By Ensign Haraz Ghanbari/USN  Photo for illustrative purposes only. ©iStock/Juanmonino
Photo for illustrative purposes only. ©iStock/Juanmonino Photo for illustrative purposes only. ©iStock/joloei
Photo for illustrative purposes only. ©iStock/joloei
 DoD photo by Lance Cpl. Immanuel Johnson
DoD photo by Lance Cpl. Immanuel Johnson Photo: ©iStock/Darwin Brandis
Photo: ©iStock/Darwin Brandis Photo: ©iStock/sd619
Photo: ©iStock/sd619 Illustration: ©iStock/Lamenko
Illustration: ©iStock/Lamenko Photo: ©iStock/mphillips007
Photo: ©iStock/mphillips007 Photo: ©iStock/AndreyPopov
Photo: ©iStock/AndreyPopov Photo: ©iStock/Ridofranz
Photo: ©iStock/Ridofranz Photo: ©iStock/okskaz
Photo: ©iStock/okskaz Photo for illustrative purposes only. ©iStock/Capifrutta
Photo for illustrative purposes only. ©iStock/Capifrutta Photo: ©iStock/Wavebreakmedia
Photo: ©iStock/Wavebreakmedia Photo for illustrative purposes only. ©iStock/SeventyFour
Photo for illustrative purposes only. ©iStock/SeventyFour Photo: ©iStock/Hailshadow
Photo: ©iStock/Hailshadow Photo: ©iStock/MartinPrescott
Photo: ©iStock/MartinPrescott Photo: ©iStock/Vera_Petrunina
Photo: ©iStock/Vera_Petrunina Photo: iStock/gorodenkoff
Photo: iStock/gorodenkoff Photo for illustrative purposes only. ©iStock/Jelena Danilovic
Photo for illustrative purposes only. ©iStock/Jelena Danilovic Illustration ©iStock/laramenko
Illustration ©iStock/laramenko Photo by Robin DeMark
Photo by Robin DeMark Photo by Mitch Mirkin
Photo by Mitch Mirkin Photo: ©iStock/PongMoji
Photo: ©iStock/PongMoji Photo: ©iStock/Nicolas_
Photo: ©iStock/Nicolas_ Illustration: ©iStock/Mohammed Haneefa Nizmudeen
Illustration: ©iStock/Mohammed Haneefa Nizmudeen Photo for illustrative purposes only. ©iStock/grandriver
Photo for illustrative purposes only. ©iStock/grandriver Photo: iStock/sturti
Photo: iStock/sturti Photo: iStock/sassy1902
Photo: iStock/sassy1902 Photo for illustrative purposes only. ©iStock/Ridofranz
Photo for illustrative purposes only. ©iStock/Ridofranz Photo: ©iStock/JTSorrell
Photo: ©iStock/JTSorrell Photo: ©iStock/busracavus
Photo: ©iStock/busracavus Photo for illustrative purposes only. ©iStock/Wavebreakmedia
Photo for illustrative purposes only. ©iStock/Wavebreakmedia Photo for illustrative purposes only. ©iStock/electravk
Photo for illustrative purposes only. ©iStock/electravk Photo: ©iStock/iLexx
Photo: ©iStock/iLexx Photo: ©iStock/lolostock
Photo: ©iStock/lolostock Photo: ©iStock/digitalskillet
Photo: ©iStock/digitalskillet Photo: ©iStock/EXTREME-PHOTOGRAPHER
Photo: ©iStock/EXTREME-PHOTOGRAPHER Photo: ©iStock/malgorzata tatarynowicz
Photo: ©iStock/malgorzata tatarynowicz Photo for illustrative purposes only. ©iStock/Westbury
Photo for illustrative purposes only. ©iStock/Westbury Photo: ©iStock/Laurence Dutton
Photo: ©iStock/Laurence Dutton Photo for illustrative purposes only. ©iStock/Steve Debenport
Photo for illustrative purposes only. ©iStock/Steve Debenport Photo: ©iStock/skynesher
Photo: ©iStock/skynesher Photo for illustrative purposes only: ©iStock/sturti
Photo for illustrative purposes only: ©iStock/sturti Photo: ©iStock/SerafinoMozzo
Photo: ©iStock/SerafinoMozzo Photo: ©iStock/spxChrome
