Office of Research & Development |
 |

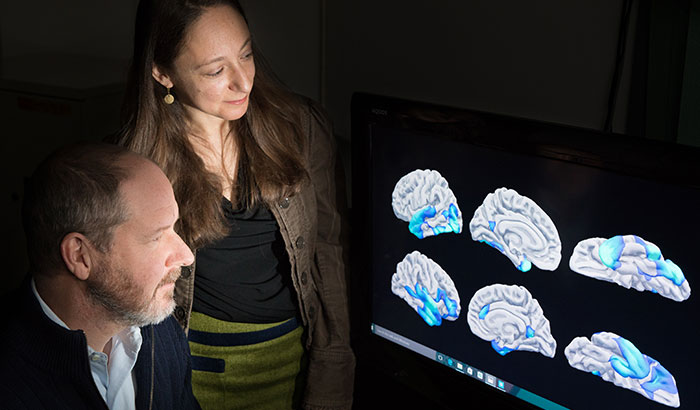
Drs. Mark Miller and Erika Wolf are with VA’s National Center for PTSD. (Photo by Derrick Morin)
January 16, 2018
By Mike Richman
VA Research Communications
"We have examined the extent to which a person’s DNA methylation age is greater than or less than their chronological age."
Evidence is growing in the scientific community that people with PTSD are aging at an abnormal pace. The link between the two is a hot topic, as is the connection between other forms of psychological and environmental stress and accelerated aging.
Two Boston-based clinical research psychologists with VA’s National Center for PTSD—Dr. Mark Miller and Dr. Erika Wolf—are at the forefront in dissecting the nexus between PTSD and accelerated aging.
They are examining the theory that the stress of PTSD and its other symptoms speed up the aging process, with biological age exceeding chronological age. They and other researchers surmise that this phenomenon could lead to an early onset of age-related diseases, such as dementia and chronic pain, and even premature death.

VA Researcher Named One of U.S.’ Top Female Scientists

Million Veteran Program director speaks at international forum
2023 VA Women's Health Research Conference

