Office of Research & Development |
 |

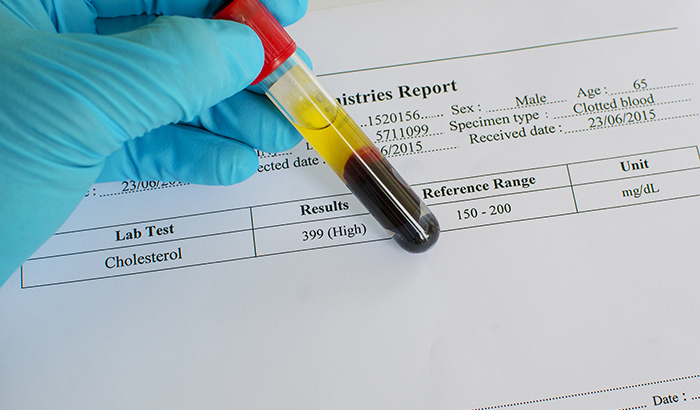
Cholesterol is key to the normal function of cell membranes. Some research, including a just-published VA study, suggests a possible link between abnormally low cholesterol and suicide risk. (Photo: ©iStock/jarun011)
June 22, 2017
By Mike Richman
VA Research Communications
"It is not clear whether an alteration in an individual's cholesterol level is sufficient in itself to alter the individual's capacity for suicide."
As a public health nurse in the New Jersey Army National Guard, Dr. Charles Reuter has seen members of the U.S. military struggling with thoughts of suicide and knows of others who have taken their own lives. The National Guard has the highest rate of suicide of any branch in the military, "which has made me even more aware of the situation," he says.
"I was and am alarmed by the rise in suicide rates in our military members and Veterans," says Reuter, also a research associate at the Coatesville Veterans Affairs Medical Center in Pennsylvania. "I wanted to try to find a way to help."
With that in mind, Reuter has added to the plethora of research examining the alarming problem of suicide in the Veteran population. Understanding that a link between cholesterol and suicide has been researched but never involving a Veteran sample, he led a study that looked into cholesterol levels as a possible marker of suicide risk among former service members. Past studies on non-Veteran populations have found that abnormally low cholesterol levels may be a biomarker of suicide risk.

Cholesterol is a substance found in most body tissues that is key to the normal function of membranes that surround cells.
Reuter's database study, published in April 2017 in Research in Nursing & Health, finds that Veterans with total cholesterol levels below 168 mg/dl (milligrams per decileter) appear to be at higher suicide risk than those with higher levels. That figure is approximately 25 to 30 mg/dl lower than what cardiology groups consider a desirable cholesterol level for adults. High cholesterol levels may put one at risk for heart disease, heart attack, or stroke.
In addition, according to the study, cholesterol levels in Veterans reporting suicide ideation, or thoughts of committing suicide, and suicide attempts were much lower than the group reporting neither. Plus, there was a notable increase in suicidality with as little as a 20 percent reduction in a Veteran's normal cholesterol level.
Despite the results, Reuter and his research team urge caution as to whether there's a definitive link between low cholesterol levels and suicide risk.
"An individual's capacity for suicide is a multifaceted component that is affected by many variables," the researchers write. "It is not clear whether an alteration in an individual's cholesterol level is sufficient in itself to alter the individual's capacity for suicide."
Reuter says, "It's important to know that I'm not saying low cholesterol will cause someone to contemplate, attempt, or commit suicide. It would be wise not to jump to any hard conclusions. Also, my findings at this point are not generalizable. I'm looking at low cholesterol as affecting somebody who is already at risk for suicide. There is a link here worthy of further research, and I am hoping that further research can contribute to a clinical decision process to help evaluate a Veteran or service member for suicide risk."
Many of the basic functions of the brain contain cholesterol. A reduction in cholesterol may alter the microviscosity, or the friction of a particle that is spreading apart, of the brain cell membrane and reduce the serotonin receptor exposure on the surface of the membrane, Reuter says. That sequence leads to a drop in serotonin uptake from the blood and less serotonin into the brain cell. The resulting imbalance between serotonin and dopamine—important chemical neurotransmitters—can increase depression and aggression, leading to suicide in certain people, he says.
Reuter designed the study to explore whether low cholesterol is linked to factors such as depression in relation to suicidality. The study included 128 Veterans who received care at the Coatesville VA. They were listed in the facility's patient record system during the period of 2009 to 2015 as having experienced suicidal ideation with evidence of escalating intent or a documented suicide attempt, or as having died by suicide.
Based on studies of non-Veterans, the researchers hypothesized that cholesterol levels below 160 mg/dl increase risk for suicide ideation or attempt. Reuter says he was not surprised that Veterans with cholesterol levels below 168 mg/dl appear to have higher suicide risk than those below 160 mg/dl. He notes that the two figures are not "drastically different."
"I say that because I would hope a Veteran who is at risk for suicide is already being cared for, treated, or on someone's radar and receiving the level of care recommended," he says. "That may be a naive statement considering the alarming rate of suicide among our Veterans, but my research is not at a stage where it can be used for a clinical decision yet. I'm hoping that as I progress with it, it will eventually be able to have clinical use."
However, Reuter wasn't expecting such a big difference with one subgroup of Vets in the study. When they were first seen at VA for a medical reason, these Veterans, part of the larger study group, had a mean cholesterol level of 210 mg/dl and didn't report suicide ideation or a suicide attempt. By way of comparison, they had a mean level of 168 mg/dl when they were seen again at a later date and did report suicide ideation or a suicide attempt. The subgroup included only 12 people, but the fact that 9 of the 12 had a major drop in cholesterol level from their first visit indicates that this finding is worth more research, he says.
His study also revealed that suicidal Veterans were younger, were thinner, were more educated, and had more anxiety and sleep problems than those being seen for an issue unrelated to suicidality.
"Research I have read indicates that this is in line with societal changes in the younger generations that have pushed people to higher education, to work more, and to sleep less," Reuter says. "This trend has led to a more stressed, anxious, and depressed group that may see suicide as a relief or end to the pain. The societal view of mental health has changed. Some also suggest that suicide does not have the stigma associated with it as it did in the past."
Reuter hopes to expand his research on potential links between cholesterol and suicide risk. Based on research he's reviewed, he also plans to consider whether to focus on low-density lipoproteins (LDL) or high-density lipoproteins (HDL), which are known as "bad cholesterol" and "good cholesterol," respectively, and whether they may impact suicide risk. Both LDL and HDL carry cholesterol to and from cells. He's also looking to measure elements of serotonin and see how they correlate to depression and suicide risk.
"I'm working on research in these areas with VA and the Army National Guard," says Reuter, who is also receiving support from Hunter College—The City University of New York, where he's an assistant professor. "My goal with this research is that it will eventually guide DoD treatment with the actively serving military, as well as treatment of the many Veterans in the VA system."
VA Research Currents archives || Sign up for VA Research updates