Photo: ©iStock/spxChrome Photo for illustrative purposes only. ©iStock/asiseeit
Photo for illustrative purposes only. ©iStock/asiseeit Illustration: ©iStock/Lars Neumann
Illustration: ©iStock/Lars Neumann Photo for illustrative purposes only. ©iStock/PeopleImages
Photo for illustrative purposes only. ©iStock/PeopleImages Photo: ©iStock/emesilva
Photo: ©iStock/emesilva Photo: ©iStock/Henrik5000w
Photo: ©iStock/Henrik5000w Photo: ©iStock/noipornpan
Photo: ©iStock/noipornpan Photo: ©iStock/Tharakorn
Photo: ©iStock/Tharakorn Photo: ©iStock/Andresr
Photo: ©iStock/Andresr (Photo for illustrative purposes only. DoD/Navy Petty Officer 1st Class Daniel Barker)
(Photo for illustrative purposes only. DoD/Navy Petty Officer 1st Class Daniel Barker) Photo: ©iStock/Solange_Z
Photo: ©iStock/Solange_Z Photo: ©iStock/Henrik5000w
Photo: ©iStock/Henrik5000w Photo by Mitch Mirkin
Photo by Mitch Mirkin Photo: ©iStock/gorodenko
Photo: ©iStock/gorodenko Photo: ©iStock/zmeel
Photo: ©iStock/zmeel Photo: ©iStock/Martin Dimitrov
Photo: ©iStock/Martin Dimitrov Photo for illustrative purposes only.©iStock/Highwaystarz-Photography
Photo for illustrative purposes only.©iStock/Highwaystarz-Photography Photo for illustrative purposes only. ©iStock/Tinpixels
Photo for illustrative purposes only. ©iStock/Tinpixels Photo: ©iStock/Utah778
Photo: ©iStock/Utah778 Photo for illustrative purposes only. ©iStock/Westbury
Photo for illustrative purposes only. ©iStock/Westbury Photo: ©iStock/SVproduction
Photo: ©iStock/SVproduction Photo: ©iStock/vadimguzhva
Photo: ©iStock/vadimguzhva Photo: ©iStock/lechatnoir
Photo: ©iStock/lechatnoir Illustration: ©iStock/mr.suphachai praserdumrongchai
Illustration: ©iStock/mr.suphachai praserdumrongchai Photo for illustrative purposes only. ©iStock/monkeybusinessimages
Photo for illustrative purposes only. ©iStock/monkeybusinessimages Photo for illustrative purposes only. ©iStock/asiseeit
Photo for illustrative purposes only. ©iStock/asiseeit Photo: ©iStock/PeopleImages
Photo: ©iStock/PeopleImages Photo: ©iStock/Pornpak Khunatorn
Photo: ©iStock/Pornpak Khunatorn Photo for illustrative purposes only. ©iStock/shapecharge
Photo for illustrative purposes only. ©iStock/shapecharge Photo: ©iStock/Luso
Photo: ©iStock/Luso Photo: ©iStock/fotografixx
Photo: ©iStock/fotografixx Photo: ©iStock/asiseeit
Photo: ©iStock/asiseeit Photo for illustrative purposes only. ©iStock/LumiNola
Photo for illustrative purposes only. ©iStock/LumiNola Photo for illustrative purposes only. ©iStock/Zinkevych
Photo for illustrative purposes only. ©iStock/Zinkevych Photo: ©iStock/wwing
Photo: ©iStock/wwing Photo: ©iStock/Xsandra
Photo: ©iStock/Xsandra Photo: ©iStock/memorisz
Photo: ©iStock/memorisz Illustration: ©iStock/yodiyim
Illustration: ©iStock/yodiyim Photo by Michael Moody
Photo by Michael Moody Photo: ©iStock/DragonImages
Photo: ©iStock/DragonImages Photo by Kimberly DiDonato-Ferro
Photo by Kimberly DiDonato-Ferro Photo: ©iStock/Morsa Images
Photo: ©iStock/Morsa Images Photo: ©iStock/MarsBars
Photo: ©iStock/MarsBars Photo: ©iStock/Natali_Mis
Photo: ©iStock/Natali_Mis Photo: ©iStock/Steve Debenport
Photo: ©iStock/Steve Debenport Illustration: ©iStock/tampatra
Illustration: ©iStock/tampatra Illustration: National Institute of Mental Health
