Office of Research & Development |
 |

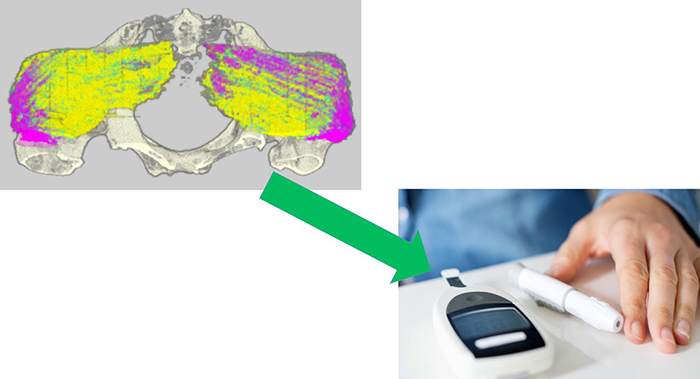
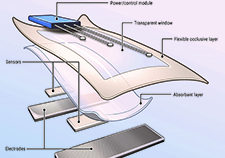
The PIPChip device is under development to identify blood-based biomarkers for pressure injury risk in people living with SCIs. (Photo courtesy Congressionally Directed Medical Research Programs and Dr. Kath Bogie.)
January 27, 2021
By Ev Chasen, contributor
VA Research Communications
"Pressure injuries are terrible wounds that particularly impact Veterans with spinal cord injuries."
In 2019, a team of researchers at VA’s Advanced Platform Technology Center (APT Center) and Case Western Reserve University (CWRU) in Cleveland found that monitoring levels of two types of proteins in the blood can help identify Veterans with spinal cord injuries who are at greater risk for developing recurrent pressure injuries. Pressure injuries, also known as pressure ulcers or bed sores, are painful wounds that can be life-threatening if they become infected.
Now, the team is developing a portable, disposable biosensor to let wheelchair users and their caregivers know if the levels of those proteins are abnormal. The device functions as an early warning system that can help prevent pressure injuries from emerging.
“Pressure injuries are terrible wounds that particularly impact Veterans with spinal cord injuries,” explains Dr. Kath L. Bogie, VA research career scientist with the APT Center and associate professor at CWRU. “We looked to see if we could figure out why some people developed these wounds, over and over again, while others didn’t.”
VA researcher develops 'smart bandage' technology for chronic wounds

Adaptive rock climbing has physical, psychological benefits for people with disabilities

3D images, algorithms are key in potential new tool for measuring bedsores in spinal cord injury

Study: Leg implants for paralysis work long-term
Bogie and her team found that the gluteus muscles of many Veterans who had recurrent pressure injuries contained high levels of fat, while that was not the case for Veterans who did not have frequent wounds. The gluteus muscles, also known as the buttocks, are the largest muscles in the human body and are the muscles on which people sit.
People with high fat levels in their glutes, the team concluded, are at higher risk of developing recurrent pressure injuries than those who did not. Determining who is at risk, however, is not a simple task, and is not related to obesity.
“Just as you can’t tell if someone has a high cholesterol level by looking at them, you can’t tell if someone has high intramuscular fat just by looking at them,” Bogie says. “In fact, some of the people with the highest fat levels in the initial study were not fat at all.”
The team identified two biomarkers in the blood samples of Veterans who had high levels of fat in their glutes. One, FABP4 (fatty acid binding protein), revealed the levels of adipose or fat tissue, and the other, FABP3, indicated the level of remaining muscle tissue. With this knowledge, the team turned to creating a useful test to quickly determine FABP4 and FABP3 levels in the blood in order to identify at-risk SCI patients.
“I talked to experts at the APT Center and Case Western—Drs. Pedram Mohseni, Michael Suster, and Umut Gurkan—to see if we could build a point-of-care technology to leverage our knowledge of what these markers are, and to do rapid testing,” Bogie recalls. Point-of-care technology allow clinicians to conduct real-time, diagnostic blood tests within minutes, instead of hours, through the use of portable analyzers.
The team is developing a portable, disposable biosensor—which they dubbed a PIPChip—to conduct the tests either by patients at home or by clinicians during regular outpatient visits. The PIPChip analyzes a drop of blood from study participants to search for indications whether they are at higher risk of developing pressure injuries.
Veterans who are at greater risk of developing pressure injuries can take steps to avoid them by making certain the wheelchair they use is the right size and the foam or gel seat cushion fits properly; shifting their weight in the chair more often; transferring themselves into and out of their chair correctly; eating a proper diet; and keeping the skin of their buttocks clean and dry.
To help ensure the PIPChip will be user-friendly, Bogie added Sean Ferry to her team. He is a Veteran consumer advocate with a spinal cord injury. “Sean will give us insight into what Veterans actually want and talk to other Veterans about what will be most useful to them,” she says.
Chief of Spinal Cord Injuries and Disorders at the Louis Stokes Cleveland VA Medical Center, Dr. MaryAnn Richmond, and assistant chief, Dr. Kristi Henzel, are also part of the research team and provide feedback on design and usability from the clinician’s perspective.
The team has received a grant for $1.07 million from the Department of Defense’s Congressionally-Directed Medical Research Program (CDMRP) Spinal Cord Injury Research Program (SCIRP) to develop the PIPChip over the next three years. The award is one of only three such awards given nationwide in fiscal year 2019. The research team will ultimately seek approval from the Food and Drug Administration in order to market the chip.
Blood samples from Veterans with SCIs who took part in the initial biomarker study will be used for initial testing of the device, and 20 more patients will validate the initial findings.
In addition to designing and developing the PIPChip biosensor, the team also hopes to prove that FABP4 and FABP3 are accurate biomarkers for the development of recurrent pressure injuries, which would benefit not only those with spinal cord injuries, but people with all kinds of injuries and illnesses requiring long periods of bed rest. They also aim to determine how often levels of intramuscular fat should be checked.
They also hope to to work with VA’s Million Veteran Program (MVP) to develop a genetic profile of people who are susceptible to changes in fat levels, a process Bogie believes is unrelated to the spinal cord injury itself.
“VA takes care of a large percentage of the spinal cord injury population in this country,” Bogie notes. “Unlike other health care systems, we take care of them for life. So we want to know what their long-term risks are and minimize them to make sure their quality of life is optimized. This study is one way we do that.”
VA Research Currents archives || Sign up for VA Research updates