Office of Research & Development |
 |

VA Research Currents archive
April 2, 2015
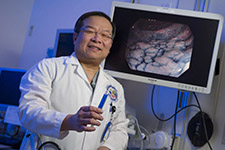
Dr. Roy Soetikno, a gastroenterologist in Palo Alto, was among the VA authors on new international guidelines for surveillance and management of dysplasia in people with inflammatory bowel disease. (Photo by Curt Campbell)
Changes in endoscopic techniques, such as dye-spraying and the use of high-definition colonoscopies, have led to a new set of recommendations on the surveillance and management of dysplasia—areas of pre-cancerous cells—in patients with inflammatory bowel disease.
The guidelines, published jointly by the American Gastroenterological Association and the American Society for Gastrointestinal Endoscopy, focus less on random biopsies to find potential trouble spots and more on using the available technology to identify and remove these precancerous areas before cancer can develop.
Inflammatory bowel disease, or IBD, puts patients at a markedly increased risk of developing colorectal cancer. IBD includes mainly ulcerative colitis and Crohn's disease.
The authors, among them researchers from three VA sites, hope the recommendations lead to improved management, and potentially less need for surgery, in patients with IBD. Joining the U.S. authors were gastroenterologists from Canada and the United Kingdom.
Dysplasia is an area or growth of abnormal cells in the colon that can, and often does, lead to colorectal cancer. If a growth, or polyp, in the colon looks cancerous, then it would be described as having high-grade or severe dysplasia. On the other hand, a polyp that does not appear cancerous would have low-grade or mild dysplasia.
Currently, patients with IBD for at least 8 years are encouraged to have regular surveillance of their colon to reduce the risk of colorectal cancer. This surveillance has entailed colonoscopy about every one to two years, with at least 32 random biopsy specimens taken from throughout the colon.
"Historically physicians were doing these procedures with equipment that wasn't providing the highest image quality. That led to them just randomly taking samples," says Dr. Tonya Kaltenbach, a gastroenterologist at the VA Palo Alto Health Care System, who was part of the group that developed the new guidelines.
"As technology has improved, we've been able to see more of the dysplasia. We can see what it looks like, and now when we do procedures on these patients we know what we're looking for," says Kaltenbach. "The technology, the tools, and our eyes have all gotten better."
While not mandated, the recommendations are meant to serve as guidelines for how providers worldwide identify and manage dysplasia in high-risk patients. The authors say that if followed, the recommendations should increase identification of pre-cancerous dysplastic areas and ideally decrease the number of patients who develop colorectal cancer or require removal of their colon.
The suggestions were developed by an international team of doctors, researchers, and other stakeholders who pooled their collective resources. Think of them as a "dream team" of gastroenterologists.
"The idea was to bring together people from around the world— experts in endoscopy, experts in inflammatory bowel disease, experts in the evaluation of evidence-based medicine, patient representatives, nurses, surgeons and more," says Dr. Kenneth McQuaid, chief of gastroenterology at the San Francisco VA Medical Center. "We wanted to bring them together to discuss the available evidence as well as the controversies and to look at where we could come to agreement on new recommendations so that physicians in the field could move forward with evidence-based guidelines."
In all, the panel performed 13 separate systematic reviews and reviewed hundreds of studies to come up with nine recommendations to identify how surveillance should be performed and, if discovered, how dysplasia should be managed.
For example, the authors recommended using high-definition systems over standard definition when performing colonoscopies, and chromoendoscopy over white light whenever possible. Chromoendoscopy involves applying special dyes that enhance contrast and allow physicians to better spot any abnormalities.
When it came to managing dysplasia, the authors recommended removing dysplastic lesions during colonoscopy whenever possible, and then continuing to monitor via endoscopy for other areas of dysplasia.
"Our goal of course is to try to save lives and to optimize quality of life. If we can identify these lesions early enough and remove them endoscopically, then we can improve quality of life for these patients dramatically," says McQuaid. "The need for surgical treatment with total colectomy [removal of the entire colon] hopefully will also decrease with incorporation of these recommendations in clinical practice."
The authors say there's also an economic benefit to the new guidelines. "There certainly is a cost-saving aspect to it. There are real costs involved in everything from biopsies to colectomies," says Dr. Loren Laine, a research health scientist at VA's Connecticut Healthcare System and a professor at the Yale School of Medicine.
But the real difference, say the authors, is that by following these guidelines, providers can discover and root out dysplasia before it turns to cancer. That kind of increased efficiency can lead to more, and potentially better options for patients facing a life-altering decision.
"Even when a patient is told they have dysplasia and that they have a 60 or 70 percent chance of developing cancer, on average they still won't opt for a colectomy, at least not right away," says Laine. "They want to avoid the procedure, and consideration of patient preferences has to be important in judgments and in decisions on patient care and management."
Though they say more research is needed and that endoscopists and providers probably need further training on chromo endoscopy and identification of subtle areas of dysplasia, the authors believe the new guidelines are an important step toward improving care and quality of life for those patients at risk of developing colorectal cancer.