Illustration: National Institute of Mental Health Photo: ©iStock/Charles Wollertz
Photo: ©iStock/Charles Wollertz Photo: ©iStock/GummyBone
Photo: ©iStock/GummyBone Photo for illustrative purposes only. ©iStock/Geber86
Photo for illustrative purposes only. ©iStock/Geber86 Photo: ©iStock/PeopleImages
Photo: ©iStock/PeopleImages Illustration: ©iStock/wildpixel
Illustration: ©iStock/wildpixel Photo for illustrative purposes only. ©iStock/ljubaphoto
Photo for illustrative purposes only. ©iStock/ljubaphoto Illustration ©iStock/kh_art
Illustration ©iStock/kh_art Photo: ©iStock/solidcolours
Photo: ©iStock/solidcolours Photo: iStock/Toa55
Photo: iStock/Toa55 Photo: iStock/dra_schwartz
Photo: iStock/dra_schwartz Photo: iStock/KatarzynaBialasiewicz
Photo: iStock/KatarzynaBialasiewicz Photo: ©iStock/3alexd
Photo: ©iStock/3alexd Photo: ©iStock/Gio_tto
Photo: ©iStock/Gio_tto Illustration: ©iStock/Nerthuz
Illustration: ©iStock/Nerthuz Photo by Jeff Bowen
Photo by Jeff Bowen Photo for illustrative purposes only. ©iStock/monkeybusinessimages
Photo for illustrative purposes only. ©iStock/monkeybusinessimages Photo: ©iStock/wenht
Photo: ©iStock/wenht Photo by Jerry Daliege
Photo by Jerry Daliege Photo: ©iStock/PeopleImages
Photo: ©iStock/PeopleImages Photo: ©iStock/imaginima
Photo: ©iStock/imaginima Photo: ©iStock/DNY59
Photo: ©iStock/DNY59 Photo: ©iStock/lbodvar
Photo: ©iStock/lbodvar Photo: ©iStock/asiseeit
Photo: ©iStock/asiseeit  Photo: ©iStock/Wand_Prapan
Photo: ©iStock/Wand_Prapan Photo: ©iStock/happyphoton
Photo: ©iStock/happyphoton Photo: ©iStock/gece33
Photo: ©iStock/gece33 Photo: ©iStock/BlackJack3D
Photo: ©iStock/BlackJack3D Photo by Robert Turtil
Photo by Robert Turtil ©iStock/bagi1998
©iStock/bagi1998 Photo: ©iStock/kasto80
Photo: ©iStock/kasto80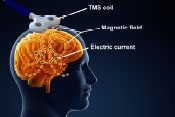 Brain illustration: ©iStock/cosmin4000
Brain illustration: ©iStock/cosmin4000 Photo for illustrative purposes only. ©iStock/PeopleImages
Photo for illustrative purposes only. ©iStock/PeopleImages Photo for illustrative purposes only. ©iStock/gilaxia
Photo for illustrative purposes only. ©iStock/gilaxia Photo: ©iStock/Hotaik Sung
Photo: ©iStock/Hotaik Sung Photo: ©iStock/Tashi-Delek
Photo: ©iStock/Tashi-Delek Photo for illustrative purposes only. ©iStock/Chalffy
Photo for illustrative purposes only. ©iStock/Chalffy Photo: ©iStock/JanIngeskogheim
Photo: ©iStock/JanIngeskogheim Photo: ©iStock/Henrik5000w
Photo: ©iStock/Henrik5000w Photo: ©iStock/LPETTET
Photo: ©iStock/LPETTET Photo: ©iStock/jxfzsy
Photo: ©iStock/jxfzsy Photo: ©iStock/JacobStudio
Photo: ©iStock/JacobStudio Photo: ©iStock/vm
Photo: ©iStock/vm Photo: ©iStock/Vasyl Dolmatov
Photo: ©iStock/Vasyl Dolmatov Photo for illustrative purposes only. ©iStock fergusowen
Photo for illustrative purposes only. ©iStock fergusowen Photo: ©iStock/Wavebreakmedia
Photo: ©iStock/Wavebreakmedia Photo by Derrick Morin
Photo by Derrick Morin Photo for illustrative purposes only. ©iStock/BraunS
Photo for illustrative purposes only. ©iStock/BraunS Photo for illustrative purposes only. ©iStock/laflor
Photo for illustrative purposes only. ©iStock/laflor Photo for illustrative purposes only. ©iStock/PeopleImages
