Office of Research & Development |
 |

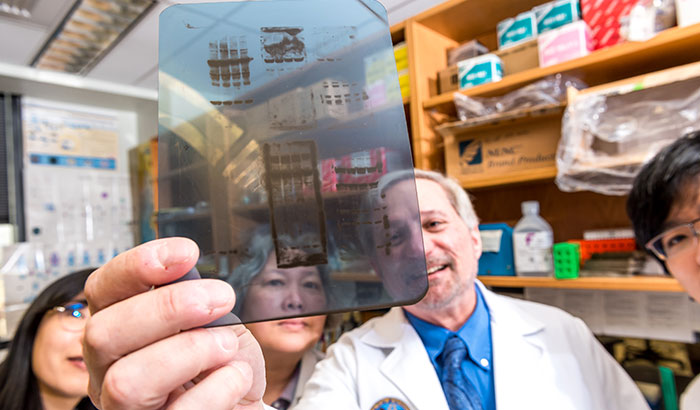
The lab of Dr. W. Timothy Garvey (holding slide) in Birmingham is one of the nation's leading sites for diabetes research. (Photo by Joe De Sciose)
April 4, 2018
By Mitch Mirkin
VA Research Communications

Dr. W. Timothy Garvey talks with Birmingham VA patient James “Lester” Hallman. (Photo by Joe De Sciose)
There is a relative flood of diabetes medications available today. The Food and Drug Administration website lists more than 50 different brand names approved to treat type 1 or type 2 diabetes. Almost half were approved only in the past five or so years.
But even with all these drug options, many of them incorporating the latest research and newest technologies, there’s still not a single one that halts the progression of the disease over several years, according to Dr. W. Timothy Garvey. That’s a holy grail for his group and other diabetes researchers, he says.
Garvey is an investigator and staff physician at the Geriatric Research, Education, and Clinical Center at the Birmingham VA Medical Center, and director of the Diabetes Research Center at the University of Alabama at Birmingham. He’s also the Butterworth Professor and Chair of the Department of Nutrition Sciences at the school.
"It's rewarding to work with [Veterans] and try to do research that has the potential to benefit them."
“We don’t have medicines that freeze the glycemic control right where it is, over a longer period of time,” says Garvey. “With any medicines we have, there’s ongoing deterioration, and a need to add new medicines, and eventually go to insulin. So we need medicines that stabilize the disease and prevent metabolic deterioration over time.”
Garvey hopes his lab can help discover just such a drug. Among the projects his team is pursuing is a VA-funded study of a gene called TRIB3. Based on research the team has done so far, the gene appears to drive the vicious cycle known as glucose toxicity, or in scientific terms, glucose-induced insulin resistance.
Beta cells within the pancreas produce insulin. The hormone allows the body’s cells to take up glucose from the bloodstream. But in type 2 diabetes, cells become resistant to the insulin. They thus become unable to absorb glucose, and it remains circulating in the blood at higher-than-normal levels. That in turn worsens insulin resistance. The beta cells eventually wear out from trying to pump out enough insulin. The resulting drop in insulin production further worsens the blood sugar crisis.
Some diabetes drugs, such as metformin, hold back the tide of insulin resistance; they make cells more sensitive to insulin, so they respond to the hormone and remain able to properly take in sugar from the blood.
But, as Garvey points out, these drugs tend to lose their effectiveness over time. Diabetes control worsens. That means glucose levels rise higher, beta cells break down, and insulin resistance increases. “In other words,” says Garvey, “poor control of diabetes begets worse diabetes.”
Garvey explains where TRIB3 comes in, potentially as part of the solution:
“In a patient with diabetes, when glucose is elevated, that hits all the tissues, causes abnormalities, and makes insulin resistance worse. We found that TRIB3 is the key operator there. The glucose increases expression of that gene, and that gene then impairs insulin signaling and causes [or worsens] insulin resistance.”
He continues: “If we could prevent glucose toxicity—that is, high glucose’s ability to wear out the beta cells and impair insulin secretion—that’s what we need to ‘freeze’ diabetes and keep it from getting worse. Drugs that could block either the induction of TRIB3, or its biological effects after it’s induced, have that potential. They would prevent glucose toxicity.”
What makes Garvey’s team unusual is their wide, full-spectrum approach. They do lab studies in cultured cells and genetically engineered mice, trying to gain new insight into the biochemical pathways of insulin resistance. But they also take biopsies of muscle and fat tissue from study volunteers at the Birmingham VA and UAB Hospital, to be metabolically characterized in the lab, and run blood sugar, triglyceride and other medical tests on those same patients. Some of the patients have diabetes, others don’t. Some are pre-diabetic, and some are perfectly healthy with regard to blood sugar. That way, the lab can run chemical tests on the tissues and cells and search for differences in levels of proteins and other molecules.

Veteran disability payments led to fewer hospitalizations
Study links statin use with diabetes progression, points to need for further research
Can statins help 75-and-overs stay healthy? PREVENTABLE trial will provide answers
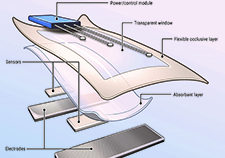
VA researcher develops 'smart bandage' technology for chronic wounds
“We’ll analyze gene expression, and then protein function from those tissues,” explains Garvey. “Then we can correlate those measurements with our in vivo [in the body] measurements of whole-body metabolism to get an idea of the degree to which those abnormalities contribute to disease.”
Garvey says that’s how his group uncovered the role of TRIB3 in the first place.
“We saw that the level [of TRIB3] in muscle tissue was correlated with how high the glucose was in patients. If [the level of gene expression] was low, the glucose was low. If it was high, the glucose was high. So that’s how we thought it might be a glucose-inducible gene.”
The next step was seeing if adding glucose to cells in Petri dishes caused TRIB3 to spike. It did. And not surprisingly, those same cells became insulin-resistant.
The team then looked at the phenomenon in mice.
“When we hyper-expressed [the gene] or knocked it out in transgenic mice, we found that the gene really did play a role in glucose-induced insulin resistance in an intact organism.”
Garvey hopes his lab’s ongoing work with TRIB3 will eventually lead to a new compound capable of stopping diabetes in its tracks. He notes that along with new drugs, lifestyle interventions—namely, diet and exercise—are critical to keep weight in check and improve other health parameters. He adds that for some patients, weight-loss surgery is a valuable treatment. “I think bringing the principles of obesity medicine into the diabetes clinic and using weight loss as a therapeutic approach in type 2 diabetes holds a lot of promise,” he says.
Among other accomplishments, Garvey’s lab, which began its work in the late 1980s, has been credited with several key publications that advanced scientific understanding of the role of insulin resistance in metabolic syndrome. One area of focus for the lab was GLUT4 transporter proteins, which ferry glucose into cells.
In patients with diabetes, says Garvey, “we were able to show defects in how well those proteins move around in the cell and respond to insulin, how easily they can get out to the cell surface, where they can really bring the glucose in. Through our VA-funded research, we described defects within that trafficking in the cell.”
All along, Veterans have played a major role in the research.
“It’s such a pleasure to work with Veterans,” says Garvey. “They’re such good people, and they’re willing to consent to research and try to be helpful. It’s rewarding to work with them and try to do research that has the potential to benefit them.”
VA Research Currents archives || Sign up for VA Research updates