Office of Research & Development |
 |


Dr. Jose Aleman is director of the NY-MOVE! Endocrinology Weight Management Clinic at VA NY-Harbor Healthcare System. He is pictured with a medical student, Ms. Laetitia Zhang. (Photo by Michael Drake, VA NY-Harbor.)
July 23, 2021
By Erica Sprey
VA Research Communications
You've tried to do everything right. You've passed on the Buffalo chicken wings on poker night. You've cut back on alcohol and switched to light beer. You've even joined the local gym. Nothing seems to work—those extra 50 lbs. won't budge.
Well, you are not alone.
Obesity is a chronic disease where the pathways that control how much we eat can lead us to take in too many calories and accumulate excess fat that promotes health complications, says Dr. Jose O. Aleman, an endocrinologist at the VA New York Harbor Healthcare System, Manhattan Campus. When coupled with easy access to poorly nutritious food, individuals with obesity often struggle with their weight loss goals.
"I tell my Veteran patients that even though 10 pounds doesn't sound like a large amount of weight, it is the type of weight loss that tends to be sustainable."
Aleman is the director of the NY-MOVE! Endocrinology Weight Management Clinic at the NY-Harbor VA. He also leads clinical research to find the best ways to help Veterans reach a healthier weight.
Aleman and his team published a study in the journal Obesity that examined the effectiveness of pharmacotherapy—weight-loss medication—when combined with lifestyle changes. The study confirmed the benefits of medication, but noted significant variability among individual patients. The researchers found the most effective weight-loss agents were phentermine/topiramate (Qsymia), followed by liraglutide (Saxenda),and orlistat (Alli).
"Both at the local and national level, we found obesity pharmacotherapy is effective in changing the trajectory of weight in Veterans in addition to lifestyle changes, said Aleman.
The study examined data for 43 local Veterans who were enrolled in the NY-MOVE! weight-loss program and who were prescribed an obesity medication. The most commonly prescribed medications at the local level were metformin (Glucophage), liraglutide, and phentermine/topiramate.
MVP study offers new insights on genetic risk for non-alcoholic fatty liver disease

Lab studies seek hormone-based obesity treatment

One-two punch helps Veterans with weight loss
The research team wanted to know how well the local group of Veterans were doing in comparison to the larger VA population. Aleman's team reviewed nearly 578,000 VA health records nationwide for Veterans who had an obesity diagnosis or metformin prescription in their VA health record. Metformin is a commonly prescribed diabetes drug that can help with weight loss.
In comparison to the New York group, the national group of Veterans had greater numbers of men, were less racially diverse, and were later in their disease progression—86% had type 2 diabetes, compared with 44% of the local group.
On average the New York group lost 8.8 pounds over the initial six-month period. Over a one-year period, 75% of the national group lost between 5.5 to 11 pounds after starting weight-loss medication.
Diet and exercise are typically first-line treatments for weight loss. In the case of Veterans, Aleman says excess weight may be related to the lack of structure they encounter after their military service is over. That is why the VA-MOVE! Weight Management Program is designed to reintroduce structure for Veterans.
VA-MOVE! makes use of behavioral interventions, like group counseling, with lifestyle guidance and nutritional education. The program offers Veterans a range of tools—for example, food journals, a mobile app to track diet and exercise, and, in some cases, access to gyms.
Studies have shown that participants in VA-MOVE! typically achieve modest, short-term weight loss—with an average of 0.28 lbs. to 7.3 lbs. at the one-year mark. Aleman says a typical weight-loss goal might be losing 5% of your baseline weight within 3 to 6 months. For a 200-pound Veteran, that would be 10 pounds.
"I tell my Veteran patients that even though it doesn't sound like a large amount of weight, it is the type of weight loss that tends to be sustainable. It will also help with health complications, which is really the goal."
The NY-MOVE! weight management clinic uses a team-centered approach to care that includes access to psychologists, nutritionists, and physicians who are trained in obesity medicine and endocrinology. The clinic provides individual or group counseling and weight-centered management of type 2 diabetes.
Many years ago it became clear to scientists that weight-loss therapies that used only lifestyle interventions—like diet and exercise—would not work for everyone. That's where medications and surgery come in.
Weight-loss medications work by decreasing appetite or increasing a feeling of fullness in the stomach. They can also interfere with fat absorption. Surgical options to induce weight loss include gastric banding, gastric sleeve, or gastric bypass procedure, among others.
If Veterans do not achieve clinically significant weight loss, the VA/DOD clinical practice guidelines on overweight and obesity recommend the addition of pharmacotherapy (medication) or bariatric surgery. However, there is little guidance in terms of the order in which agents should be used or for which populations.
When indicated, clinicians at NY-Harbor VA prescribe weight-loss medications or surgery for their patients. They also proactively treat conditions that may affect weight gain, like diabetes or prediabetes—a slightly elevated blood sugar level. People who have prediabetes are at greater risk of developing heart disease or type 2 diabetes.
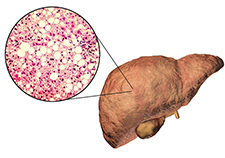
Having obesity puts people at risk for developing a number of diseases, including type 2 diabetes. Diabetes is a disease in which the body does not produce enough insulin, or the insulin it makes can't effectively remove excess sugar from the blood. Aleman says it makes sense to treat obesity and diabetes at the same time.
"If the patient has evidence of elevated blood sugar because of their weight, we tend to favor agents that do not cause weight gain, but might encourage weight loss," he says. "We gather a somewhat extensive patient history and use that to decide which medication is right for each patient."
As a group, Veterans are at greater risk of being overweight than the general population. Nearly 80% of Veterans in the VA health system had overweight or obesity in 2014. That puts them at danger for metabolic diseases like type 2 diabetes, certain types of cancer, and heart disease.
The VA-MOVE! Weight Management Program helps Veterans make healthy changes in eating, physical activity, and behavior. There are several key strategies that can help manage weight loss:
In VA-MOVE!, Veterans learn skills like planning and preparing, problem solving, and stress management. Most people who commit to VA-MOVE! can reach a healthier weight, feel better, have more energy, and reduce health problems.
(From the VA-MOVE! Weight Management Program, Workbook for Veterans, Module 1)
VA Research Currents archives || Sign up for VA Research updates