Office of Research & Development |
 |

In a study by a team that included a VA researcher, rats were fed a high-fat diet to induce weight gain and then treated successfully with a hormone-based drug that reduced food intake and body weight. (Photo for illustrative purposes only: ©GettyImages/fotografixx)
January 18, 2022
By Nancy Volkers
For VA Research Communications
"Obesity increases risk for heart disease, type 2 diabetes, cancer, and COVID-19-related hospitalization, as well as overall mortality. Designing any targeted intervention to lower disease burden is important."
A potent, long-lasting “cousin” of a naturally occurring hormone reduced food intake and body weight in a rat model of obesity, according to results published in September 2021 in the journal Frontiers in Physiology.
The researchers say the results “mark a new avenue in anti-obesity drug interventions” and could potentially lead to a safe, effective treatment for the problem, which affects some 4 in 10 Americans.
Dr. James E. Blevins of the VA Puget Sound Health Care System completed the study with colleagues from Seattle Children’s Research Institute; the University of Washington; Harvard Medical School; and OXT Therapeutics, Inc.
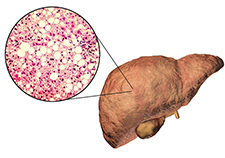
MVP study offers new insights on genetic risk for non-alcoholic fatty liver disease

Lab studies seek hormone-based obesity treatment

One-two punch helps Veterans with weight loss
The research focused on ASK1476, a human-made peptide with a structure similar to that of oxytocin.
Oxytocin is a protein-based hormone made by the brain. Studies have linked it with a wide variety of body functions and behaviors, including feeding, respiration, immune regulation, social memory, learning, digestion, pain perception, maternal behavior, and aggression. Because of its role in childbirth, maternal bonding, and romantic and sexual attraction, it is often called the “love hormone.”
Previous research suggests that administering oxytocin reduces food intake and prevents or reduces weight gain in animal models, as well as humans. However, oxytocin is quickly broken down in the body and cannot be taken by mouth. That’s why studies use injections or nasal administration.
Researchers created ASK1476 as a longer-lasting analogue of oxytocin. Blevins and colleagues have tested it for safety, effectiveness, and potential side effects.
“It's been exciting and fortunate to work with this group to address some of the limitations of oxytocin in terms of the short half-life,” said Blevins, who also is in the Division of Metabolism, Endocrinology and Nutrition at the University of Washington School of Medicine, Seattle. “There has been one study … that found intranasal oxytocin to elicit weight loss in men and women with obesity, but it required four daily intranasal administrations over eight weeks, and the weight loss was fairly modest. If we can find highly selective analogues that last longer and can be taken less frequently without causing any adverse effects, we'd be much better off.”
Before experiments started, rats were fed a high-fat diet (60% fat, 20% protein, 20% carbohydrate) for 15 weeks to induce weight gain. Then the group conducted preliminary experiments to determine the right doses for the study, followed by a 28-day intervention.
In the dose escalation phase, they gave the animals increasing doses of either oxytocin or ASK1476. Each dose was given for three days, followed by a two- to five-day washout period before the next higher dose began. The researchers saw reductions in food intake and loss of body weight at very low doses of both drugs. The human-made peptide was more potent, with an effective dose only one-fourth that of oxytocin. Neither drug affected water intake and neither appeared to cause nausea. These can be common effects of existing weight-loss drugs.
“ASK1476 had some very strong effects,” said lead author Dr. Christian Roth, with the Seattle Children’s Research Institute. “We had no concerns with fluid regulation, but we did have a few animals [receiving ASK1476] that died. We don’t yet know the reason, but we think it is linked to that specific molecule, so we are considering testing other peptides.”
The 28-day intervention included 24 rats, randomized to three groups that received ASK1476, oxytocin, or saline solution. The doses in the intervention were selected based on data from the dose-escalation experiment and were adjusted twice if needed. The final dose of ASK1476 was one-fifth the dose of oxytocin.
Animals receiving the drug treatments had initial decreases in body weight followed by a plateau in weight, whereas those receiving the control saline solution had increases in body weight. Both groups of drug-treated rats ate less over the 28-day period and were not more active than control rats.
By the end of the study, treated rats also had lower blood levels of leptin, triglycerides, and alanine aminotransferase, compared with control rats. Lower levels of these molecules generally correlate with better health.
“One thing we did not see was drug tolerance,” said Blevins. “Both of these drugs are competing against the body’s counter-regulatory systems that promote weight regain in response to weight loss, but we didn’t seem to see that with either oxytocin or ASK1476.”
Blevins noted that obesity is a major problem in the United States, including within the Veteran population. “Obesity increases risk for heart disease, type 2 diabetes, cancer, and COVID-19-related hospitalization, as well as overall mortality,” he said. “Designing any targeted intervention to lower disease burden is important.”
Weight loss also has been shown to lessen symptoms of PTSD, estimated to affect between 11% and 20% of Veterans. But current drug treatments for obesity can disturb sleep and often cause nausea and other gastrointestinal issues, Blevins said.
Most weight-loss drugs also cannot be used in children, another at-risk population, with more than 1 in 5 US children considered obese as of 2020.
“These studies are a critical first step in defining future therapies,” said Blevins.
Other evidence suggests that oxytocin has effects on blood pressure, fat balance, muscle mass, and bone strength. This makes studies on oxytocin and similar molecules relevant to an even larger percentage of Veterans, noted coauthor Dr. Alex Kiselyov, with OXT Therapeutics, Inc.
“For example, oxytocin's effect on adult muscle stem cells is very well-documented,” said Kiselyov. “It helps maintain muscle mass, which is important in an aging population.”
Blevins and colleagues are currently delving into studies of how these molecules work.
“Specifically, we are looking at whether other analogues elicit changes in gene expression as indicators of whether these analogues could be boosting energy expenditure by stimulating brown adipose tissue thermogenesis or converting white adipocyte [white fat] cells to more metabolically active brown adipocyte-like fat cells,” for example, Blevins said. “We are trying to better understand the mechanisms that drive the oxytocin analogue’s ability to promote weight loss.”
The researchers hope to test other molecules similar to ASK1476 to find safe and effective treatments for reducing the burden of obesity in Veterans and non-Veterans alike.
The study was funded by the National Institutes of Health, Seattle Children’s, the Department of Defense, and VA. Further funding details can be found in the journal article.
VA Research Currents archives || Sign up for VA Research updates