Office of Research & Development |
 |


Dr. Richard Weir displays a prototype for one of his ongoing projects. It calls for developing a mechanical finger that can be sized for a female hand using 3D printing technology. (Photo by Terri Rorke)
November 17, 2020
By Mike Richman
VA Research Communications
Dr. Richard Weir is a self-dubbed “sci-fi geek.”
His favorite movies include 21st century science fiction thrillers “Surrogates,” “Ready Player One,” and “Iron Man,” as well as “Star Wars,” “Blade Runner,” and “Robocop” from years back. He has absorbed the readings of renowned sci-fi authors David Brin and Iain Banks.
With a seemingly endless supply of curiosity, Weir does a lot of mental doodling and diagramming. He also likes to make things.
"We have to do the engineering to put it into a form and shape so it will work in the body."
“I can’t help myself,” says Weir, an expert in prosthetics technology at the VA Eastern Colorado Healthcare System. “I read so much science fiction. So maybe my ideas aren’t completely strange to me. I guess you get exposed to ideas. Then you see if the idea has merit or not. You can work it from there. A lot of times, I get ideas and it’s like, `Oh, I see pieces from different places, and I see how they go together.”
Today, Weir is doing just that. In his latest technological challenge, he’s co-leading the development of an innovative power source for wearable devices like prostheses and implantable devices, such as pacemakers or deep brain stimulators, that will harvest electricity from blood sugar. If successful, the technology will be the first of its kind.
In theory, the power source could be used for anything that’s worn on the body and needs electricity, Weir says. He and his colleagues are confident that the components needed to create such a device are in place. They also believe an opportunity exists to develop a system that optimizes and integrates those components to produce a viable system in size, power, and efficiency.

VA engineering research center posts another invention: prosthetic hook mouse

VA scientists testing new technology to absorb moisture, increase comfort with prostheses

