Office of Research & Development |
 |

VA Research Currents archive
December 10, 2015
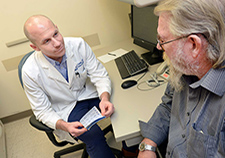
Dr. Matthew Crowley meets with diabetes patient Jon Morris at the Durham VA. Crowley's team is studying how to use telehealth to boost care for Veterans with diabetes whose condition has not responded to standard clinic-based care. (Photo by Linnie Skidmore)
A new telehealth program developed at the Durham VA Medical Center may be sweet news for Veterans whose diabetes has not responded to standard care.
The program is called ACDC—short for Advanced Comprehensive Diabetes Care. Tested in a pilot study of 50 Veterans with persistently poor diabetes control, the approach beat standard clinic-based care for nudging blood sugar levels toward normal. The pilot study results went online Nov. 5, 2015, in the journal Telemedicine and e-Health.
Half the Veterans in the study got "usual care," without any special interventions. They also got an education packet.
The other half took part in the telehealth program. It combined four key elements:
Lead researcher Dr. Matthew J. Crowley and colleagues write that these four elements work together to "target factors underlying persistent poorly controlled diabetes."
Moreover, they say that because the ACDC program doesn't require staffing or equipment beyond what VA medical centers already have in place, it can potentially be scaled up nationwide.
Crowley noted in an interview that "VA is way ahead of the curve in developing telemedicine infrastructure, and we specifically designed this approach to take advantage of that fact for those Vets most in need."
The researchers compared several outcomes across the two study groups. The main measure was HbA1c, which shows average blood sugar levels over the past two to three months.
After six months, the usual-care group showed a slight reduction: from 10.5 to 10.2. The drop was sharper in the ACDC group: 10.5 to 9.2. That may not sound like a lot, but the researchers say that over time such an improvement in blood sugar could significantly cut the risk of heart attack or other complications, and death.
"You need to consider the population we're working with—these are patients for whom nothing else has worked. A 1 percent change is actually a pretty big deal in this population," says Crowley.
The reduction in blood sugar, not surprisingly, was greater for those ACDC participants who took part in more phone encounters. For patients who completed more than 6 of the scheduled 12 encounters, the average A1c improvement was nearly 2 percent.

Veterans with poor diabetes control who took part in a Durham VA telehealth study were helped to become more regular in checking their blood sugar, among other improvements. Regular checking helps patients understand how their sugar is affected by eating, exercise, and stress, and helps improve care planning. (Photo: ©iStock/Fertnig)
The ACDC group, but not the usual-care group, had lower blood pressure after six months. They also did better on an overall measure of diabetes self-care, although their self-reported medication adherence remained the same as that of the usual-care group.
The groups also remained about equal with regards to depression symptoms. But most of the ACDC group already had psychiatry care in place, so the study intervention may have added little to their care in this area.
The researchers acknowledge that intensive telehealth care doesn't suit everyone's tastes. Almost half of the patients who were approached to be in the study declined to take part.
But among those who did, most said they found the program acceptable. On a follow-up survey, most agreed that ACDC "seemed like an appropriate way to address my diabetes." Most said it fit their lifestyle, and that they were willing to continue using the skills they learned.
Now Crowley and colleagues are seeking funding to study the model across several sites, with up to 300 patients. "We want to further examine ACDC's effectiveness, feasibility, and generalizability at different VA centers," he says. "Because VA has built a unique nationwide telemedicine infrastructure, we see major potential for implementing this approach to persistent poorly controlled diabetes at centers across the country. We see the larger study as the next step toward that objective."
He says his group is also taking a closer look at what "usual care" actually looks like for those with persistent poor control of their diabetes. For example, are they typically missing scheduled appointments?
"My sense based on our prior work," says Crowley, "is that many patients with persistently poor diabetes control have very real barriers that make improvement under usual care more difficult—for example, competing demands from employment, transportation problems, and difficulty adhering to the complex self-management behaviors that diabetes requires."
Through the ACDC research, he says, "we've been able to identify and focus on a subgroup of Veterans that really needs something different than 'usual' care."