Office of Research & Development |
 |

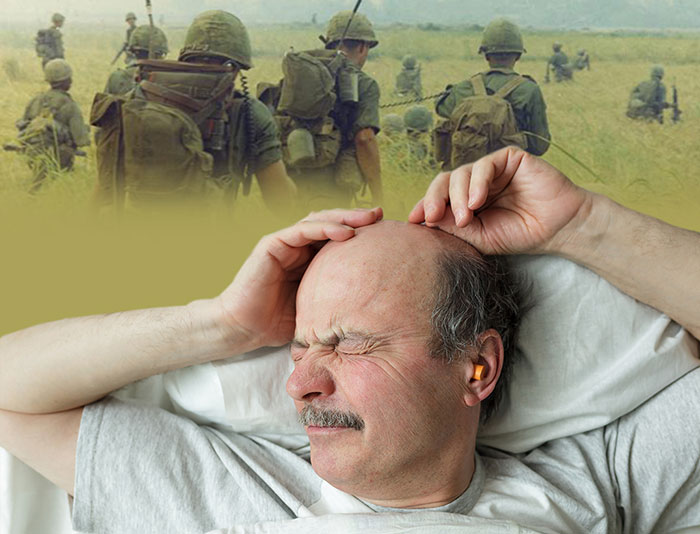
Many Veterans with combat-related PTSD experience nightmares. (Photos: ©iStock/Koldunov; National Archives)
March 13, 2019
By Mike Richman
VA Research Communications
"We recommend starting with one of the behavioral treatments when a patient has access to a qualified therapist and is willing to commit to that therapy."
The scientific community has made major strides in recent years to untangle PTSD, a mental health condition that can trigger flashbacks to a traumatic event or cause one to feel distant and angry. Advancements have been made to understand the reasons behind PTSD, where the condition takes hold in the brain, and which therapies work best.
But uncertainty exists in how to best treat nightmares, a hallmark symptom of PTSD. Research results on therapies for PTSD patients who are experiencing nightmares have been inconsistent. That shortcoming applies to Veterans, active-duty service members, and civilians, all of whom have been diagnosed with the disorder.

Dr. Ali El-Solh is a pulmonologist and sleep specialist at the VA Western New York Healthcare System in Buffalo. (Photo by Terry McGuire)
Dr. Ali El-Solh, a pulmonologist and sleep specialist at the VA Western New York Healthcare System in Buffalo, is hoping to improve the lives of Veterans with PTSD who are battling nightmares. He authored a review that explores why nightmares are a characteristic of PTSD, examines the health risks linked to PTSD and nightmares, elaborates on psychological and drug treatments for these nightmares, and identifies future research needs.
El-Solh’s review appeared online in the journal Nature and Science of Sleep in November 2018. He discussed his work with VA Research Currents.
Why is it important to highlight the connection between PTSD and nightmares?
I wrote the review largely because of the profound impact of nightmares on the quality of life of Veterans with PTSD and the inconsistent results of available treatments for this disorder. It’s of great concern that Veterans who have nightmares are at higher risk for suicide and suicidal thoughts. Understanding the origin of nightmares may offer clues in how to address the serious consequences that stem from these distressing events. But the disheartening reality is that our approach to the treatment of nightmares is limited by the fact that we have no objective tools [like a brain scan] to assess their extent and severity. In addition, it’s more apparent that nightmares are not experienced alike. They are shaped by the traumatic events and underlying behavioral and medical conditions of each person.
You say there’s no single strategy that holds the most promise for alleviating nightmares in people with PTSD. Why is that?

