Office of Research & Development |
 |

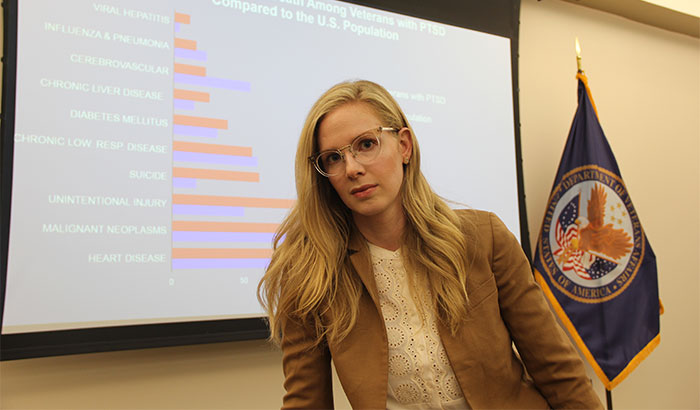
Dr. Jenna Forehand, a research fellow at the White River Junction VA Medical Center in Vermont, led a study on rates and causes of death among Veterans with PTSD. (Photo by Katherine Tang)
July 10, 2019
By Mike Richman
VA Research Communications
"These findings suggest that behavioral factors may contribute to the excess mortality risk."
A new study finds that Veterans who have been treated for PTSD are twice as likely as the U.S. population to die from suicide, accidental injury, and viral hepatitis, an infection that causes liver inflammation and damage.
The findings appeared online June 15, 2019, in the American Journal of Preventive Medicine.
Of the Veterans who died from accidental injury, more than half succumbed to poisoning. The researchers didn’t identify the types of poisoning that led to death.

