Office of Research & Development |
 |
Office of Research & Development |
 |


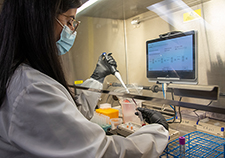
Brian Strzelecki, a research engineer and 3D printing specialist at VA Puget Sound, co-authored the VA study that evaluated how well the 3D masks perform.
May 27, 2021
By Mike Richman
VA Research Communications
"Instead of relying strictly on purchasing off-the-shelf masks during a crisis situation, which everybody's trying to do, VA is working to create its own mask in order to build redundancy into the hospital supply chain."
The COVID-19 pandemic has caused a high demand for respiratory protection among health care workers in hospitals, especially surgical N95 face masks—cup-shaped respirators that guard against airborne particles and liquid contaminants.
In response, VA researchers are experimenting with 3D-printed masks as a substitute for N95s and other respiratory devices.
A newly published study evaluated how well the 3D masks perform, with a focus on the filter materials used to block out airborne particles and liquid contaminants. The project team found a wide range of filter efficiency in the 3D masks, including some filters that met or closely approached the criteria needed to make a typical N95. Others did not filter nearly as well when matched up against the N95.

The researchers found a range of filter efficiency in the 3D masks, such as this one, including some that met or closely approached the criteria needed to make an N95. (Photo by Janet Busey)
The findings appeared online in May 2021 in the Journal of Occupation and Environmental Hygiene.
Dr. Jack Stapleton, an infectious disease specialist at the Iowa City VA Health Care System, served as the study’s principal investigator. He’s also a professor at the University of Iowa, where researchers carried out the lab testing for the study.
The filter materials that met the filter efficiency and breathing resistance criteria of an N95 mask can potentially be used with 3D masks in the future, Stapleton says. But as more people are vaccinated to protect themselves from the virus, and the normal supply chain of N95s stabilizes, he hopes the use of 3D masks will be a less pressing issue.
“However, in the event of a new respiratory pathogen or a shortage of personal protective equipment, this research provides evidence to support use of 3D-printed masks with specific filters,” Stapleton says.
Along with Drs. Peter Thorne and Patrick O’Shaughnessy, VA engineers who are affiliated with the University of Iowa College of Public Health, Stapleton also studied the best method of filter disinfection.
“We had promising results in that we showed you can reuse materials that are disinfected by heat and still retain filtering function,” he says. “But the most common method used to disinfect filter materials, hydrogen peroxide, was not as effective. Hydrogen peroxide disinfection reduced the efficiency of the filter materials tested so they didn’t meet the N95 criteria. In addition, the small filter area in the 3D-printed masks led to problems with breathing resistance,” or difficulty breathing.

AI to Maximize Treatment for Veterans with Head and Neck Cancer

VA researcher works to improve antibiotic prescribing for Veterans
VA’s Million Veteran Program played crucial role in nation’s response to COVID-19 pandemic
VA Further Develops Its Central Biorepository: VA SHIELD
Currently, 3D-printed masks do not exist on the market. But VA is creating its own supply through a new program spawned by the VHA Innovation Ecosystem. The program involves the VA Puget Sound Health Care System in Washington state; the Ralph H. Johnson VA Medical Center in Charleston, South Carolina; and the Hunter Holmes McGuire VA Medical Center in Richmond, Virginia. All three facilities have 3D-printing capability and are leading efforts to develop new clinical innovations that leverage the technology.
“Instead of relying strictly on purchasing off-the-shelf masks during a crisis situation, which everybody’s trying to do, VA is working to create its own mask in order to build redundancy into the hospital supply chain,” says a co-author of the study, Brian Strzelecki, a research engineer and 3D printing specialist at VA Puget Sound. “We’re exploring a new concept of a reusable mask design that VA can potentially make for itself and that can act as a supplemental personal protective device when traditional models can’t be acquired.”
Work by Strzelecki and other engineers at VA Puget Sound prompted the study. They developed a reusable mask with a 3D-printed hard, plastic frame and desired to test different filter materials, which sit in a box in front of the frame. Seeking assistance, they contacted Stapleton and his University of Iowa colleagues, who aimed to learn which filter materials would work in a 3D mask in place of N95 respirators and facemasks that surgeons wear in the operating room. Commercial vendors supplied the filters tested in the study.
In the 3D mask design, the engineers used 25% of an existing surgical mask for filter patch material. They tried to take that design to the next level by finding a filter material that would be on par with an N95, not only a surgical mask. “Because of that, we held the original filter patch dimensions constant trying to find a material that would work to get the design equivalent to an N95,” Strzelecki says.
The N95s do not use replaceable filters. The mask itself filters out most of the contaminants. In addition, the N95 mask isn’t made of a hard, 3D-printed material, so the design is different from the mask created by Strzelecki and his team.
The researchers evaluated 14 types of filters and eight combinations for filtration efficiency, liquid penetration, and breathing resistance, in accordance with standards of the National Institute for Occupational Safety and Health (NIOSH). NIOSH approves cup-shaped filtering facepiece respirators and gives them the designation N95.
Some filter materials in individual layers and one combination met the filter efficiency and breathing resistance criteria of an N95 mask when tested at the NIOSH air flow rate (85 liters per minute). “These media and the combination could therefore serve as the raw material in the fabrication of a cup-like N95 when shortages occur, as has [happened] during the current COVID-19 pandemic,” the researchers write. “The 3D-printed mask holds promise as an easily fabricated alternative to a standard N95.”
Achieving the right breathing resistance, Strzelecki explained, is like a balancing act. “The mechanics of filtration indicate that when you increase the protective layers, chances are the filtration efficiency goes up,” he says. “You can add a bunch of layers of filtration to the point where you’re filtering out all of the bad stuff, but as a result a very small percentage of air is reaching the user. That makes it hard to breathe properly. Finding the proper filter material is the balance of having the material thin enough so enough air passes through to the user, but it still captures all of the virus particulate before it reaches the user.”
Stapleton and his colleagues performed additional testing to assess two filter disinfection methods—dry heat and vaporized hydrogen peroxide—that would enable reuse of the filter patch in a hospital setting, instead of having to swap it out after each use. The dry heat disinfected the filters with no drop in filtration efficiency. But the hydrogen peroxide reduced filtration efficiency by an average of 13% and increased breathing resistance four-fold due to the smaller filter space in the 3D mask, compared to that of an N95.
A 2020 study by the same research team showed that dry heat seems to be a more viable decontamination method than hydrogen peroxide for the filter material.
Strzelecki considers the latest study a success, in terms of what the researchers aimed to discover.
“At the very least, we were able to determine which industrial filter materials were not even close to being a viable candidate in a clinical setting,” he says. “Before, it was a daunting task trying to start this process because there are so many potential facemask options commonly used in industrial applications that theoretically may be able to work in a clinical setting.
“We collected a lot of good data,” he adds. “This is going to be a great springboard to drive a lot of different future designs of reusable 3D-printed masks. The current design needs to be refined a little further, and some minor improvements need to be made before we go all the way to the official NIOSH testing and get the required stamp of approval.”
VA Research Currents archives || Sign up for VA Research updates