Study probes user satisfaction with upper-limb prostheses

Researchers piloting nerve stimulation for amputation pain
That’s because of the invention of a cloth-like membrane—an anion exchange membrane—that can generate electricity in a high pH (acidity) environment like the body when blood flows over and-or through the membrane. Human blood is full of glucose, which is a form of sugar and a source of fuel for the body. The membrane reacts with those sugars and creates electricity as a by-product of the reaction. This electricity can be stored in a battery for later use to provide power for both implanted and external devices, according to Weir.
“It is the membrane that allows us to work with these sugars,” says Weir, who is also a professor of bioengineering at the University of Denver. “In the body, things are at a particular acidity. So we thought, `Let’s have a look at these membranes and see if we can use them with blood sugar.’ People have been trying to do implanted power systems that use blood sugars for a while, but they’ve always run into problems. That’s why we think our membrane is the thing that will enable us to succeed where others have not.
“We have to do the engineering, though, to put it into a form and shape so it will work in the body,” he adds. “There’s a lot of difference between moving a device from benchtop proof-of-concept to getting it into a form suitable for use even as an out-of-the-body type of fuel cell and then moving from an external system into an implanted system. We have a lot to do to develop the membrane from a prototype system into a physically realizable system.”
It’s important to maximize blood flow over and-or through the membrane, Weir explains, in order to increase the amount of contact between the two and produce high levels of electricity. Glucose in the blood will react chemically with coatings on the membrane, he adds.
“That makes the glucose give up some electrons that we can then use for electricity,” he says. “Electricity is nothing more than the flow or movement of electrons, so the moment we have something that can create or generate electrons, we harvest those and use them to power devices, assuming we can get enough. We’ll have to supply some oxygen to it, as well. The reaction of the oxygen and glucose with the membrane will produce the electricity. It’s basically a linear thing whereby the more blood we can have in contact with the membrane, the more electricity we can make.”
Dr. Chulsung Bae, a professor at Rensselaer Polytechnic Institute in New York, is supplying the anion exchange membrane. Bae is a colleague of Dr. John Pellegrino, a professor at the University of Colorado and a collaborator of Weir on the blood sugar project.
They are working on the technology in Weir’s lab at the Rocky Mountain Regional VA Medical Center in Denver. Scientists in the lab specialize in building prosthetic hands for people with upper-limb loss. Dr. Jacob Segil, a mentee of Weir, is also involved in the blood sugar project. He focuses on building special sensors that fit into prosthetic fingertips and bring a sense of touch.
Weight is a major factor in the success of prostheses and implantable devices. Weir and his colleagues are always trying to make prosthetic hands that are light, compact, and as powerful as possible. Their new technology, he says, could replace the batteries with a handkerchief-sized piece of fabric-like membrane that would provide continuous power. “It’s living in you, so you wouldn’t need to re-charge batteries,” he says. “We’d be harvesting power from your body continuously.”
The desire to produce small, light, and powerful sources makes Weir and his team eager to figure out new and better ways to generate power and electricity.
“That led to some discussions with Dr. Pellegrino on this proposal,” Weir recalls. “He said, `Why don’t you go directly to the source and use blood sugar. Sugar has a really high energy content.’ So it’s like, `Okay, that’s interesting.’ Gasoline is a liquid in your fuel tank. It contains a whole lot of energy. Then it’s released when it goes into the engine and is ignited by the sparkplugs. When it’s stored, it’s stored in a liquid form, so it’s a very compact sort of energy. Sugar is kind of the same way. Sugar beets and sugar cane are used as alternative biofuels because they have a real high energy content or what we call specific energy. That makes sugar an excellent fuel source.”
Weir and his team are at least a year away from testing a prosthesis that will demonstrate the concept of the membrane using sugar as a fuel. That will be accomplished on a benchtop system, he says, noting that he and his colleagues will start with the hand because “that’s our comfort zone.” For the future, it’s possible to envision a scenario in which the blood sugar flows through a tube on the skin to an instrument linked to the prosthesis.
But a fully implantable system in which blood sugar is powering something like a deep brain stimulator is years away, he notes.
“Whenever surgery is needed to put a device into somebody, that takes a long time to make it through human trials,” Weir says. Case in point: He led a team that developed an implantable sensor system that measured muscle signals. The goal of the project was to acquire prosthesis control signals from all 18 forearm muscles through implantable myoelectric sensors (IMES). It took about a decade, he says, for the project to go from initial funding to initial testing in human trials.
“It takes a long time before these technologies make it to humans,” he says. “We’re putting an implanted membrane into the body and using blood sugar in a person. We have to go through animal trials first and a bunch of other steps before it can get into people.”
Weir has long been a VA leader in prosthetic technology. More than a decade ago, he and his colleagues contributed to an effort funded by the Defense Advanced Research Projects (DARPA) to build the world’s most advanced prosthetic arm. They partnered with a private firm and the Applied Physics Lab at Johns Hopkins University in Baltimore to build a 15-motor hand for an arm system that was unveiled in 2007. The system is now being further developed.
Weir also consulted on the LUKE/DEKA arm, which was developed through the same DARPA initiative. VA researchers were key to testing and optimizing the LUKE/DEKA arm, the first prosthetic arm capable of performing multiple simultaneous powered movements. The U.S. Food and Drug Administration approved it in 2014.
His latest technological adventure, he says, is not some fanciful hope or plan. He believes there’s solid science behind the idea. Among the colleagues he’s shared it with, none have expressed outright skepticism.
“Not to my face, anyway,” he says with a laugh. “At the moment, we can make a reasonable argument because the pieces are there. We can say, `Oh, this actually might work.’ That’s why we’re pursuing it. So it’s not completely pie in the sky because we know what’s gone on before, and we’re basing some of our initial choices and designs on sort of an existing type of technology. This may sound like science fiction, but I think a lot of it is a logical extension of how we can improve some of the systems that we see. I don’t know. There are always naysayers but there are also yeasayers, so you want to be positive in your outlook.”
VA is funding the project with a Small Projects in Rehabilitation Research (SPIRE) grant, which is usually for pilot-level, high-risk, high-reward endeavors.
“We have a peer-reviewed grant, so it’s been legitimized in that sense,” Weir says. “It’s very empowering to move forward with this idea and develop it further. A SPIRE award allows you to do innovative, high-risk types of projects so you can explore the idea to see if you can get any preliminary data and learn whether the idea works at all.”
In Weir’s opinion, the technology would be a “game changer because we would be able to make and harvest power from people themselves, without having to charge anything out of the wall. You just eat your chocolate bar or something, and then you’d be good to go.”
“This is just experimental, but it’s high-risk, high gain,” he says. “It has the potential to be very impactful if we can get it to work, even on a benchtop or external system. It would be a novel sort of fuel cell technology.”
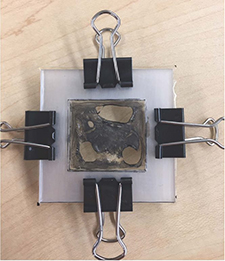
In a bench-top set up for the blood sugar-based fuel cell, the membrane is held by plastic pieces that are crimped together in the bolted assembly.
Like many technologies in their infancy, the idea of using blood sugar to fuel prostheses and implantable devices is triggering its share of questions. After all, prior attempts to use blood sugar as a power source have come up short. But while much about the technology may be speculative, its core concept is in place. The goal is to advance it to physical reality.
Dr. Richard Weir of VA Eastern Colorado, one of the scientists leading the project, addressed some of these questions:
--- Mike Richman
VA Research Currents archives || Sign up for VA Research updates