Office of Research & Development |
 |


VA has participated in or will participate in phase 3, double-blind, placebo-controlled trials for COVID-19 vaccines produced by at least five pharmaceutical companies. (Photo for illustrative purposes only: ©iStock/Geber86)
November 25, 2020
By Mike Richman
VA Research Communications
"We appreciate that not everyone wants to participate, nor should they if they have certain health conditions."
Surveys have shown that a large percentage of Americans are skeptical about the COVID-19 vaccines and therapeutics that are being tested in clinical trials. Many believe the drugs under analysis in Operation Warp Speed, the public-private partnership to facilitate and accelerate the development of COVID-19 vaccines, therapeutics, and diagnostics, are not undergoing enough scrutiny.
Engine, a media and marketing services company, reported in September that only 27% of the respondents to its surveys said they would get a COVID-19 vaccine as soon as it’s ready. The company found that 77% of Americans would eventually get a vaccine, but that half plan to wait for more research and safety data before doing so.

VA center training the next generation of researchers in blood clots and inflammation

AI to Maximize Treatment for Veterans with Head and Neck Cancer

VA researcher works to improve antibiotic prescribing for Veterans
VA’s Million Veteran Program played crucial role in nation’s response to COVID-19 pandemic
Efforts are underway around the world to find a vaccine for COVID-19. According to The New York Times, scientists are testing 52 vaccines in clinical trials in people, and at least 87 preclinical vaccines are under active investigation in animals.
Thus far, VA has participated in or will participate in phase 3, double-blind, placebo-controlled trials for COVID-19 vaccines produced by at least five pharmaceutical companies. VA Greater Los Angeles took part in the Moderna trial and the VA medical center in Cleveland took part in the Pfizer trial. Both of those trials are closed to new volunteers. Earlier this month, Pfizer found in preliminary data that its vaccine was more than 90% effective in preventing COVID-19 within seven days after getting a second dose. Moderna announced based on interim results that its candidate was 94.5% effective within two weeks after receiving a second dose.
Currently, VA is enrolling participants at 17 VA medical centers for the Janssen/ENSEMBLE trial, and recruitment is underway for the AstraZeneca trial at VA New York Harbor. VA is also preparing to recruit participants for the Novavax and Sanofi studies before the end of the year. VA Ann Arbor in Michigan and the Miami VA have been identified for the Novavax trial, and the Bay Pines VA in Florida has been selected for the Sanofi trial.
Recently, nine U.S. pharmaceutical companies, including Moderna, Pfizer, AstraZeneca, Novavax, and Sanofi took steps to allay fears among a jittery public by pledging not to seek FDA approval or Emergency Use Authorization for potential vaccines without conclusive positive data.
For VA’s perspective on the integrity and other aspects of the COVID-19 vaccine trials, VA Research Currents spoke with Dr. Molly Klote, the director of the Office of Research Protections, Policy, and Education in VA’s Office of Research and Development.
VA Research Currents: Vaccines normally require years of research and testing before reaching the clinical stage. What’s your response to the belief that COVID-19 vaccines are being pushed through the system too quickly?
Klote: It’s unfortunate that the public has that perception. There’s no evidence that the science or the process in the U.S. approval system is being shortcut in any way. One reason the process is going faster than many experts anticipated is that we are using different technologies than what we used to develop vaccines in the past. Take, for instance, the flu vaccine. More than 80% of flu vaccines require an egg for the vaccine to be developed. It’s estimated that we may have used 140 million eggs this flu season alone. The process in which the virus is grown in the egg takes at least six months to produce a vaccine.
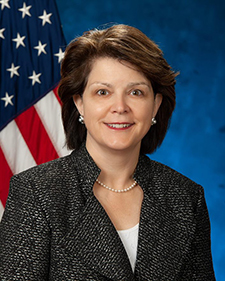
Dr. Molly Klote is the director of the Office of Research Protections, Policy, and Education in VA's Office of Research and Development.