Photo for illustrative purposes only. ©iStock/PeopleImages Illustration: ©iStock/goa_novi
Illustration: ©iStock/goa_novi U.S. Army, via Wikimedia Commons
U.S. Army, via Wikimedia Commons ©iStock/domoyega
©iStock/domoyega ©iStock/SeventyFour
©iStock/SeventyFour ©iStock/MladenZivkovic
©iStock/MladenZivkovic Photo for illustrative purposes only. ©iStock/South_agency
Photo for illustrative purposes only. ©iStock/South_agency Photo: ©iStock/PeopleImages
Photo: ©iStock/PeopleImages Photo: ©iStock/vchal
Photo: ©iStock/vchal Photo: ©iStock/RomoloTavani
Photo: ©iStock/RomoloTavani Photo: ©iStock/stevecoleimages
Photo: ©iStock/stevecoleimages Photo for illustrative purposes only. ©iStock/jacoblund
Photo for illustrative purposes only. ©iStock/jacoblund Photo for illustrative purposes only. ©iStock/KatarzynaBialasiewicz
Photo for illustrative purposes only. ©iStock/KatarzynaBialasiewicz Photo: ©iStock/VladimirSorokin
Photo: ©iStock/VladimirSorokin Photo for illustrative purposes only. ©iStock/Wavebreakmedia
Photo for illustrative purposes only. ©iStock/Wavebreakmedia Photo: ©iStock/solidcolours
Photo: ©iStock/solidcolours Photo for illustrative purposes only. ©iStock/ClarkandCompany
Photo for illustrative purposes only. ©iStock/ClarkandCompany Photo: ©iStock/LeoPatrizi
Photo: ©iStock/LeoPatrizi Photo: ©iStock/Natali_Mis
Photo: ©iStock/Natali_Mis Photo by Robert Turtil, for illustrative purposes only.
Photo by Robert Turtil, for illustrative purposes only. Photo for illustrative purposes only. ©iStock/FatCamera
Photo for illustrative purposes only. ©iStock/FatCamera Photo: ©iStock/Ivcandy
Photo: ©iStock/Ivcandy Photo: ©iStock/courtneyk
Photo: ©iStock/courtneyk Photo: ©iStock/dusanpetkovic
Photo: ©iStock/dusanpetkovic Photo: ©iStock/davidperks
Photo: ©iStock/davidperks Photo: ©iStock/D-Keine
Photo: ©iStock/D-Keine Photo: ©iStock/Ivan-balvan
Photo: ©iStock/Ivan-balvan Photo for illustrative purposes only. ©iStock/laflor
Photo for illustrative purposes only. ©iStock/laflor Photo: ©iStock/Sasha_Suzi
Photo: ©iStock/Sasha_Suzi Photo: ©iStock/theasis
Photo: ©iStock/theasis Image courtesy of Dr. Albert Leung
Image courtesy of Dr. Albert Leung Photo by Robert Turtil
Photo by Robert Turtil Photo: ©iStock/Dr_Microbe
Photo: ©iStock/Dr_Microbe Photo for illustrative purposes only. ©Stock/Tempura
Photo for illustrative purposes only. ©Stock/Tempura Photo: ©iStock/porpeller
Photo: ©iStock/porpeller Photo: ©iStock/Donghero
Photo: ©iStock/Donghero Photo by Jerry Daliege
Photo by Jerry Daliege Photo: ©iStock/KarenMassier
Photo: ©iStock/KarenMassier Photo: ©iStock/amesy
Photo: ©iStock/amesy Photo: ©iStock/chameleonseye
Photo: ©iStock/chameleonseye Photo for illustrative purposes only. ©iStock/XiXinXing
Photo for illustrative purposes only. ©iStock/XiXinXing Photo: ©iStock/efks
Photo: ©iStock/efks Photo for illustrative purposes only. ©iStock/seb_ra
Photo for illustrative purposes only. ©iStock/seb_ra Photo: ©iStock/kali9
Photo: ©iStock/kali9 Photo: ©iStock/wildpixel
Photo: ©iStock/wildpixel Photo: ©iStock/kieferpix
Photo: ©iStock/kieferpix Photo by Petty Officer 1st Class Holly L. Herline/USN
Photo by Petty Officer 1st Class Holly L. Herline/USN Photo: ©iStock/kupicoo
Photo: ©iStock/kupicoo Photo: ©iStock/digihelion