Dr. Jay Gorman
Suicide prevention care

VA Researcher Named One of U.S.’ Top Female Scientists

Million Veteran Program director speaks at international forum

2023 VA Women's Health Research Conference

Self-harm is underrecognized in Gulf War Veterans
The investigators also concluded that Veterans with PTSD were more likely than the general population to die from diabetes and chronic liver disease. They also had slightly higher “all-cause mortality,” meaning they were more likely to die from any cause. The overall death rate in the PTSD group was 5% higher.
Dr. Jenna Forehand, a research fellow at the White River Junction VA Medical Center in Vermont, led the study. She and her team reviewed data on all Veterans who underwent PTSD treatment in the VA health care system from 2008 to 2013. That cohort included almost 500,000 former service members, more than one-third of whom served in the wars in Iraq and Afghanistan, with many experiencing combat.
In the year following PTSD diagnosis, 60% of the study population was diagnosed with depression, 39% with nicotine dependence, 23% with alcohol dependence, and 3% with opioid dependence.
Forehand wasn’t surprised that all-cause mortality was higher for Veterans with PTSD than for the general population.
“The overall results support prior literature demonstrating an association between PTSD and excess mortality, although the mortality risk among Veterans with PTSD is much smaller than in previous studies,” she says. “That difference may be attributed to our inclusion of all-era Veterans, including a large proportion of young Veterans, across a range of PTSD treatment settings. Veterans seeking treatment for PTSD may be more inclined to seek treatment for other medical conditions, thereby mitigating potential risk factors associated with mortality.”
Excess mortality is the proportion of deaths that occur beyond the regular death rate that would be predicted for a given population.
The inclusion of all-era Veterans allowed the researchers to examine causes of death among men and women of varying ages who served in different conflicts, Forehand notes.
The research team, Forehand adds, was surprised to find that Veterans with PTSD also had an elevated risk of death from accidental injury and viral hepatitis.
“These findings suggest that behavioral factors may contribute to the excess mortality risk,” she says. “We’re concerned that Veterans with PTSD are engaging in unhealthy or risky lifestyle behaviors like injection drug use that may lead to infection with viral hepatitis. Compared with the general population, treatment-seeking Veterans with PTSD, including young Veterans and women, are dying from largely preventable causes. PTSD is therefore a major public health concern and a priority for preventive health care.”
Conversely, the findings showed fewer-than-expected deaths among the Veterans with PTSD from cerebrovascular disease and malignant neoplasms, or cancer. Cerebrovascular disease causes blood vessel damage in the brain that can lead, for example, to various types of stroke or a brain aneurysm. Malignant neoplasms are tumors that tend to spread to other parts of the body.
Understanding the complex nature of PTSD is one of VA’s most pressing challenges. High percentages of Veterans who fought in Vietnam, the Gulf War, and Iraq and Afghanistan have had the mental health condition sometime in their lives.
PTSD symptoms include flashbacks, nightmares, hypervigilance, aggressive behavior, and severe anxiety. In addition to decreased quality of life, people with PTSD suffer from increased rates of cardiovascular, metabolic, and autoimmune disorders.
Research has shown that PTSD also greatly increases someone’s risk for suicidal ideation, which is the thought of taking one’s own life. But findings are mixed as to whether PTSD elevates risk for death from suicide.
Most published reports about the causes of death in Veterans with PTSD have focused on those who served in Vietnam. Research on the causes of death in other Veteran cohorts with PTSD, including those who fought Iraq and Afghanistan, has been limited, Forehand notes.
“With advances in medicine and technology, Veterans who served in recent conflicts are more likely to survive combat injuries, thereby increasing the prevalence of PTSD, pain disorder, and opioid use among survivors,” she says. “We were fortunate to have access to a contemporary, nationally representative data sample of U.S. Veterans with PTSD, including young Veterans and women. No study has investigated causes of death by age group among all-era, treatment-seeking Veterans with PTSD and compared their death rates to the U.S. general population. Understanding these causes may help pinpoint potential targets for prevention.”
The Veterans in her study were mostly white men who averaged 50 years in age. Almost all of them used VA primary care and outpatient mental health services for PTSD treatment, with nearly half visiting outpatient specialized PTSD clinics.
More than 5,000 Veterans out of the nearly 500,000 in the cohort died in the first year of VA PTSD treatment, the findings showed. The top three causes of death were heart disease, cancer, and accidental injury. The leading causes of death for young Veterans (ages 18 to 34) were accidental injury and suicide, with heart disease and cancer being the top causes of death for middle-aged Veterans (35 to 64) and those at least 65 years old. Among the Vets who died of accidental injury, the top causes were poisoning, motor vehicle traffic, and falls.
The paper had limitations, such as the fact that the study population included only Veterans.
“The Veteran population has demonstrated characteristics that make it unique from other PTSD populations,” the researchers write. “Notably, Veterans are predominantly older and male. Veterans who access the VA health care system are more likely to have poorer health, a lower [socioeconomic status], and more medical conditions than the general population. Therefore, these findings may not be generalizable to civilians with PTSD. It will be important that other studies replicate these results in non-Veteran populations and adjust for relevant factors.”
The researchers also say “treatment-seeking PTSD patients may benefit from more seamless transitions between care settings.” That means they could use, for one thing, closer monitoring after being seen by a clinician for their mental health condition, Forehand says.
“Veterans with PTSD often struggle with co-occurring medical and psychiatric illnesses and are prone to engage in unhealthy behaviors that increase their mortality risk,” she says. “When Veterans complete outpatient PTSD treatment or are discharged from residential care, it’s often difficult to monitor co-health conditions and external risk factors. For example, Veterans with PTSD and pain may be at risk for opioid use disorder. Opioids, in turn, may play a role in suicide, accidental injury, and hepatitis, especially among Veterans with PTSD ages 18 to 34. Close follow-up, cross-provider communication, and community integration may help bolster psychosocial support and bridge the gap between discharge and symptom relapse.”
Going forward, Forehand is interested in studying preventive strategies that address risk factors and co-health conditions in Veterans with PTSD.
“I would like to research whether evidence-based psychotherapy for PTSD impacts mortality outcomes in Veterans seeking treatment for PTSD,” she says. “Although the cohort [in her 2019 study] began in 2008 to account for changes in VA delivery of evidence-based PTSD care, that study was not designed to determine whether PTSD care effects mortality. Additional multi-year longitudinal cohorts are required to assess that outcome.”
VA Research Currents archives || Sign up for VA Research updates