Self-harm is underrecognized in Gulf War Veterans
The key question Miller and Wolf are trying to answer is what traumatic stress does to make someone age at a rate faster than normal.
“Everyone wants to know how traumatic stress `gets under the skin,’ ” Wolf says. “My view is that psychiatric symptoms are paired with biological reactions that are manageable in the acute phase but become problematic when they occur chronically. These include inter-related processes, such as increased heart rate, inflammation in the brain, and oxidative stress, as well as decreased immune system functioning, abnormal stress reactivity, and metabolic irregularities that disrupt basic bodily functions.”
Oxidative stress is tissue damage resulting from an excessive amount of pro-oxidants and an insufficient level of antioxidants.
“Collectively, these problems take a toll on the body via cellular aging and reduced blood brain barrier functioning, as well as other processes,” Wolf says. “In addition, behaviors such as smoking, substance use, and poor sleep, nutrition, and exercise contribute to some of the same biological problems. My hope is if we can identify this process early on and see who is at risk for which negative outcomes, we can prevent or delay the risk of disease by matching treatments to the person.”
Wolf and Miller, who are also affiliated with the Boston University School of Medicine, have been pursuing this line of research for several years.
Initially, the duo conducted studies that showed major links between Veterans with PTSD and accelerated aging. Some of the former service members were in their early 30s, suggesting that relatively young Vets with PTSD have the potential to age fast and develop age-related health conditions.
“The idea that traumatic events can have a physical effect on people has been around for a long time,” Miller says. “Observations suggest that traumatic stress starts a cascade of biological consequences that can produce visible signs of aging. [Further] research shows how this is happening on a cellular level, and for the first time we have the methods to actually see it in a person’s DNA.”
As they examine accelerated aging in relation to PTSD, Miller and Wolf have come to focus on an index of biological or cellular age referred to as DNA methylation (DNAm) age. Methylation is one of the main ways the body switches genes on and off, and certain patterns of DNA methylation change normally with a person’s age.
Investigators have developed calculations for predicting cellular age from DNA methylation data. Some researchers have linked abnormal DNA methylation to adverse outcomes, including human diseases.
Miller and Wolf are taking it a step further by researching PTSD in relation to abnormalities in DNA methylation age.
“We have examined the extent to which a person’s DNA methylation age is greater than or less than their chronological age,” Wolf says. “We have shown in analyses focused on Veterans that PTSD was linked to accelerated methylation age. We also showed that Veterans with accelerated DNA methylation age were more likely to display subtle signs of neurodegeneration in a region of the brain important for transmitting information across the cerebral cortex—and that they were more likely to die prematurely.”
The cerebral cortex plays a vital role in memory, attention, cognition, awareness, language, and consciousness.
In a study published in July 2017 in the journal Psychosomatic Medicine, Wolf and colleagues evaluated ties between trauma exposure, PTSD symptoms, and accelerated versus decelerated DNAm aging in 241 trauma-exposed Veterans. The team also examined if accelerated DNA methylation age predicted death over the course of a 6.5-year medical review period.
The researchers found that PTSD hyperarousal symptoms were linked to accelerated DNAm age, but that trauma exposure and PTSD severity were not. Accelerated DNA methylation age was associated with a 13 percent increased risk of death during the medical review period.
The findings suggested that the association between PTSD and accelerated DNAm age may be related to the hyperarousal symptom cluster, which includes difficulty sleeping and outbursts of anger.
Wolf says Veterans should care about accelerated DNA methylation age to the extent that it “represents an early sign of the subsequent development of clinical health conditions, such as metabolic syndrome.” The latter is a group of conditions, including increased blood pressure, high blood sugar, excess body fat, and abnormal cholesterol, that occur together and can raise the risk of heart disease, stroke, and diabetes.
At the same time, she stresses it’s too early to use DNA methylation age as a clinical tool.
“However, if the research continues to support its use, we could envision a day in which DNA methylation age is assessed and tracked over time to examine the impact of intervention efforts on cellular age at an individual level,” she says. “More directly, our work on metabolic syndrome suggests that PTSD may be viewed as a risk factor for cardiometabolic disorders, such that Veterans with PTSD might need screening for cardiometabolic problems a decade earlier than current recommendations.”
She adds: “In many instances, if a person does not have a family history of heart disease, then screening might not occur until about age 40. But our data have demonstrated that there were metabolic aberrations in Veterans with PTSD who are in their early 30s. We need to make sure that group is being found and followed early on.”
To gain a clearer picture of whether PTSD and other psychiatric symptoms accelerate DNA methylation age, Wolf and Miller are pursuing longitudinal studies that span more than a decade. They are also looking at other biological signs of cellular aging, such as inflammation in the brain, immune response, and telomere length. Telomeres are an essential part of human cells that affect how they age.
The Wolf-Miller tandem is also interested in studying how reductions in inflammation and oxidative stress may be tied to improving the pace of cellular aging.
Case in point: Miller led a study, published in January 2018 in the journal Brain, Behavior, and Immunity, that examines factors that influence the blood levels of C-reactive protein (CRP) in people with PTSD. Little is known about those factors.
CRP is a popular measure of peripheral brain inflammation, which has been associated with impairments in cognitive function.
Nearly 300 post-9-11 Veterans, over half of whom had PTSD, participated in the study. The researchers found that the Veterans with PTSD were more likely to have CRP levels in the clinically elevated range than those without PTSD.
The findings “provide new insights into genetic and epigenetic mechanisms of inflammatory processes in the pathophysiology of PTSD and point to new directions for biomarker identification and treatment development for patients with PTSD,” Miller, Wolf, and their colleagues wrote.
According to Miller, research is underway that could provide important insights into the location of inflammatory markers and oxidative damage in the brain.
He notes that scientists are pursuing DNA methylation and gene expression studies using brains that were donated to VA’s National PTSD Brank Bank, a brain tissue biorepository that supports research on the causes, progression, and treatment of PTSD. The bank is part of a consortium led by VA’s National Center for PTSD.
So what are the possibilities for stemming the development of PTSD-related accelerated aging? Wolf defines this as “uncharted territory.”
“But it’s an important direction to pursue,” she says. “We don’t yet know if accelerated aging can be weakened or reversed in response to a pharmacological or behavioral intervention. Given some evidence that obesity is associated with accelerated aging, it would be reasonable to assume that behavioral factors such as stress reduction, exercise, and getting good sleep and nutrition have the potential to be helpful in this regard.”
VA Research Currents archives || Sign up for VA Research updates