Photo: ©iStock/digihelion Photo: ©iStock/porpelle
Photo: ©iStock/porpelle Photo: Mitch Mirkin
Photo: Mitch Mirkin Photo for illustrative purposes only: ©iStock/kali9
Photo for illustrative purposes only: ©iStock/kali9 Photo: ©iStock/sercan samanci
Photo: ©iStock/sercan samanci Photo for illustrative purposes only: ©iStock/debibishop
Photo for illustrative purposes only: ©iStock/debibishop Photo: ©iStock/Evgeny Gromov
Photo: ©iStock/Evgeny Gromov Photo: ©iStock/kitzcorner
Photo: ©iStock/kitzcorner Photo: ©iStock/tinors
Photo: ©iStock/tinors Photo courtesy of www.xenex.com
Photo courtesy of www.xenex.com ©iStock/Duka82
©iStock/Duka82 Adapted from JN article
Adapted from JN article Photo: ©iStock/NanoStockk
Photo: ©iStock/NanoStockk Photo: ©iStock/RomaRiolen
Photo: ©iStock/RomaRiolen Photo: ©iStock/jhorrocks
Photo: ©iStock/jhorrocks Photo: ©iStock/evryka23
Photo: ©iStock/evryka23 Photo for illustrative purposes only. ©iStock/RapidEye
Photo for illustrative purposes only. ©iStock/RapidEye Photo for illustrative purposes only. ©iStock/Wavebreakmedia
Photo for illustrative purposes only. ©iStock/Wavebreakmedia Photo: ©iStock/Dr._Microbe
Photo: ©iStock/Dr._Microbe Photo for illustrative purposes only. ©iStock/Steve Debenport
Photo for illustrative purposes only. ©iStock/Steve Debenport Photo for illustrative purposes only. ©iStock/GlobalStock
Photo for illustrative purposes only. ©iStock/GlobalStock Photo: ©iStock/Natali_Mis
Photo: ©iStock/Natali_Mis Photo: ©iStock/wildpixel
Photo: ©iStock/wildpixel Photo: ©iStock/AndreyPopov
Photo: ©iStock/AndreyPopov Photo: ©iStock/PeopleImages
Photo: ©iStock/PeopleImages Photo: Christopher Pacheco
Photo: Christopher Pacheco Photo: ©iStock/JTSorrell
Photo: ©iStock/JTSorrell Photo: ©iStock/yodiyim
Photo: ©iStock/yodiyim Photo: ©iStock/jamesbenet
Photo: ©iStock/jamesbenet Photo: USMC
Photo: USMC Photo for illustrative purposes only. ©iStock/Lyashik
Photo for illustrative purposes only. ©iStock/Lyashik Photo for illustrative purposes only. ©iStock/juanmonino
Photo for illustrative purposes only. ©iStock/juanmonino Photo by Cpl. Manuel Serrano/USMC
Photo by Cpl. Manuel Serrano/USMC Photo courtesy of Tampa VAMC
Photo courtesy of Tampa VAMC Image courtesy of study authors
Image courtesy of study authors ©iStock/Highwaystarz-Photography
©iStock/Highwaystarz-Photography Photo:©iStock/Dusan Vidar
Photo:©iStock/Dusan Vidar Photo: ©Stock/artenex
Photo: ©Stock/artenex Photo:©iStock/onairjiw
Photo:©iStock/onairjiw Photo for illustrative purposes only. ©iStock/g-stockstudio
Photo for illustrative purposes only. ©iStock/g-stockstudio Photo ©iStock/adventtr
Photo ©iStock/adventtr Photo:©iStock/Nicolesy
Photo:©iStock/Nicolesy Photo:©iStock/Hailshadow
Photo:©iStock/Hailshadow Photo:©iStock/Rpsycho
Photo:©iStock/Rpsycho Photo: Wikimedia Commons
Photo: Wikimedia Commons Photo: ©iStock/laflor
Photo: ©iStock/laflor Photo: ©iStock/OcusFocus
Photo: ©iStock/OcusFocus Photo: ©Stock/Ondroo
Photo: ©Stock/Ondroo Photo: ©Stock/fluxfoto
Photo: ©Stock/fluxfoto Photo: ©Stock/portishead1
Photo: ©Stock/portishead1 Photo for illustrative purposes only. ©iStock/kieferpix
Photo for illustrative purposes only. ©iStock/kieferpix Photo: ©iStock/marrio31
