Office of Research & Development |
 |
Office of Research & Development |
 |


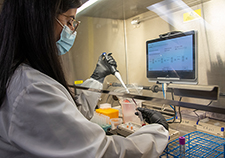
Karen Curtis, with Environmental Services at the Baltimore VA Medical Center, cleans a patient room in the hospital’s intensive care unit. (Photo by Mitch Mirkin)
April 8, 2020
Erica Sprey
VA Research Communications
VA anthropologist Dr. Jennifer Van Tiem says she often spends part of her day just "hanging out."
While you might guess that she is talking about hanging out with friends, she actually means observing and talking with the people around her and taking field notes for research.
Van Tiem is a VA researcher working for the Health Services Research and Development Center for Access and Delivery Research and Evaluation (CADRE) at the Iowa City VA Health Care System.
She and her coauthors recently published a paper in the American Journal of Infection Control that highlighted the importance of asking environmental service workers for their perspectives on infection control in community living centers.
"The ability to...hold an awareness of the whole facility might be...crucial to connecting and balancing the social and clinical aspects of care when developing infection control policies. "
The researchers interviewed 40 staff members at five different VA community living centers across the U.S. Staff roles included: epidemiologists, infectious disease specialists, nurse managers, nursing assistants, and environmental service workers, sometimes referred to as housekeeping staff.
Their aim was to assess staff members' knowledge, attitudes, and beliefs concerning infection prevention and resident-centered care in community living centers.
Veterans who live in long-term care facilities are at high risk of developing a drug resistant infection, such as methicillin-resistant Staphylococcus aureus or MRSA. Infection prevention practices designed to combat infections like MRSA were first developed for patients in acute care settings like hospital ICUs. However, these practices are more difficult to implement in long-term care facilities, where staff strive to create a home-like setting for residents.
The researchers found that staff felt challenged by the need to maintain effective infection control while still providing a home-like environment for residents that facilitated social interactions. They also found that environmental service workers had a unique way of thinking about infection control that typically was not considered by their team members.
"Our findings suggest that infection control team members may find environmental service workers to be natural, untapped allies in identifying opportunities to improve infection control policies in community living centers," wrote the study authors.

AI to Maximize Treatment for Veterans with Head and Neck Cancer

VA researcher works to improve antibiotic prescribing for Veterans
VA’s Million Veteran Program played crucial role in nation’s response to COVID-19 pandemic
VA Further Develops Its Central Biorepository: VA SHIELD
VA community living centers serve the dual purpose of providing a home for older Veterans who need assistance with activities of daily living and providing skilled nursing care.
Unlike an acute care setting in a hospital, Veterans' rooms are not just where they receive care. They are also a personal space that contains pictures, mementos, and other important belongings. Veterans spend time with friends in their rooms, and often share a bathroom with another resident.
In a community living center, unlike an inpatient setting, Veterans are encouraged to move more freely around their environment. They frequently visit friends, talk to nurses at the front desk, and take their meals in a shared dining room. Social interactions like these are an important component of Veterans' care.
However, this freedom of movement can complicate infection prevention. Rather than focus solely on the bedroom, environmental service workers must expand their efforts to surfaces throughout the facility. That means, for example, knowing to clean the corners in residents’ rooms, as well as the railings in hallways and front-desk countertops.
"Acute care practices like bathing, wound care, and room cleaning, occur in the residents' rooms," says Van Tiem. "But the social aspects of care occur in communal dining spaces, hallways, and the nurses' stations. Balancing these two paradigms of care means that infection prevention is, in the words of a nurse who participated in the study, 'like a puzzle that we keep solving every day.'"
The ideals that drive the community living center are a homelike setting, social integration, and mobility, says Van Tiem. In contrast, the ideals that drive infection prevention are cleanliness, sterility, and contact precautions or enhanced barrier precautions. Van Tiem notes that it's been very difficult for staff to know how to balance those two goals.
Busy health care staff typically focus their energies on patient care, in order to maintain efficiency and quality of care. In a community living center, that means nurses are focused on patient care tasks that take place in Veterans' rooms, like wound care, bathing, and drawing blood.
Environmental service workers aren’t considered part of the clinical care team, yet they play a critical role in infection prevention. Van Tiem says she thinks of them as geographers, navigating daily the many different spaces and domains that encompass the community living center.
According to Van Tiem, one of the things that became clear from talking with environmental service workers, was the idea of a "therapeutic space." Therapeutic spaces are another way to talk about the social aspects of patient care, she says. Thinking in in this way can help staff understand how the location of the nurses' station might encourage residents to gather, or how residents' living habits and daily schedules make it necessary to negotiate when to clean rooms.
Environmental service workers' aptitude for thinking globally is just what community living centers need, in terms of infection control practices, Van Tiem suggests.
"The ability to notice corners and hold an awareness of the whole facility might be like a keystone—crucial to connecting and balancing the social and clinical aspects of care when developing infection control policies."

Drug-resistant bacteria have been a major problem for hospitals and long-term care facilities worldwide. (Photo: ©iStock/SrdjanPav)
Hospital-acquired infections are a significant concern for health care facilities. So is the growing problem of drug resistant organisms like vancomycin-resistant enterococci (VRE) and methicillin-resistant Staphylococcus aureus (MRSA). These organisms are referred to as multidrug resistant organisms, or MDROs.
Risk factors that make it more likely a person will get a MDRO include a weakened immune system, chronic illness, and indwelling medical devices like a urinary catheter. Residents in community living centers are also at high risk of developing an infection from a MDRO.
In 2007, VA instituted a "MRSA bundle" in its acute-care hospitals to combat health-care-associated infections like MRSA. In 2009, the MRSA Prevention Initiative was implemented in VA long-term care facilities. The bundle has four components that are used to treat patients who have a MDRO:
Following implementation of the MRSA bundle, rates of health care-associated MRSA infections in VA hospitals declined by 62% over two and a half years, according to a study in the New England Journal of Medicine.
One important component of the MRSA bundle is the use of PPE for health care staff, which includes gloves, gowns, and masks. Different types of health care facilities may recommend varying degrees of PPE use.
"Contact precautions" means that hospital staff should wear PPE for any contact with infectious patients. "Enhanced barrier precautions" loosen those restrictions slightly, directing staff to wear PPE if they anticipate touching a resident or contaminated surface.
In 2013, VA changed its MRSA guidelines, replacing the mandate for contact precautions with enhanced barrier precautions. Using enhanced barrier precautions is a way of protecting a nurse's non-clinical relationships with her patients. In practice, that means a nurse would not don PPE if she were just coming into a patient's room to check on them or tell them something, says VA researcher Dr. Jennifer Van Tiem.
Using isolation precautions to care for residents who have a MDRO could have the unintended effect of making Veterans feel stigmatized and increase their risk of depression and anxiety.
Dr. Daniel Morgan is an epidemiologist at the VA Maryland Health Care System in Baltimore. He was principal investigator on a two-part study that examined the effectiveness of MRSA isolation policies in 133 VA community living centers. (Van Tiem's research on infection control practices in community living centers was derived from part two of Morgan's study.)
The study was part of a larger VA Collaborative Research to Enhance and Advance Research Excellence (CREATE) on MRSA infection prevention strategies.
The team analyzed data from 226,000 admissions to VA long-term care facilities, looking at MRSA infection rates. They also reviewed infection prevention policies at 74 facilities to determine if isolation practices were used for residents with MRSA. Overall, MRSA infections declined by 30% during the observation period. The team found no difference in MRSA infection rates for varying isolation use.
VA Research Currents archives || Sign up for VA Research updates