Office of Research & Development |
 |


Hundreds of VA clinics nationwide now integrate mental health care with primary care, making it easier for Veterans to get services to address depression, anxiety, and other conditions. (Photo: ©iStock/FatCamera)
March 28, 2018
By Mike Richman
VA Research Communications
About 30 percent of VA patients using primary care providers have a diagnosed mental health disorder, and many others have undiagnosed conditions. Improving access for these Veterans to mental health services is one of the agency’s top priorities.
To that end, the agency launched the Primary Care-Mental Health Integration (PC-MHI) program in 2007. The initiative aims to increase access to mental health specialty care for primary care patients and, in turn, lessen the need for potentially time-consuming referrals to non-primary care mental health services. It calls for embedding psychologists and other specialists in primary care to address common mental health needs, with depression, anxiety, and alcohol abuse being the target conditions.

Dr. Lucinda Leung is a physician and health services researcher at the VA Greater Los Angeles Healthcare System. (Photo by Scott Hathaway)
The PC-MHI model is now in place at hundreds of VA clinics nationwide.
Dr. Lucinda Leung, a physician and health services researcher at the VA Greater Los Angeles Healthcare System, led two studies to learn if PC-MHI is working. She and her team gathered evidence showing that the program is improving Veteran access to mental health care as intended.
“As a primary care provider at VA, I see many patients struggling with mental health and physical health problems,” Leung says. “It’s difficult to lower my patient’s blood pressure if that person is too depressed to take medication and care for himself or herself. Bringing mental health care directly to primary care patients is key to engaging them, since many Veterans do not easily ask for help.”
She says VA primary care providers have traditionally needed to refer patients to mental health specialists. But many primary care clinics using PC-MHI care have lifted the need for such referrals, she adds.
“Often under PC-MHI, primary care providers can simply walk down the hall and `hand off’ a patient to a mental health provider on the same day,” she says.
PC-MHI consists of a team of mental health experts, mainly psychologists, social workers, licensed mental health counselors, and care managers who are often nurses. VA requires its hospitals and community-based outpatient clinics (CBOCs)—primary care sites that serve as satellite clinics for large VA campuses—to have a full-time PC-MHI staff on site if they see more than 10,000 patients a year. CBOCs that see 5,000 to 10,000 Veterans a year must use some version of PC-MHI on a part-time basis.
"Bringing mental health care directly to primary care patients is key to engaging them, since many Veterans do not easily ask for help."
Currently, more than 300 VA clinics—both at medical centers and at CBOCs that meet the full-time and part-time criteria—are required to have PC-MHI services. But Leung says more have probably implemented some variation of the program. All but two of the 29 VA facilities that were part of her two studies reported using PC-MHI to some extent, but only a third are required to do so, she says. Those 29 sites are in a southwest VA administrative region (Veterans Integrated Service Network, or VISN, 22).
Both of her studies included the same cohort: nearly 67,000 primary care patients with mental illness who were treated at the 29 sites from 2008 to 2013. Of the patients, 35 percent had depression, 36 percent had anxiety, and 22 percent had PTSD.

Dr. Jay Gorman
Suicide prevention care

VA Researcher Named One of U.S.’ Top Female Scientists

Million Veteran Program director speaks at international forum
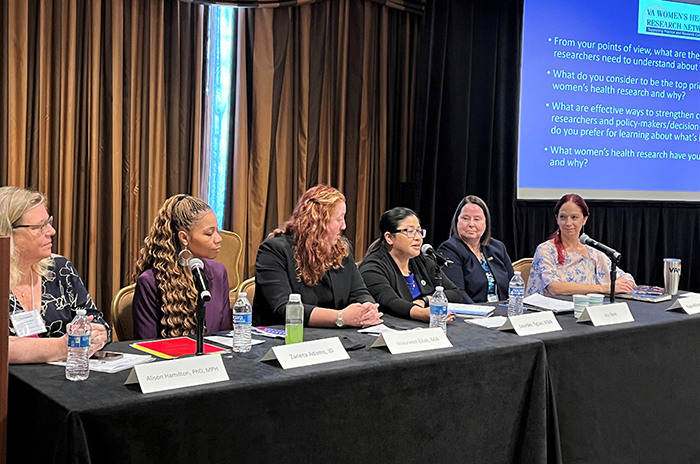
2023 VA Women's Health Research Conference
One of the studies appeared in Psychiatric Services in December 2017. The researchers concluded that primary care clinics with greater use of PC-MHI showed less reliance on non-primary care-based mental health specialty (MHS) services for patients with depression. The same clinics did not show declines in mental health specialty visits for conditions such as schizophrenia and bipolar disorder.
In addition, for every 1 percent increase in the share of primary care patients who received PC-MHI services, patients at the same clinic had 1.2 percent fewer general mental health specialty visits per year. There was no drop in more specialized MHS visits.
The latter are services “I would not expect PC-MHI to replace,” Leung says. “These are PTSD services and other services for patients with serious mental conditions.”
In terms of why MHS use was down for depression, Leung explains: “For these `bread and butter’ often less-complicated mental health problems, PC-MHI providers assist primary care providers with managing the problem directly in a primary care clinic. These conditions usually resolve after short-term therapy or medication. If the mental health condition worsens, the patient will then transition from PC-MHI to mental health specialty care for more intensive services.”
She adds: “Psychotic disorders, like schizophrenia and bipolar disorder, are generally lifelong conditions. They are often complex and require wraparound service from a large team of mental health specialists. Primary care is not as well-equipped to care for patients with serious mental illness, so we want to ensure that these patients are plugged in with the right specialists for help. PTSD usually falls somewhere in the middle, and there are a lot of good specialty programs dedicated to treat this condition in VA.”
Leung’s other study appeared in the Journal of the American Board of Family Medicine in the January-February 2018 issue. It examines whether increasing primary care clinic engagement in PC-MHI services is linked to changes in patient health care use and costs.
The researchers found that the median share of primary care patients who received PC-MHI services at the 29 facilities increased by 8.2 percent from 2008 to 2013. Also, 1.5 PC-MHI visits substituted for each non-primary care-based MHS visit, without raising total costs by a significant margin, according to the statistical methods used in the study.
“If you build it, they will come,” Leung says of the 8.2 percent figure “If you bring mental health care directly to patients in need, they are probably more likely to use it. Clinics are using PC-MHI more and more. Just imagine the hurdles related to going to a different floor, building, or city to receive mental health care for a condition like depression. That’s a lot to require of some Veterans.”
Today, integrated mental health care is a major trend in VA. Leung notes, in particular, that VA has pushed hard for PC-MHI care to be available to Veterans. The agency has invested many resources to support the program, namely by hiring more psychologists and other mental health experts to work in primary care, she says.
PC-MHI seems easier to implement in an integrated health care system like VA, compared with non-VA medical facilities, Leung says.
“Large integrated health systems, such as VA, Kaiser Permanente, and Intermountain Healthcare, have been champions for collaborative care services like PC-MHI,” she says. “These systems have good programs for communication and monitoring, less reimbursement issues for collaborative care services, and other strong elements of health care integration. Other systems are beginning to realize the benefits of investment in collaborative care, so more and more are doing it. However, they may face additional hurdles because their care delivery and financial incentives may not be aligned the same way as VA.”
Although it has become clearer to her that more and more VA facilities are using PC-MHI, Leung believes more research is needed to understand the quality of services provided in integrated mental health care.
“Better access to care does not always mean better quality care,” she says. “Understanding how PC-MHI is linked to the quality of depression care, for instance, is my next research project.”
VA Research Currents archives || Sign up for VA Research updates