Photo: ©iStock/marrio31 Photo ©iStock/KentWeakley
Photo ©iStock/KentWeakley Photo ©iStock/D-Keine
Photo ©iStock/D-Keine Image from Bone Research via Creative Commons
Image from Bone Research via Creative Commons Photo: ©iStock/PeopleImages
Photo: ©iStock/PeopleImages Photo by Mitch Mirkin
Photo by Mitch Mirkin Photo for illustrative purposes only. ©iStock/Vadimguzhva
Photo for illustrative purposes only. ©iStock/Vadimguzhva Photo: ©iStock/Darwin Brandis
Photo: ©iStock/Darwin Brandis Photo: ©iStock/CheshireCat
Photo: ©iStock/CheshireCat Photo by Master Sgt. Mark C. Olsen
Photo by Master Sgt. Mark C. Olsen Photo: ©iStock/yodiyim
Photo: ©iStock/yodiyim Photo: ©iStock/shironosov
Photo: ©iStock/shironosov Photo courtesy of xenex.com
Photo courtesy of xenex.com Photo: ©iStock/ands456
Photo: ©iStock/ands456 Photo for illustrative purposes only. ©iStock/Halfpoint
Photo for illustrative purposes only. ©iStock/Halfpoint Photo for illustrative purposes only. ©iStock/domoyega
Photo for illustrative purposes only. ©iStock/domoyega Photo: ©iStock/domoyega
Photo: ©iStock/domoyega  Photo: ©iStock/LPETTET
Photo: ©iStock/LPETTET Photo: ©iStock/jamesbenet
Photo: ©iStock/jamesbenet Photo: ©iStock/dra_schwartz
Photo: ©iStock/dra_schwartz Photo: ©iStock/cherrybeans
Photo: ©iStock/cherrybeans Photo: ©iStock/Cecile_Arcurs
Photo: ©iStock/Cecile_Arcurs Photo: ©iStock/Thomas_EyeDesign
Photo: ©iStock/Thomas_EyeDesign Photo: ©iStock/solidcolours
Photo: ©iStock/solidcolours Photo: ©iStock/porpeller
Photo: ©iStock/porpeller Photo: ©iStock/nicolas
Photo: ©iStock/nicolas Photo: ©iStock/Morrhigan
Photo: ©iStock/Morrhigan Photo: ©iStock/RoBeDeRo
Photo: ©iStock/RoBeDeRo Photo: ©iStock/Martin Prescott
Photo: ©iStock/Martin Prescott Photo: ©iStock/selvanegra
Photo: ©iStock/selvanegra Photo: ©iStock/fstop123
Photo: ©iStock/fstop123 Photo by Sgt. Richard Blumenstein/USMC
Photo by Sgt. Richard Blumenstein/USMC  Photo: ©iStock/choja
Photo: ©iStock/choja Photo: ©iStock/thomasandreas
Photo: ©iStock/thomasandreas Photo for illustrative purposes only. ©iStock/KatarzynaBialasiewicz
Photo for illustrative purposes only. ©iStock/KatarzynaBialasiewicz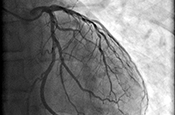 Photo: ©iStock/kalus
Photo: ©iStock/kalus Photo: ©iStock/mixetto
Photo: ©iStock/mixetto Photo by Scott R. Galvin
Photo by Scott R. Galvin Photo: ©iStock/sdominick
Photo: ©iStock/sdominick Photo courtesy of Bedford VAMC
Photo courtesy of Bedford VAMC Photo: ©iStock/designer491
Photo: ©iStock/designer491 Photo for illustrative purposes only. ©iStock/Photawa
Photo for illustrative purposes only. ©iStock/Photawa Photo: ©iStock/adventtr
Photo: ©iStock/adventtr Photo: ©iStock/Mark_Hubsky
Photo: ©iStock/Mark_Hubsky Photo: ©iStock/lolostock
Photo: ©iStock/lolostock Photo for illustrative purposes only. ©iStock/Marjan_Apostolovic
Photo for illustrative purposes only. ©iStock/Marjan_Apostolovic Photo: ©iStock/kali9
Photo: ©iStock/kali9 Photo: ©iStock/PeopleImages
Photo: ©iStock/PeopleImages
 Photo: ©iStock/malgorzata tatarynowicz
Photo: ©iStock/malgorzata tatarynowicz Photo: ©iStock/ viola83181
Photo: ©iStock/ viola83181 Photo: ©iStock/bowdenimages
Photo: ©iStock/bowdenimages Photo: ©iStock/eyenigelen