VA Researcher Named One of U.S.’ Top Female Scientists

Million Veteran Program director speaks at international forum

2023 VA Women's Health Research Conference

Self-harm is underrecognized in Gulf War Veterans
It’s hard to single out one therapy because the choice of the therapy depends on a patient’s preferences and the availability of expertise to deliver the treatment. We recommend starting with one of the behavioral treatments when a patient has access to a qualified therapist and is willing to commit to that therapy. We also advocate lifestyle modifications that promote good sleep, such as stress relief exercises, an avoidance of alcohol and caffeine, and a refrain from using electronic media close to bedtime. A drug can also be prescribed. In order to promote adherence to medications, we go over the expectations intended from the patient and discuss potential side effects. Frequent monitoring following completion of any therapy is key to assessing whether a satisfactory response has been achieved or whether another treatment should be used.
Such complementary techniques as acupuncture, herbal medicine, yoga, massage, and support groups have been described as other potential therapies for treating nightmares. However, these reports are anecdotal and included a limited number of participants. Nonetheless, patients are encouraged to pursue complementary therapies if they alleviate nightmares.
Your review notes that imagery rehearsal therapy (IRT) is considered the “preferred empiric treatment” for PTSD-related nightmares. What is IRT?
Imagery rehearsal therapy is a behavioral therapy that’s based on the premise that nightmares can be altered through daytime rehearsal of dreams. In other words, the script of a reoccurring nightmare can be modified into a new scenario with a non-frightening ending. The new script is rehearsed daily and can be practiced in a group or individual format. In contrast to medication, imagery rehearsal therapy has been shown in randomized controlled trials to ease the anxiety emanating from nightmares. The beneficial effect can last for more than 12 months and unlike drugs used for nightmares, IRT has no side effects. Other behavioral therapies for nightmares like systematic desensitization and exposure, relaxation, and rescripting therapy have been as effective as IRT. But head-to-head comparisons between those treatments are rare. The choice of the behavioral therapy depends on the doctor’s expertise, the willingness of the patient to return for follow-up visits, and the patient’s ability to cope with the stressful response that may result from recalling distressing events.
In terms of drugs, the alpha-1 blocker prazosin has been widely used in VA to help ease PTSD nightmares. But a large clinical trial sponsored by VA’s Cooperative Studies Program (CSP) found that prazosin did no better than placebo, although the researchers did say the drug worked better in a certain subgroup of patients. Is prazosin still the most promising drug for treating PTSD-related nightmares?
The failure of prazosin in the CSP trial makes behavioral therapy the treatment of choice for this disorder. But the inability of prazosin to improve sleep-related problems in the trial may not be surprising, given that PTSD produces many symptoms that may be only partially responsive to treatment. Our approach has been to continue prazosin in Veterans who have experienced improvement or resolution from nightmares, while discontinuing it in those who have not benefited from it.
I should add that combining drugs with a behavioral therapy for treating PTSD-related nightmares is an area of active investigation. While preliminary data suggest that this approach may be beneficial, large randomized controlled trials are needed to confirm these observations.
You say in the review that given the “intricate relationship between PTSD and nightmares,” future clinical trials must adopt a more pragmatic approach focused on therapies linked to one’s socioeconomic background. What do you mean by that?
Most clinical studies have been designed to compare one therapy versus a placebo, or one treatment versus another treatment, irrespective of the nature of the event responsible for triggering the nightmares. As a result, these studies have often been inconclusive or not reproducible when used to address the nightmares of another Veteran. We’ve proposed that future studies should include a combination of existing treatments targeted to specific groups with similar backgrounds or experiences. In the absence of an objective test to measure and quantify these events, any reported improvement can’t be applied to another case.
There has also been a lack of large randomized controlled trials to assess health outcomes in patients with PTSD who are experiencing nightmares. That’s because of the difficulty in measuring and assessing nightmares objectively. Current studies must rely on a patient’s response to gauge the effectiveness of a therapy. These responses are influenced by cultural, socioeconomic, and personal factors. Most of these studies are also limited by small sample size.
What hope is there for Veterans coping with this debilitating problem?
Nightmares may fade over time. Although there is nothing to identify patients who’ll respond to treatment or in whom nightmares will resolve themselves, a happy ending is always possible. Keeping a positive attitude may help to ease the intensity of these events. Studies have shown that personality traits, such as optimism and pessimism, can affect many areas of health and well-being. The positive thinking that usually comes with optimism, for example, is a key part of managing negative emotions related to nightmares.
VA Research Currents archives || Sign up for VA Research updates