Before the pandemic and as a result of the inefficiencies in the vaccine development process, President Trump issued an executive order to modernize our flu vaccine manufacturing technologies. For the development of COVID-19 vaccines, we’re not relying on the 90-year-old egg-based process. Instead, we’re using new ways to activate the immune system. So mainly because of technology, we’re able to move these vaccines forward so quickly. There’s also no evidence that lower approval standards are being applied to these vaccines, compared with others produced in emergency situations. For all vaccines, the benefits must outweigh the risks.
Some Veterans, like other segments of the population, may be skittish about participating in a vaccine trial. How are you assuring everyone that they are safe?
Research is what is going to stop this pandemic. We appreciate that not everyone wants to participate, nor should they if they have certain health conditions. That’s why all research in the United States is voluntary. Those of us who are dedicated to the protection of humans in research work very hard to make sure that anyone who wants to participate in a study is fully aware of the potential risks and benefits of being a research volunteer.
Studies are designed with criteria on who can participate and who can’t, based on known risks. For instance, in a study where you are testing a certain antibiotic, you would not allow people who are allergic to that antibiotic to participate. Those known risks are written in detailed informed consent documents that are worded at an eighth-grade reading level to make sure the potential known risks are clear and not mixed with medical jargon. We want a fully informed volunteer group so the volunteers can make their own choice to participate based on the provided information. Of course, we don’t know all the risks at the start of a research study. That’s why we closely watch research volunteers during the study. If new risks are identified, the informed consent process gets updated for future volunteers. If necessary, everyone already in the study is alerted.
We absolutely recognize some of the long-standing fears that exist because of the history of abuses in clinical research in the U.S. and around the world. The name “Tuskegee” says it all. [In the Tuskegee Syphilis Study, which began in 1932, U.S. government health workers were found to have carried out unethical and harmful experiments on 600 African-American men who were tested for a treatment to syphilis.] We hold our researchers and institutions to a high ethical standard that includes ongoing oversight, both locally and nationally. If there’s a signal that something is going wrong in a study, we look closely, pause, and make sure we are not causing harm. All adverse events are reviewed by the study teams and, when necessary, reported to the oversight boards. All volunteers receive care for adverse reactions that require care.
However, information about how the research community has set tough standards to safeguard against abuses and about its commitment to care for study participants doesn’t always make it into the communities that have been harmed in the past. There are deep-rooted fears that we must slowly overcome through ethical and respectful behavior by our scientific community. There’s no hidden agenda in these vaccine trials. Our goal is to find a safe and effective vaccine for the greatest number of people to bring an end to this pandemic.
What research protections are in place to mitigate bias and ensure integrity in these vaccine trials?
To mitigate bias, investigators are required to disclose any financial or personal conflicts of interest that may cloud their judgement when conducting a trial. In VA, the Office of General Counsel – Ethics, reviews all disclosures of conflicts of interest and develops a plan to eliminate conflicts, if they exist.
To ensure integrity, the conflict of interest issue is important. We also look toward the study design itself. Will what the researchers are proposing get them to the endpoints that are required to prove their findings? This is where statisticians become very important in the research design. Statisticians calculate how many people a study needs to have enough of the events you are studying to know if it works. For the vaccine trials, the “events” are COVID-19 infections by natural exposure. We want to be clear that these are not challenge trials. We’re not exposing people to COVID-19 after we vaccinate them. We encourage volunteers in these trials to take all the precautions that are recommended by federal, state, and local health authorities. We know that people do get exposed, even if they are careful. Those odds are being calculated into the vaccine trial design.
To further support the study integrity, the research teams go through extensive training with the study sponsors to make sure they understand the research and know how to handle the vaccine and report all data so effective oversight of the trial is possible. Teams of study overseers keep an eye on the daily reporting, looking for signals that anything might be going wrong. The volunteers also are trained on how to report symptoms they are having. Since these studies are double-blinded, meaning neither the researcher nor the volunteer knows if they received the vaccine or the placebo [a salt-water injection], that also helps to keep the reporting free from bias and contributes to integrity.
If the volunteers are having and reporting symptoms, since they don’t know if they received the vaccine or not, they won’t be able to downplay the symptoms by thinking, `Oh, I know I got the vaccine, so these symptoms must not be COVID-19.’ They are more likely to report everything. That process helps with the integrity of the data coming forward because people are keeping electronic study diaries and reporting, `Do I have a fever, or do I have any symptoms?’ They’re keeping daily diaries of what’s going on while they are being watched during the trial. It’s also the job of the data safety monitoring board, a group of scientists who have no personal or financial stake in the outcome of the study, to look at the data and make recommendations on whether to stop the trial due to the number or severity of adverse events.