Photo: ©iStock/eyenigelen Photo: ©iStock/andesr
Photo: ©iStock/andesr Photo: ©iStock/pixologicstudio
Photo: ©iStock/pixologicstudio Coast Guard photo by Petty Officer 3rd Class Eric D. Woodall
Coast Guard photo by Petty Officer 3rd Class Eric D. Woodall Photo for illustrative purposes only. ©iStock/shironosov
Photo for illustrative purposes only. ©iStock/shironosov Photo for illustrative purposes only. ©iStock
Photo for illustrative purposes only. ©iStock Photo for illustrative purposes only. ©iStock/Marjan_Apostolovic
Photo for illustrative purposes only. ©iStock/Marjan_Apostolovic Photo: U.S. Army
Photo: U.S. Army 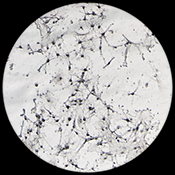 Photo: ©iStock/defun
Photo: ©iStock/defun For illustrative purposes only. Photo: ©iStock/digitalskillet
For illustrative purposes only. Photo: ©iStock/digitalskillet Photo: ©iStock/LPETTET
Photo: ©iStock/LPETTET Photo: ©iStock/WanjaJacob
Photo: ©iStock/WanjaJacob Photo: ©iStock/meen_na
Photo: ©iStock/meen_na Photo: ©iStock/Raycat
Photo: ©iStock/Raycat Photo: ©iStock/zilli
Photo: ©iStock/zilli Photo: ©iStock/Hailshadow
Photo: ©iStock/Hailshadow Photo: ©iStock/solidcolours
Photo: ©iStock/solidcolours Photo: ©iStock/ballero
Photo: ©iStock/ballero Army photo by Staff Sgt. Jennifer Bunn. For illustrative purposes only.
Army photo by Staff Sgt. Jennifer Bunn. For illustrative purposes only. Photo for illustrative purposes only. ©iStock/digitalskillet
Photo for illustrative purposes only. ©iStock/digitalskillet Photo: ©iStock/yodiyim
Photo: ©iStock/yodiyim Photo: ©iStock/monkeybusinessimages
Photo: ©iStock/monkeybusinessimages Photo: ©iStock/OGphoto
Photo: ©iStock/OGphoto Photo: ©iStock/Nikada
Photo: ©iStock/Nikada Photo for illustrative purposes only. ©iStock/Squaredpixels
Photo for illustrative purposes only. ©iStock/Squaredpixels Photo: ©iStock/knape
Photo: ©iStock/knape Photo: ©iStock/Steve Debenport
Photo: ©iStock/Steve Debenport Photo: ©iStock/ChrisChrisW
Photo: ©iStock/ChrisChrisW Photo for illustrative purposes only. ©iStock/Marjan_Apostolovic
Photo for illustrative purposes only. ©iStock/Marjan_Apostolovic Photo: ©iStock/Tinpixels
Photo: ©iStock/Tinpixels Photo: ©iStock/trekandshoot
Photo: ©iStock/trekandshoot Photo: ©iStock/Barmaleeva
Photo: ©iStock/Barmaleeva Photo: ©iStock/ksass
Photo: ©iStock/ksass Photo: ©princessdlaf
Photo: ©princessdlaf Photo by Kevin Walsh
Photo by Kevin Walsh Photo: ©iStock/kevinruss
Photo: ©iStock/kevinruss Photo: ©iStock/sudok1
Photo: ©iStock/sudok1 Photo: ©iStock/vitanovski
Photo: ©iStock/vitanovski Photo: ©iStock/vadimguzhva
Photo: ©iStock/vadimguzhva Photo: ©iStock/Solange_Z
Photo: ©iStock/Solange_Z Photo: ©iStock/michaeljung
Photo: ©iStock/michaeljung Photo: ©iStock/spanteldotru
Photo: ©iStock/spanteldotru Photo: ©istock/beerkoff
Photo: ©istock/beerkoff Photo: ©istock/selvanegra
Photo: ©istock/selvanegra Photo: Tech. Sgt. H. Deffner, U.S. Army
Photo: Tech. Sgt. H. Deffner, U.S. Army Photo for illustrative purposes only. ©iStock/bowdenimages
Photo for illustrative purposes only. ©iStock/bowdenimages Photo for illustrative purposes only. ©iStock/lovro77
Photo for illustrative purposes only. ©iStock/lovro77 Photo: ©iStock/vitanovski
Photo: ©iStock/vitanovski Photo: ©iStock/BVDC
Photo: ©iStock/BVDC DoD photo by Lance Cpl. Immanuel Johnson
DoD photo by Lance Cpl. Immanuel Johnson ©iStock/bagi1998
©iStock/bagi1998 Photo: ©iStock/Scharvik
Photo: ©iStock/Scharvik Photo: ©iStock/spanteldotru
Photo: ©iStock/spanteldotru Photo: ©iStock/luchsche
Photo: ©iStock/luchsche Photo: Jason Miller
Photo: Jason Miller Photo: ©iStock/sturti
Photo: ©iStock/sturti Photo: ©iStock/RapidEye
Photo: ©iStock/RapidEye Photo by April Eilers
Photo by April Eilers Photo for illustrative purposes only. ©iStock/Highwaystarz-Photography
Photo for illustrative purposes only. ©iStock/Highwaystarz-Photography Photo: ©iStock/LeoPatrizi
Photo: ©iStock/LeoPatrizi Photo: Staff Sgt. William Tremblay/USA
Photo: Staff Sgt. William Tremblay/USA Photo: ©iStock/Eva-Katalin
Photo: ©iStock/Eva-Katalin Courtesy of EOS Surfaces
Courtesy of EOS Surfaces Photo: ©iStock/emesilva
Photo: ©iStock/emesilva Photo: ©iStock/jarun011
Photo: ©iStock/jarun011 Photo: Ames Laboratory, U.S. Dept. of Energy
Photo: Ames Laboratory, U.S. Dept. of Energy Photo: ©iStock/yodiyim
Photo: ©iStock/yodiyim Photo by Mitch Mirkin
Photo by Mitch Mirkin ©iStock/gilaxia
©iStock/gilaxia ©Stock/marekuliasz
©Stock/marekuliasz ©Stock/sshepard
©Stock/sshepard ©Stock/stockdevil
©Stock/stockdevil ©iStock/sudok1
©iStock/sudok1 ©iStock/ChesiireCat
©iStock/ChesiireCat ©iStock/blueringmedia
©iStock/blueringmedia Photo: ©iStock/Kwangmoozaa
Photo: ©iStock/Kwangmoozaa A Veteran receives an explanation of the Wii-Fit from Dr. Kalpana Padala at the Central Arkansas Healthcare System. (Photo by Jeff Bowen)
A Veteran receives an explanation of the Wii-Fit from Dr. Kalpana Padala at the Central Arkansas Healthcare System. (Photo by Jeff Bowen) Photo: ©iStock/kali9
Photo: ©iStock/kali9 ©iStock/Sutthaburawonk
©iStock/Sutthaburawonk ©iStock/Steve Debenport
©iStock/Steve Debenport ©iStock/Image Source
©iStock/Image Source ©iStock/Scharvik
©iStock/Scharvik ©iStock/javi_indy
©iStock/javi_indy ©iStock/monkeybusinessimages
©iStock/monkeybusinessimages Photo: ©iStock/MikeyGen73
Photo: ©iStock/MikeyGen73 Photo: ©iStock/FikMik
Photo: ©iStock/FikMik Photo: ©iStock/AlexRaths
Photo: ©iStock/AlexRaths
 Photo: ©iStock/yodiyim
Photo: ©iStock/yodiyim Photo: ©iStock/simarik
Photo: ©iStock/simarik Photo: ©iStock/lentolo
Photo: ©iStock/lentolo Photo: ©iStock/FatCamera
Photo: ©iStock/FatCamera Photo: Airman 1st Class Christopher Griffin/USAF
Photo: Airman 1st Class Christopher Griffin/USAF Photo: ©iStock/selvanegra
Photo: ©iStock/selvanegra Photo: ©iStock/bloodstone
Photo: ©iStock/bloodstone Photo: ©iStock/PeopleImages
Photo: ©iStock/PeopleImages Photo ©iStock/stock colors
Photo ©iStock/stock colors Photo ©iStock/shironosov
Photo ©iStock/shironosov Photo ©iStock/sturti
Photo ©iStock/sturti Photo: ©iStock/Wavebreak
Photo: ©iStock/Wavebreak Photo courtesy of Australian Army
Photo courtesy of Australian Army Photo: ©iStock/ Imagesbybarbara
Photo: ©iStock/ Imagesbybarbara Photo: ©iStock/ Johnny Greig
Photo: ©iStock/ Johnny Greig Photo courtesy of www.gulflink.osd.mil
Photo courtesy of www.gulflink.osd.mil
 Photo: ©iStock/efks
Photo: ©iStock/efks (Photo courtesy of Pan lab)
(Photo courtesy of Pan lab) Photo: ©iStock/ands456
Photo: ©iStock/ands456