Finally, the FDA’s research review process that takes place after the initial trial data are ready for review adds to the integrity of the trials. The FDA will review the trial outcome data when the vaccine sponsor presents the data. A panel of FDA experts weighs in on the data.
I understand VA wants to make sure minorities, namely African Americans, Hispanics, and Native Americans, are well represented in these vaccine trials. Is that because a large percentage of people in these demographics have been susceptible to coronavirus?
There’s no question that our populations of color have been more affected by the virus. Essentially, there are two reasons we want to have people of diverse racial and ethnic backgrounds participate in these trials. If they take part in a trial, people in their families and communities are more likely to accept the fact that a vaccine will work if the FDA approves it. If you conduct a study on only white men and say to a diverse community, `Hey, this is going to work for you,’ no one is going to believe you. The other reason we need different ages, genders, races, and ethnicities is because of differences in immune responses and genetic variations. We know men’s and women’s immune systems respond differently to vaccines. We know age affects the immune system. We need a wide range of participants to see if there are differences in effectiveness. It’s also better for the overall safety profile of the vaccine. If there’s going to be a problem in any segment of our population, we want to know that now, not after the vaccine gets FDA-approved.
Is VA recruiting only Veterans for these clinical trials?
All VA medical centers can recruit anyone into these trials, if they choose to recruit beyond the Veteran population. If the VA site recruits people who are not eligible for care at VA, some extra steps come into play. The medical center must create a medical record and provide VA’s notice of privacy practices to the people who are not eligible for care. VA hospitals also need to care for the people in the trial if there is a research-related injury. That’s why some medical centers may not be able to open the studies to a broader population. VA hospitals must consider the impact of the study activities on the care we continue to give to our Veterans. VA has agreements with the vaccine companies that require reimbursement to VA for any care that a study participant receives for a research-related injury in one of the VA COVID vaccine trials. We are not spending, without reimbursement, VA health care dollars that are allocated by Congress for the care of our Veterans for non-Veteran care in these studies.
How effective do you think a COVID-19 vaccine could be?
Pfizer released very exciting preliminary data from its study of 44,000 people who received the vaccine. Moderna followed right behind with interim results from its 30,000 volunteers showing great effectiveness and safety. Once the FDA reviews the companies’ safety and effectiveness data, it may issue an Emergency Use Authorization [EUA] to one or both companies. A EUA would allow the vaccines to start to be given outside of a research study. But the granting of a EUA does not mean we stop doing research on other vaccine candidates by other companies. We still need more vaccine trials to go on and more people to volunteer. Each vaccine manipulates the immune system in slightly different ways. In addition, some vaccines require only one vaccination to be effective, and some like Pfizer and Moderna require the initial vaccination and a booster shot a few weeks later. The different vaccines also require storage at varying temperatures, including some at minus-70 degrees Fahrenheit. These factors make the delivery of some vaccines harder than others.
We’re trying to protect at least 50% of the people who are vaccinated from getting seriously ill. That’s the FDA effectiveness cutoff. You must show at least 50% effectiveness. People say, `Oh my gosh, 50% doesn’t seem very high.’ But when you look at the flu vaccine, we measure effectiveness based on how many people who get the flu avoid having to be hospitalized. The overall range of effectiveness has been 19% to 60% over the past 10 years. When you consider other vaccines we have tried to develop, we’ve never gone above 32% effectiveness with the HIV vaccine, which is why one has never been approved. It’s not easy to get to 50%. There’s no guarantee you are going to get to 50% effectiveness when you start a vaccine trial. That’s why the Pfizer and Moderna preliminary data, which are pending confirmation, are so exciting.
We would love to have several COVID-19 vaccines that are more effective than 50%. It seems that two are already showing promise. We’ll continue to search for differences in effectiveness in different populations. We want to make sure our most vulnerable citizens are protected. That’s why we do the research. That’s why we need volunteers.
VA Research Currents archives || Sign up for VA Research updates